Dentists Journal
All Time Top Stories
All Dentists Journal · Top Ten Weekly · Headlines

Hemangioma of the lip a purple spot on the lip
Lip Hemangiomas. This common lip discoloration is often caused by minor trauma such as that occurring at a dentist office, or even just biting your lip.
But there are various potential causes of a purple spot on your lip. Some of them are benign (not threatening to your health), while others could be signs of something more serious. The following list of conditions could help you narrow down what's behind the discoloration you're experiencing, but be careful not to self-diagnose – a healthcare professional is best-suited to diagnose and treat your condition. Some of the most common causes of a purple spot on the lip include:
A broken blood vessel, blood blister, or bruise

The purple spot on your lip could be the result of an impact, or perhaps you bit your lip, causing it to bruise. If you have a bruise on your lip, your purple spot should go away in a matter of days. If it doesn't, the condition could be something else. Contact your healthcare professional for an appointment.
Venous Lake

A venous lake is the swelling of a vein under your skin, tends to affect the elderly, and can show on your lip, ears, or face.
The cause is unknown, but it's believed to be associated with sun exposure. According to the American Osteopathic College of Dermatology, venous lakes are benign and don't cause pain or other symptoms. Treatment is typically for cosmetic purposes and includes light electrocautery, laser ablation, liquid nitrogen cryosurgery, or, more rarely, surgical removal.
Allergic Reaction
Certain foods, lipstick or chapstick, or another item that you're allergic to could have come into contact with your lip, causing it to turn purple. In most cases, an allergic reaction will go away on its own. If you're experiencing other symptoms like difficulty breathing or swallowing, get immediate medical attention.
Lip Cancer
According to Memorial Sloan Kettering Cancer Center, lip cancer is the most common oral cancer. Tobacco products, excessive alcohol consumption, and sun exposure all increase your chances of getting lip cancer. If you think you may have lip cancer, visit your healthcare professional for diagnosis and treatment right away. Catching this disease early increases your likelihood for successful treatment, whether your doctor recommends surgery or radiation.
If you've noticed a dark spot on your lip, or any other changes to the skin on your lips, it's always a good idea to see your healthcare professional for diagnosis. It may be a benign condition that will go away on its own, but if it's something more serious, you'll be happy to catch it early so you can begin treatment right away.
(05/25/2021)by Essence Medispa
More Information: https://www.essencemedispa.com/blog/hemangioma-of-the-lip-purple-spot-on-the-lip
Views: 5,151

What Causes a Dark Spot on Gums?
Amalgam Tattoo
An amalgam “tattoo” occurs when a silver filling is being placed and some of the metal filling material inadvertently becomes lodged in the gum tissue or cheek. It usually looks like a small, irregularly shaped dark blue discoloration. They may look strange when you brush your teeth, but these dots are perfectly harmless and require no treatment.

Gum Injuries
Trauma, such as accidentally biting your tongue or cheek or being hit in the mouth while playing sports, can leave a bruise, appearing as a dark spot on the gum or cheek. You would most likely be aware of this happening and can easily relate the bruise to a specific injury. This type of injury will usually heal by itself in a week or two and requires little treatment beyond palliative care, such as rinsing with warm salt water.

For any lesion that is more severe or doesn’t seem to be healing, you should see your dentist. You should also always wear amouth guard to protect your teeth while playing contact sports.
Minor oral injuries, such as a cut from sharp food, can sometimes result in a pyogenic granuloma, a bright red or purple swollen bump. This overgrowth of tissue can also appear in the mouth during pregnancy. If they are bothersome, granulomas can be easily removed, and they are not malignant or dangerous.
Dark Gum Spots & Teething
Occasionally, a swollen spot known as an eruption hematoma can form over a child’s erupting tooth. When this small, fluid-filled cyst contains blood it appears dark blue or purple. The word “hematoma” refers to an area filled with blood, just like any bruise you might get from bumping your knee or elbow. This is a harmless lesion that requires no treatment and will disappear as the tooth grows into the mouth.
Rare Conditions
In rarer cases a dark spot on gum tissue can point to a disease or growth. A nevus, for example, is a congenital tumor-like malformation of the skin or mucous membrane that can develop in the mouth. It may appear as a dark blue pigmented mole and is typically harmless and requires no treatment.
The circulatory disease thrombocytopenia, characterized by a deficiency in the number of platelets in the blood, can also be marked by oral spots called thrombocytopenic purpura. Other oral symptoms include spontaneous bleeding gums and the appearance of small red dots called petechiae on the roof of the mouth and the cheeks. This condition requires referral to a doctor for accurate diagnosis and treatment.
What to Do About Dark Spots?
Many soft-tissue-related dark spots in the mouth are harmless, and there is no need to remove or disturb them unless they become painful. It’s no secret that your mouth is a reflection of the health of your whole body, so it never hurts to see your dentist if you notice any perplexing oral changes. They will likely already perform a regular oral cancer screening and other checks of your soft tissues at your regular dental cleanings.
If your dentist is uncertain about the cause of a dark spot on gums, they may have you return in a week to see if there are any changes. If there are persistent symptoms or problematic changes in the size, shape, or color of a spot, your dentist may refer you to a doctor or oral surgeon for appropriate followup.
(05/18/2021)by Beddington Dental
More Information: https://beddingtondentalclinic.com/what-causes-a-dark-spot-on-gums/
Views: 4,850

Dentistry as one of the oldest medical professions
Dentistry is one of the oldest medical professions, dating back to 7000 B.C. with the Indus Valley Civilization. However, it wasn’t until 5000 B.C. that descriptions related to dentistry and tooth decay were available. At the time, a Sumerian text described tooth worms as causing dental decay, an idea that wasn’t proven false until the 1700s!
In ancient Greece, Hippocrates and Aristotle wrote about dentistry, specifically about treating decaying teeth, but it wasn’t until 1530 that the first book entirely devoted to dentistry—The Little Medicinal Book for All Kinds of Diseases and Infirmities of the Teeth—was published.

By the 1700s, dentistry had become a more defined profession. In 1723, Pierre Fauchard, a French surgeon credited as the Father of Modern Dentistry, published his influential book, The Surgeon Dentist, a Treatise on Teeth, which for the first time defined a comprehensive system for caring for and treating teeth. Additionally, Fauchard first introduced the idea of dental fillings and the use of dental prosthesis, and he identified that acids from sugar led to tooth decay.
In 1840, the first dental college (Baltimore College of Dental Surgery) opened, establishing the need for more oversight. In the United States, Alabama led the way by enacting the first dental practice act in 1841, and nearly 20 years later, the American Dental Association (ADA) was formed. The first university-affiliated dental institution, the Harvard University Dental School, was founded in 1867.
By 1873, Colgate had mass produced the first toothpaste, and mass-produced toothbrushes followed a few years later.

What may come as a surprise is that the first African American to earn a dental degree dates all the way back to 1869, and the first female dental assistant was employed in New Orleans in 1885. What might be most surprising of all is that most Americans did not adopt good brushing habits until after World War II, when soldiers stationed abroad brought the concept of good oral health back to the United States!
Other Fun Teeth Facts:
-Hesy-Re was an Egyptian scribe who lived around 2600 B.C. and is recognized as the first dental practitioner.
-Paul Revere, famous for warning Colonial troops that the British were coming, was also trained as a dentist by America’s first dentist, John Baker.
-Edward H. Angle, who started the first school of orthodontics in 1901, created a simple classification for crooked teeth in the late 1800s, a system still in use today.
-The first dental X-ray was used in 1896.
(08/03/2020)by ADEA
More Information: https://www.mybestdentists.com/resources/AmericanDentalEducationAssociati
Views: 4,072

Sore throat, causes and symptoms
A sore throat is pain, scratchiness or irritation of the throat that often worsens when you swallow. The most common cause of a sore throat (pharyngitis) is a viral infection, such as a cold or the flu. A sore throat caused by a virus resolves on its own.
Strep throat (streptococcal infection), a less common type of sore throat caused by bacteria, requires treatment with antibiotics to prevent complications. Other less common causes of sore throat might require more complex treatment.
Symptoms:

Symptoms of a sore throat can vary depending on the cause. Signs and symptoms might include:
Pain or a scratchy sensation in the throat
Pain that worsens with swallowing or talking
Difficulty swallowing
Sore, swollen glands in your neck or jaw
Swollen, red tonsils
White patches or pus on your tonsils
A hoarse or muffled voice
Infections causing a sore throat might result in other signs and symptoms, including: Fever, Cough, Runny nose, Sneezing, Body aches, Headache, Nausea or vomiting.
Causes
Viruses that cause the common cold and the flu also cause most sore throats. Less often, bacterial infections cause sore throats.
Viral infections
Viral illnesses that cause a sore throat include:
Common cold
Flu (influenza)
Mono (mononucleosis)
Measles
Chickenpox
Coronavirus disease 2019 (COVID-19)
Croup — a common childhood illness characterized by a harsh, barking cough
Bacterial infections
A number of bacterial infections can cause a sore throat. The most common is Streptococcus pyogenes (group A streptococcus) which causes strep throat.
Prevention
The best way to prevent sore throats is to avoid the germs that cause them and practice good hygiene. Follow these tips and teach your child to do the same:
Wash your hands thoroughly and frequently, especially after using the toilet, before eating, and after sneezing or coughing.
Avoid sharing food, drinking glasses or utensils.
Cough or sneeze into a tissue and throw it away. When necessary, sneeze into your elbow.
Use alcohol-based hand sanitizers as an alternative to washing hands when soap and water aren't available.
Avoid touching public phones or drinking fountains with your mouth.
Regularly clean telephones, TV remotes and computer keyboards with sanitizing cleanser. When you travel, clean phones and remotes in your hotel room.
Avoid close contact with people who are sick.
(11/28/2020)by Mayo Clinic
More Information: https://www.mayoclinic.org/diseases-conditions/sore-throat/symptoms-causes/syc-20351635
Views: 3,804
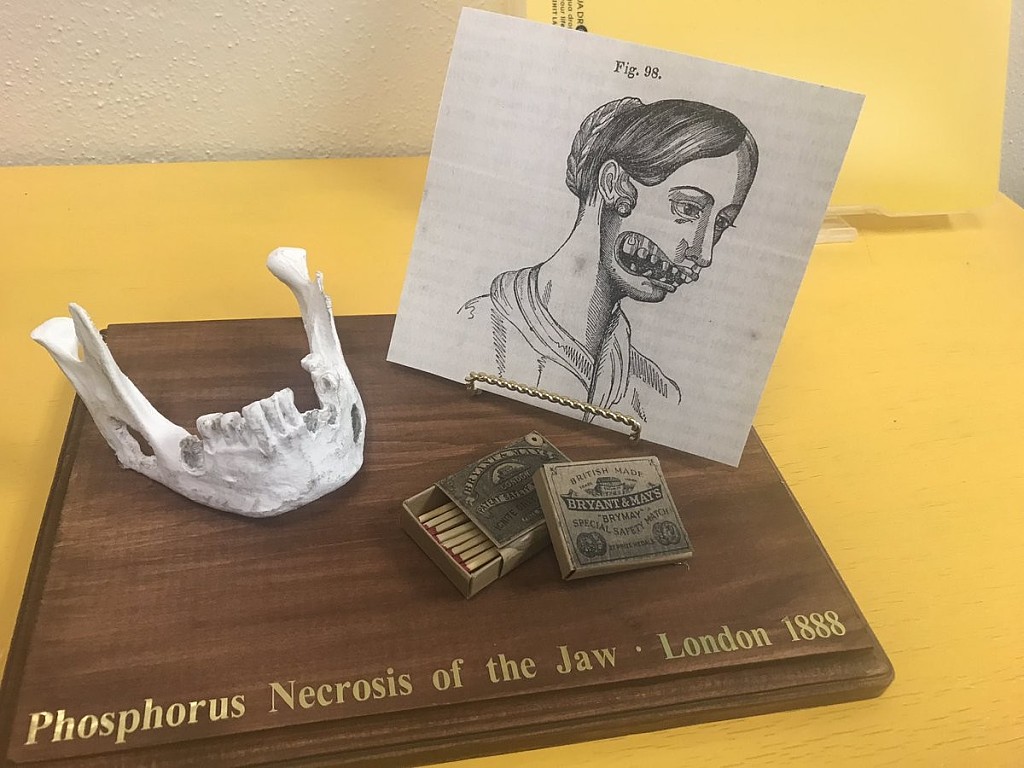
What Is Phossy Jaw?
What do household matches have to do with dental health? A look back in time highlights an interesting historical event — which now seems to be repeating itself. In the 19th century, some workers in match factories developed a condition called phossy jaw after being exposed to a chemical used in the match manufacturing process. This condition, clinically known as osteonecrosis of the jaw, vanished until it recently reappeared in the 21st century.
History of Phossy Jaw
An article in the journal Craniomaxillofacial Trauma & Reconstruction states that this oral disease came about in the 1860s because matchstick factory workers were exposed to dangerous levels of phosphorous — a chemical used for creating matchsticks. Inhaling the phosphorous fumes resulted in a rise in the incidence of gum disease, bone deterioration and bone cell death that was termed phossy jaw.
Beyond the oral effects of this condition, these workers also experienced respiratory symptoms such as coughing, drainage and bloody discharge from the lungs that was termed phossy lung. They also experienced seizure conditions called phossy brain and blood conditions known as phossy marrow. These toxic responses were all eventually traced back to the matchstick factories, and the condition soon disappeared among the population after alternative factory materials were introduced in 1906.
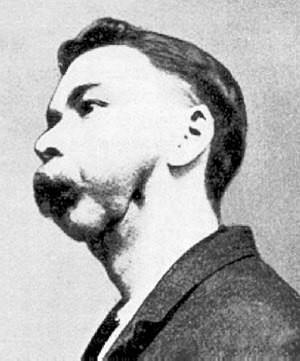
Modern-Day Phossy Jaw
To understand why cases similar to phossy jaw have returned, you'll first need to understand how bisphosphonates work. As Johns Hopkins Medicine explains, doctors often prescribe bisphosphonate medications to patients with systemic diseases such as osteoporosis, which is a condition that weakens the bones. These medications prevent and treat bone thinning in individuals who are diagnosed with osteoporosis, lupus or other bone-weakening conditions. Bisphosphonates work by slowing the process by which the body dissolves certain bone-building minerals.
Despite this medication's positive effects, one possible side effect of using bisphosphonate drugs is bisphosphonate-induced osteonecrosis of the jaw (ONJ), which is very similar to phossy jaw. The American College of Rheumatology (ACR) describes ONJ as a condition where the jawbone becomes exposed and doesn't get enough blood, so it begins to weaken and die, often causing pain. An individual who is taking or has previously taken bisphosphonate medication is at a greater risk for ONJ, and it most commonly occurs following dental extractions.

It's common for dental professionals to advise patients who need extractions to discontinue the use of bisphosphonate drugs and take an antibiotic prior to the procedure, explains Johns Hopkins Medicine. This is because, while bisphosphonates are used to prevent bone thinning, they can interfere with jawbone healing, especially after dental work.
Bisphosphonate-induced ONJ is rare, as the National Osteoporosis Foundation notes. But ONJ can also occur in individuals who have not taken bisphosphonate drugs. Other risk factors for ONJ include radiation treatment, infection and steroid use.
Treating and Preventing Osteonecrosis of the Jaw
The ACR says that patients who have taken bisphosphonates or are currently taking them should inform their dental provider of their medication history prior to any dental care. This allows the dental provider to take precautions should a surgical procedure be necessary — especially in cases of tooth removal. If an individual does develop ONJ, their dental professional will likely recommend antibiotics, oral analgesics and mouthrinses, which are often effective.
Both dentists and oral and maxillofacial surgeons know how to identify the risk factors associated with using bisphosphonate medications, thanks to their dental school education and extensive training. When you keep your dental professionals informed about your medication use, they can plan their approach accordingly to help prevent ONJ and other healing complexities following dental treatment.
(03/18/2021)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/threats-to-dental-health/what-is-phossy-jaw
Views: 3,755

Invisalign is the Invisible Way to Straighten Teeth
For many years, orthodontic treatment required wearing bulky, uncomfortable metal braces and wires. The shame and embarrassment of sporting these bulky metal braces prevented many people from seeking the beautifully straight smile they desired.
Invisalign was created for the patient that wants straighter teeth without wearing visible, uncomfortable metal braces. Invisalign patients wear a series of clear, plastic aligners that gradually shift teeth into the desired position and alignment. Because of the nature of the aligners, patients can maintain a normal looking smile while simultaneously straightening their teeth.
What Invisalign Can Correct

Invisalign corrects cases of minor tooth misalignment or poor spacing, where the problem is mostly cosmetic. This includes small spaces between the teeth, crowding of the teeth, an overbite (i.e., the upper teeth bite over the lower teeth), and a crossbite (i.e., the upper and lower jaws are misaligned).
Patients that have substantial structural issues with the teeth or problems with the bite are typically better suited for traditional braces or another orthodontic alternative.
Advantages of the Invisalign System
There are many reasons why patients prefer Invisalign to traditional braces, including the following:
Aligners fit comfortably and don’t irritate the inside of the mouth
Aligners don’t disrupt speech
Aligners can be removed to eat so patients can enjoy all of their favorite foods
Aligners are inconspicuous and virtually undetectable in the mouth
Total treatment time is usually shorter than other orthodontic treatments
Treatment Details
Invisalign aligners are custom-fabricated to the exact specifications of the patient. No two treatment plans are precisely alike.
The first step to of Invisalign treatment is to capture information about the teeth’s current position. The dentist takes photographs and digital impressions that are used to create a three-dimensional “map” of the teeth’s planned movement. The map charts the teeth’s original position through Invisalign treatment to their final position. This information is then sent to the dental laboratory that constructs the series of customized aligners.
The patient receives their first set of upper and lower aligners and should wear them for 20 to 22 hours per day (removing them to eat and clean). The aligners put gentle pressure on the teeth to move them into the correct alignment and position. Patients may have a slight adjustment period, getting used to the way the aligners feel, but they usually don’t experience discomfort. They can eat, speak and smile normally while wearing the aligners.
After two to four weeks, that set of aligners is swapped out for the next set in the series. This repeats until the teeth have shifted into the desired position and alignment.
Invisalign patients are supervised by a dentist throughout treatment. The dentist periodically checks the progress of treatment and examines the teeth and bite for any potential problems.
Total treatment time varies by patient, but many Invisalign patients are able to complete treatment in less than a year.
At Dental Health Associates in Sylvania Ohio, our dentists are thoroughly trained and extensively experienced with Invisalign treatment. We enjoy helping our patients transform their smiles easily and comfortably!
(07/28/2020)by Andrew Marshall Huntzinger
More Information: https://www.mybestdentists.com/AndrewMarshallHuntzinger
Views: 3,685
Dr. Zachary Potts goal is to change his patient's outlook by making every experience positive, comfortable and rewarding
Dr Zachary Potts is committed to not only providing the highest quality dental care available but also to erasing the negativity associated with going to the dentist. His goal is to change his patient’s outlook by making every experience at Moorpark Center for Dentistry positive, comfortable, and rewarding.
“They’re happy, they’re smiling, they’re having a good time laughing and opening up. Just seeing that transformation in people after an experience in my unique office is what keeps me loving my career.” – Dr. Potts
Education & Professional Affiliations Loma Linda University School of Dentistry – Graduated first in his class and received the Clinician of the Year award for clinical excellence. American Academy of Cosmetic Dentistry (AACD) American Academy of Implant Dentistry (AAID) Academy of General Dentistry (AGD) American Dental Association (ADA) California Dental Association (CDA) Santa Barbara Ventura County Dental Society Dentistry Development Study Club, president Board-certified in oral conscious sedation
When not providing people in Ventura County with cutting-edge dental care, Dr. Potts enjoys dining, traveling, and spending time with his wife and three children, Jelina, Corbin, and Amelia. He also has two dogs, a cat, and enjoys television, movies, and collecting beer, wine, and fine whiskey. A family man, Dr. Potts prefers spending his time away from work doing things that make his children happy.
(09/21/2020)More Information: https://mybestdentists.com/ZacharyLeroyPotts
Views: 3,642

ADA and others recommend to establish a Dental Home for your child
The American Academy of Pediatrics (AAP), the American Dental Association (ADA), and the American Academy of Pediatric Dentistry (AAPD), recommend to establish a “Dental Home” for your child by around one year of age. Children who have a dental home at younger ages are more likely to receive appropriate preventive and routine oral health care, as well they are more likely to avoid future dental issues and disease. They also learn early to love the dentist and are less apt to have fear and phobias with coming to see us.
The key…EDUCATION! At our NoPo Dental office we know how hard being a parent can be and that teeth and oral hygiene are not always your top focus in the early years. As a pediatric dentist and a mother of two, Doctor Staci and her team are full of tips and tricks to get you dental savvy and to help your child become more cooperative and compliant for oral hygiene routines. We will review daily recommendations with a strong focus on diet, as well as helpful positioning to brush and floss and clever strategies to make all of it fun while you do it!

Parents are allowed to stay with their child at our NoPo Kids Dentistry office for routine cleanings, check-ups and treatment, and whether it is their very first dental visit, or their twentieth, the team at NoPo Kids Dentistry strive daily to create the most positive, loving, upbeat, and motivating appointment for you and your child.
(07/17/2020)by Doctor Staci
More Information: https://www.mybestdentists.com/mbd-newest-approved-dentists/AnastaciaMWhitman
Views: 3,587

What Is Plica Fimbriata?
The underside of your tongue isn't something that you would normally think about if everything is functioning as it should. But just imagine if one morning, as you're eating breakfast, you discover that these folds underneath your tongue are painfully irritated. You may also notice that saliva is pooling in the area. Immediately, you would be concerned about what might be going on. These small folds are called the plica fimbriata, and they are just one of the many structures that make up the tongue and salivary glands.
Structures Under the Tongue
As the ENT Atlas explains, the plica fimbriata is an elevated crest of mucous membrane on the underside of your tongue. Here's a quick anatomy lesson to help you understand the exact location of these folds in your mouth.
Below your tongue is a horseshoe-shaped area of tissue known as the floor of the mouth. This flat area of soft tissue has a separate rising fold of tissue that connects it to the underside of the tongue, known as the lingual frenulum. The plica fimbriata consists of two raised folds that are located on both sides of where the lingual frenulum connects to the tongue, as seen in an illustration from StatPearls.

Plica Fimbriata and Your Salivary System
As a presentation from Semmelweis University outlines, the plica fimbriata is part of the salivary gland system in your mouth. The saliva that is produced near the floor of the mouth comes through the salivary glands and drains under the tongue through the sublingual and submandibular ducts. The plica fimbriata is one location where these ducts open to release saliva in the mouth.
Common Salivary Gland and Duct Issues

The salivary gland and duct system under your tongue can be disturbed by various oral health problems. If a salivary gland gets blocked by a calcified formation, also known as a salivary stone, the area can become painful and swollen, according to Johns Hopkins Medicine. The stones — also called sialolithiasis — occur in the submandibular gland about 80% of the time.
If you think that you have a salivary stone, you should seek immediate care from your physician or dental professional. Sialolithiasis can be diagnosed with an ultrasound or a computerized tomography scan. Oftentimes, applying moist heat and massaging the salivary gland can help to relieve this condition. Anti-inflammatory medications, such as ibuprofen, can also help to reduce the swelling and pain associated with salivary stones.
If these first-line measures do not alleviate the condition, you may require surgery. As the Cleveland Clinic explains, if the stone is located near the surface, your doctor or dentist may be able to remove it in a quick in-office procedure. This would involve using local anesthesia and making a small incision to the area. If the stone is deep in the tissue, your doctor would possibly need to use a technique called salivary sialendoscopy. This involves using a tiny scope to visualize the duct while using a special tool to retrieve the stone. In most cases, patients recover well with no further issues.
Now that you know more about the structures underneath your tongue, you can feel empowered to discuss any issues that develop in this area with your dental professional.
(06/26/2021)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/mouth-and-teeth-anatomy/what-is-the-plica-fimbriata-and-where-is-it-located
Views: 3,574

ADA 'respectfully yet strongly disagrees' with WHO guidance recommending delay of dental care
The American Dental Association released a statement Aug. 12 stating it "respectfully yet strongly disagrees" with the World Health Organization's interim guidance recommending that "routine" dental care be delayed in certain situations because of COVID-19."Oral health is integral to overall health.
Dentistry is essential health care," ADA President Chad P. Gehani said. "Dentistry is essential health care because of its role in evaluating, diagnosing, preventing or treating oral diseases, which can affect systemic health."The ADA Board of Trustees adopted an ad interim policy stating dentistry is essential health care during a video call July 27, and the House of Delegates will consider it as a resolution during its virtual meeting in October.
As U.S. COVID-19 cases began to rise in March, the ADA called for dentists to postpone all but urgent and emergency care in order to understand the disease and consider its effect on dental patients, dental professionals and the greater community, Dr. Gehani said.
Both the ADA and Centers for Disease Control and Prevention then issued interim guidance for dental professionals related to COVID-19, calling for the use of the highest level of personal protective equipment available, such as masks, goggles and face shields.
To minimize aerosols, the ADA guidance also recommended dental professionals use rubber dams and high-velocity suction whenever possible and hand scaling instead of ultrasonic scaling when cleaning teeth.
"Millions of patients have safely visited their dentists in the past few months for the full range of dental services," Dr. Gehani said. "With appropriate PPE, dental care should continue to be delivered during global pandemics or other disaster situations."
(08/13/2020)by Mary Beth Versaci
More Information: https://mybestdentists.com/in-the-news/AmericanDentalAssociation
Views: 3,529

Hidden dental dangers that may threaten your whole body
A growing number of older adults have something to smile about: research shows they're keeping their teeth longer. While that makes chewing and talking easier and staves off malnutrition and the discomfort of dentures or missing teeth, it also means you need to be more vigilant than ever about preventing dental problems — including some that can have life-threatening complications.
Tooth decay

One in five adults ages 65 or older has untreated tooth decay (a cavity). This develops when food and bacteria form plaque that sticks to teeth and produces toxins that break down a tooth's outer layer (enamel).
Bacteria also can infect the root of the tooth and form a small pocket of pus (an abscess). "If the infection doesn't find a way out, it may travel to another space in the head. It wants the path of least resistance, so it may infect the jaw. But it can also travel to the brain and cause death, although this is fortunately rare," warns Dr. Lisa Thompson, a geriatric dentistry specialist at the Harvard School of Dental Medicine.

Gum disease
Two out of three adults ages 65 or older have gum disease (also called periodontal disease). This is inflammation of the gums that can lead to tooth loss and many other problems. The disease starts with plaque buildup that irritates the gums. This early stage (gingivitis) causes swollen gums that bleed easily.
If untreated, gingivitis can extend below the gum line. The body's own immune system is thought to fuel the condition, as white blood cells — called to attack the bacteria — eventually damage gum tissue as well. "It can infect the gums all the way down to the ligament that holds the teeth in the bone, penetrate the ligament, destroy bone, and cause tooth loss and abscesses," Dr. Thompson says. At worst, bacteria from gum disease may get into the bloodstream and infect the heart valves, a potentially deadly complication.
People with gum disease are more likely to have high blood pressure, diabetes, rheumatoid arthritis, osteoporosis, Alzheimer's disease, and pneumonia — although it is not proven that the gum disease actually causes these conditions.
Older adults face increased risks
Maintaining good oral health gets harder as we age. Sometimes that happens because we've suffered declines in other abilities. "You might have arthritis and decreased manual dexterity. That can make it difficult to brush or floss your teeth or properly care for dentures if you have them," says Dr. Thompson.
Another challenge: age-related physical changes in the mouth. The gums start to recede, exposing more of your teeth and creating new spaces that floss doesn't always reach. The teeth become less sensitive as the nerves inside them shrink and a secondary layer of dentin (porous material beneath the enamel) develops.
"You may not feel the same amount of pain in the tooth if there's a problem, and it can progress before you realize it," Dr. Thompson points out. And years of wear and tear can leave your teeth weakened or cracked and vulnerable to dental problems.
Chronic conditions also play a role in oral health. Uncontrolled diabetes can make gum disease worse. And many medications cause dry mouth. "You need saliva — which contains fluoride and electrolytes [like sodium and calcium] and moistens the mouth — to help clean and protect the teeth," Dr. Thompson says. A lack of saliva can lead to tooth decay in as little as three months after dry mouth begins.
What you can do
By staying on top of oral hygiene, you can ward off cavities and even reverse gingivitis. But it's going to take extra effort now. These steps can help keep your mouth — and the rest of you — healthy:
Brush your teeth at least twice a day and floss at least once. If you're still not removing enough debris, Dr. Thompson recommends adding an interdental brush to your routine. "It has a little cone-shaped bristle that fits between the teeth," she explains. "You can find it in the toothbrush aisle of any pharmacy."
If you have dry mouth, ask your dentist about a prescription toothpaste or mouth rinse with fluoride to help protect against cavities. Chewing gum with xylitol may also stimulate saliva production, which can help protect against cavities.
If you find brushing difficult because of arthritis, try an electric toothbrush or a toothbrush with an ergonomic handle.
Avoid smoking, which is a risk factor for gum disease.
If you have dentures, be sure to brush them daily and soak them overnight in a denture cleaner.
Don't skip check-ups and cleanings at your dentist's office (at least two to four times per year, depending on your gum health).
(09/11/2020)by Harvard School of Dental Medicine
More Information: https://www.mybestdentists.com/dental-schools/HarvardSchoolofDentalMedicine
Views: 3,504

Too much fluoride causes defects in tooth enamel
Exposing teeth to excessive fluoride alters calcium signaling, mitochondrial function, and gene expression in the cells forming tooth enamel -- a novel explanation for how dental fluorosis, a condition caused by overexposure to fluoride during childhood, arises. The study, led by researchers at NYU College of Dentistry, is published in Science Signaling.
Fluoride is a naturally occurring mineral that helps to prevent cavities by promoting mineralization and making tooth enamel more resistant to acid. It is added to drinking water around the world -- the U.S. Department of Health and Human Services recommends a level of 0.7 parts per million -- and all toothpastes backed by the American Dental Association's Seal of Acceptance contain fluoride. The Centers for Disease Control and Prevention (CDC) named water fluoridation one of 10 great public health achievements of the 20th century for its role in reducing tooth decay.

While low levels of fluoride help strengthen and protect tooth enamel, too much fluoride can cause dental fluorosis -- a discoloration of teeth, usually with opaque white marks, lines, or mottled enamel and poor mineralization. Dental fluorosis occurs when children between birth and around nine years of age are exposed to high levels fluoride during this critical window when their teeth are forming, and can actually increase their risk of tooth decay. A survey by the CDC found that roughly 25 percent of the U.S. population examined (ages 6 to 49) show some degree of dental fluorosis.
"The benefits of fluoride for oral health considerably outweigh the risks. But given how common dental fluorosis is and how poorly understood the cellular mechanisms responsible for this disease are, it is important to study this problem," said Rodrigo Lacruz, PhD, associate professor of basic science and craniofacial biology at NYU College of Dentistry and the study's senior author.
To investigate the molecular bases of dental fluorosis, the researchers analyzed the effects of exposing tooth enamel cells to fluoride -- levels on the higher end of what you would find in drinking water and consistent with what is found in areas where people commonly have fluorosis. They then assessed fluoride's impact on calcium signaling within the cells, given calcium's role in mineralizing tooth enamel.
The researchers found that exposing enamel cells from rodents to fluoride resulted in calcium dysregulation, with decreases in calcium entering and stored in the endoplasmic reticulum, a compartment within cells with many functions, including storing calcium. In addition, fluoride disrupted the function of mitochondria (the cells' power generators), and therefore energy production was altered. Finally, RNA sequencing -- which queries the genomes of cells -- revealed that, in enamel cells exposed to fluoride, there was an increased expression of genes encoding endoplasmic reticulum stress response proteins and those encoding mitochondrial proteins, which are involved in producing the cell's energy.
"This gives us a very promising mechanistic view of how fluorosis arises," Lacruz said. "If your cells have to make enamel, which is heavily calcified, and due to exposure to too much fluoride the cells undergo continued stress in their capacity to handle calcium, that will be reflected in the enamel crystals as they are formed and will impact mineralization."
The researchers then repeated the experiment using early-stage kidney cells from humans, but they did not observe the same effects when the kidney cells were exposed to fluoride -- suggesting that enamel cells are different from cells forming tissue in other parts of the body.

"You would think that if you expose the enamel cells and kidney cells to the same stressor -- treating them with the same amount of fluoride for the same period of time -- that you'd have more or less similar responses. But that was not the case," said Lacruz. "Under the same circumstances, enamel cells react to coping with stress in vastly different ways than kidney cells. We are unraveling a mechanism that highlights the uniqueness of enamel cells and explains why fluorosis is more of a problem in the teeth than anywhere else in the body."
(08/25/2020)by New York University
More Information: https://www.mybestdentists.com/dental-schools/NewYorkUniversity
Views: 3,449

How about Dental Sealants?
Dental sealants are thin, plastic coatings that seal over the narrow grooves found on the chewing surfaces of back teeth (molars and premolars).
When placed perfectly on these deep pits, sealants can prevent a significant amount of tooth decay (cavities) by protecting sensitive tooth surfaces from acid that causes cavities.
Sealants are not generally placed on baby teeth but on the tooth enamel of permanent teeth (“adult” teeth).
Dental sealants function much like sealing cracks in a driveway or on the sidewalk. The grooves in the chewing surfaces of back teeth are sealed so that food particles and bacteria will not settle within the fissures, causing cavities.
Application of sealants may be appropriate for some pediatric dental patients to prevent tooth decay in kids. However, they are not a substitute for brushing, flossing, and a healthy diet.
Dental sealants can be placed by your dentist, dental hygienist, or other dental professional. Some states dental boards have laws governing by whom, how, and in what circumstances dental sealants can be placed.
While I will recommend sealants at my office, I do so with very strict criteria, application techniques, and only the cleanest materials. So, are dental sealants worth it for your children’s dental health?
How are sealants applied to teeth?
Sealant placement is a relatively easy process.
First, the teeth are cleaned of plaque or food particles and then thoroughly examined for tooth decay.
Each tooth is dried and surrounded by absorbent material so it remains dry throughout the procedure.
The tooth is cleaned with a mild etchant (acid etch solution) to roughen the tooth surface and encourage bonding of the sealant material.
The etchant is rinsed and the teeth are dried again.
Depending on your material of choice, a thin layer of bonding agent may be used prior to the placement of the very viscous sealant material.
The sealant is painted directly onto the chewing surface of each tooth.
Finally, a curing light may be used to harden the dental sealant.
The teeth must be nicely isolated so no contaminants, such as saliva, affect the bond. Ozone gas can be applied to ensure bacteria on or around the tooth is reduced or eliminated prior to sealing.
If a small cavity is detected, air abrasion or a dental laser or drill can be used to clean out the infection prior to any material placement.
(06/24/2020)by Staci Whitman DMD
More Information: https://www.mybestdentists.com/AnastaciaMWhitman
Views: 3,440

Sindecuse Museum is devoted to preserving and exhibiting the history of dentistry
The Sindecuse Museum exhibits and preserves a historical museum collection containing over 25,000 objects focused on the history of dentistry with particular interest on dental practice and technology in the United States and Michigan dating from the 18th century to today. It is dedicated to educating it's audiences about the history of dentistry through museum exhibition, related programs, research, and preservation of the collections.

The museum was established in 1991 with a grant from Dr. Gordon H. Sindecuse, a 1921 graduate of the University of Michigan School of Dentistry. Its first professional part-time curator was hired that year. However, the museum's collections had been forming for several decades before the museum was established, as members of the School of Dentistry faculty, including Dr. Charles Kelsey, Professor Al Richards, and dental librarian Sue Segar, preserved and stored equipment, photos, and documents relating to the history of dentistry and the history of the dental school.

The Museum has a collection of more than 15,000 catalogued items, about 15 percent of which are displayed at one time.
For many years, dentistry in America was regarded as a low trade, a sort of “tooth carpentry” practiced by barbers, blacksmiths, and other multitasking professions.
In the early 1800s, practitioners began working to legitimize the profession and lift it to the ranks of a respected medical science. To make tooth care easier, more comfortable, and less hazardous, dentists developed specialized tools and furniture, refining them over the decades. These innovations eventually led to the modern dentist office.
The Sindecuse Museum is located in the atrium connecting the Kellogg Building with the School of Dentistry on the UM campus. The best way to access it is through the main entrance of the Kellogg Building located on Fletcher Street just off of North University Ave. The main entrance has stairs, but a handicapped entrance is available on the northern side of the building.
Parking can be hard to find on the busy University of Michigan campus, but parking structures are available in the nearby downtown district of Ann Arbor, Michigan.
(06/10/2020)More Information: https://www.mybestdentists.com/UniversityofMichigan
Views: 3,436

We think about your child’s body as a whole and not just your child’s teeth and mouth
As a holistic dentist and a member of the Holistic Dental Association, Doctor Staci thinks about your child’s body as a whole and not just your child’s teeth and mouth. We thoroughly examine and discuss how one part of the human body can affect another part and talk a lot about how we are interconnected system…not just a bunch of separate body parts.
In using the term biological dentistry, we are not attempting to stake out a new specialty for dentistry but rather to describe a philosophy that can apply to all facets of the dental practice and to health care in general: to always seek the safest, least toxic, and least invasive way to accomplish the mission of treatment and to discover the root cause of the issue to prevent it from happening again.
We uphold and attain all of the same goals of modern dentistry and try our best to do it while treading as lightly as possible on the patient’s biological terrain. A more biocompatible approach to oral health is the hallmark of biological dentistry. At NoPo Kids Dentistry, we have the following holistic and sustainable offerings at our office:
1. Mercury free
2. BPA/bis-GMA free
3. Non-invasive treatments like ozone and remineralizing options
4. Limit the plastics and waste in our office and emphasize recycling
5. Digital xrays to reduce exposures
6. Electronic charting to reduce paper waste
7. Multipure Water Filtration System for drinking water for all patients and staff and the advanced Ezee Klean by Oasis filtration for during treatment appointments
(07/03/2020)by Dr Anastacia Whitman
More Information: https://mybestdentists.com/mbd-newest-approved-dentists/AnastaciaMWhitman
Views: 3,393

Dentistry is an essential service says the ADA Board of Trustees
The American Dental Association Board of Trustees has adopted an ad interim policy stating dentistry is essential health care to help guide advocacy for the dental profession during the COVID-19 pandemic.
The Board established the ad interim policy via a video call July 27, and the House of Delegates will consider it as a resolution during its virtual meeting in October.
"This policy was created to recognize that dentistry is an essential service. Whether it's the current pandemic, a future epidemic or a natural disaster in a particular area, this policy recognizes the need for people to be able to continue to access the full range of dental services," ADA President Chad P. Gehani said (photo).
"Doing so will help people maintain their oral health and contribute to their overall health. Oral health is integral to overall health — staying well often depends on having access to health care, which includes dental treatment.

"From March 16-April 30, the ADA called for dentists to postpone all but urgent and emergency procedures to help mitigate the spread of COVID-19, keep patients out of overburdened hospital emergency departments and conserve personal protective equipment. By the end of May, most state governments had lifted restrictions on dental offices, but as COVID-19 cases continue to rise in many states, the dental community is concerned governors may again limit dental services to urgent and emergency care, which could negatively impact dentists and the oral health of the public, Dr. Gehani said.
The policy states oral health is an integral component of systemic health and dentistry is an essential health care service because of its role in evaluating, diagnosing, preventing and treating oral diseases, which can affect systemic health.
It advises that the ADA use the term "essential dental care" — defined as any care that prevents and eliminates infection and preserves the structure and function of teeth and orofacial hard and soft tissues — in place of "emergency dental care" and "elective dental care" when communicating with legislators, regulators, policymakers and the media about care that should continue to be delivered during pandemics and other disasters.
"Using the term 'elective dental procedures' implies oral health care is optional and diminishes the evidence validating that oral health is an integral component of overall health," Dr. Gehani said.
The policy also states the ADA will urge state agencies and officials to recognize the oral health workforce when designating its essential workforce during public health emergencies. Government agencies such as the Department of Homeland Security and Federal Emergency Management Agency have already acknowledged dentistry as an essential service.
(08/10/2020)by Mary Beth Versaci
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,390

WHY AN ENDODONTIST?
Your dentist has referred you to an endodontist because he or she understands that you will benefit from the specialized training and experience that a root canal specialist can offer. An endodontist is a dentist with special training in diagnosing and treating problems associated with the soft tissue inside of the tooth. To become an endodontist a dentist must complete an ADA certified, two-year, full-time program of advanced training in endodontics. We will work with you and your dentist to hold on to your natural dentition.
THE NATURAL CHOICE
There is nothing as good as your natural tooth! Your dentist has recommended a root canal because saving your teeth is the natural choice. There are many new ways to replace a missing tooth, but not even the most advanced implants or bridges can in fact replace your natural tooth. Not all teeth can be saved, but whenever possible saving your tooth should be your first choice it’s the natural choice!
WILL IT HURT?
Root canal treatment doesn’t cause pain it relieves it! A toothache is most often caused by infection or other damage to the soft tissue inside the tooth. Root canal treatment removes this damaged tissue from the tooth, thereby relieving the pain. Occasionally the healing can be delayed by pre-existing conditions such as infection and inflammation but in most cases conditions start improving after a few days.
IS IT SAFE?

Yes! Root canal treatment is a safe and effective procedure. Starting in the 1930s and continuing until today, research has shown that people with root canal fillings are no more likely to be ill than people without them. There is no relationship between the presence of endodontically treated teeth and the presence of illness.
THE BAD OLD DAYS
Recently a few very vocal dentists and physicians have been claiming that teeth that have received root canal treatment contribute to the occurrence of illness and disease in the body. This claim is based on the now obsolete studies performed by Dr. Weston Price from 1910-1930. Dr. Price believed that bacteria trapped in the teeth during root canal treatment can cause almost any type of disease, including arthritis, heart disease, kidney disease, and others. Although he and others meant well, their claims resulted in many millions of unnecessary extractions and mutilated mouths. Back then, many people in their 30’s and 40’s had all their teeth extracted for nothing and had to wear dentures for the rest of their lives. Sound like anyone you met?
(06/10/2020)More Information: https://mybestdentists.com/ManuelAnthonyBustamante
Views: 3,336

Dr. Telthorst believes that part of his job is to educate patients about their dental treatment so they can make informed choices
What does Dr Dean F. Telthorst love about my job? "Getting to know my patients and showing them how easy it is to stay healthy."
Dean F. Telthorst, DDS, FAGD has been in practice for over 30 years and armed with training from the prestigious Pankey Institute for Advanced Dental Studies, Dr Telthorst strongly believes in taking the time to understand his patients desires and individual situations.
“A dental exam starts with conversation, not with teeth,” he says. “It’s important that I have some understanding of the person that is before me. Only then can I recommend practical and appropriate dental treatment.”
Dr. Telthorst is meticulous and thorough in his work, which includes porcelain crowns, veneers, bonded white fillings, oral surgery, and the treatment of periodontal disease. “Patients hear these dental terms,” he observes, “but frequently don’t understand what it means for them today and the implications for their future.”
Earned his Doctor of Dental Surgery degree from the University of Missouri in 1983.
Became a Fellow of the Academy of General Dentistry in 1998
Attended the Pankey Institute for Advanced Dental Studies 2001, 2002, 2003, 2004, 2006
Member of the American Dental Association, Missouri Dental Association, Greater St. Louis Dental Society
Is a delegate to the Missouri Dental Association’s annual House of Delegates meeting
Served on the Board of Directors for the Greater St. Louis Dental Society 2006 – 2008
He became a fellow of the Academy of Dentistry International in 2012.
Received the Greater St Louis Dental Society Distinguished Service Award in 2015
President of the Dental Society 2018
Favorite restaurant: Rigazzi’s
Hobbies: motorcycling, photography
(09/15/2020)More Information: https://mybestdentists.com/DeanFTelthorst
Views: 3,326

When do babies start teething?
Newborns typically have 20 baby teeth concealed below the gumline. Teething is the process of these teeth erupting through the gums.
Teething usually begins about halfway through the first year of life. Different teeth erupt at different rates, with the front teeth tending to emerge first.

During teething, a baby may feel pain and discomfort, and they can show this in various ways.
In this article, we give a general timeline for the eruption of baby teeth. We also describe signs of teething and provide tips on easing any pain and discomfort.
According to the American Dental Association (ADA), baby teeth tend to appear within the first 6–8 months of life.The first teeth to erupt are usually the front teeth at the top or bottom of the mouth. Dentists refer to these teeth as the incisors. The rate and order in which the other teeth appear can differ from one baby to another.The ADA provide the following timeline of the usual ages at which baby teeth emerge:
1. lower central incisors (the bottom front two teeth): 6–10 months
2. upper central incisors (the top front two teeth): 8–12 months

3. upper lateral incisors (at either side of the central incisors): 9–13 months
4. lower lateral incisors (at either side of the central incisors): 10–16 months
5. upper first molars (behind the upper canines): 13–19 months
6. lower first molars (behind the lower canines): 14–18 months
7. upper canines: 16–22 months
8. lower canines: 17–23 months
9. lower second molars: 23–31 months
10. upper second molars: 25–33 months
If there is no sign of any teeth appearing at about 6 or 7 months of age, this is usually no cause for concern, according to the American Academy of Pediatrics.
By the baby’s first birthday, they should see a dentist, whether or not they have teeth yet.The enamel coating on baby teeth is thinner than that on adult teeth, and so it is more prone to cavities. For this reason, routine dental checkups are important for babies.
Signs of teething:
There are several indications that a baby is teething, including:
1. increased irritability
2. increased crying
3. drooling
4. a rash around the mouth, neck, or chest, caused by drooling
5. gnawing or biting on objects
6. cheek rubbing
7. ear pulling
8. a slight elevation in temperature, but not a fever
At about 6 months of age, when teething usually begins, a baby’s immune system is starting to develop, and the antibodies received from the placenta are wearing off. During this time, babies start developing colds and other viral illnesses.
(08/11/2020)by Jenna Fletcher
More Information: https://www.mybestdentists.com/in-the-news/AmericanDentalAssociation
Views: 3,312

What to eat when you're having dental issues
You know that what you eat directly impacts your health, and that includes the health of your teeth and gums. But it can work the other way around too. If you have an orthodontic appliance, such as braces, or have had certain dental problems or procedures, the health and comfort of your teeth and gums can directly impact what you eat. Here are some tips for what to eat and how to avoid these common dental issues.
Braces are delicate, and any food that you need to bite into to eat is prime for breaking braces. You can get around this by cutting the food, such as corn off the cob or rib meat off the bone, or slicing apples and chopping carrots into small, bite-size pieces.

Any food that you need to bite into to eat is prime for breaking braces. You can get around this by cutting the food, such as corn off the cob or rib meat off the bone, or slicing apples and chopping carrots into small, bite-size pieces. You may also experience problems eating after your braces are tightened–teeth may feel sore.
The first few days are the worst, so try eating softer foods like those listed below until the soreness passes: Scrambled eggs,oatmeal, soup with soft vegetables or pureed or cream soups, soft cheeses, including cottage cheese, smoothies and milkshakes, pudding and custard, meatloaf, mashed potatoes, sorbet and frozen yogurt, tortillas (soften by microwaving or steaming), yogurt, soft-cooked, shredded chicken and meat, protein shakes, tofu, ripe fruits, such as peaches and nectarines, cut into bite-size pieces, couscous, quinoa, bulgur, soft-cooked rice, pasta and noodles, polenta, baked apples, peanut butter, chicken or tuna salad, refried beans, avocado , applesauce, macaroni and cheese, pancakes, soft bread, saltines and matzoh, mashed bananas, cooked veggies, hummus, canned or cooked fruit.

If you get mouth sores, try these tips to make eating easier and speed healing: Choose cool or room temperature foods, blend and moisten dry or solid foods, drink through a straw to bypass mouth sores, eat high protein, high calorie foods to speed up healing time. For example, add protein powder to milk shakes or powdered dry milk to fortify mashed potatoes and soups.
Your nutrition and dietary needs following oral surgery or getting implants depends on factors including your nutritional status prior to your procedure, the extent of your procedure, how much impact there is on oral function and how long your recovery is expected to last. A liquid or soft foods diet may be required for a few days or longer, until your mouth heals. Opt for nutrient-rich foods such as fruits, vegetables, low-fat dairy foods and lean meats, eggs and beans whenever possible since they provide vitamins, minerals and nutrients needed for healing, including zinc, protein, and vitamins A and C.
Try these foods: Scrambled eggs, oatmeal or cream of wheat (make with milk instead of water to boost nutrition), soup with soft vegetables or pureed or cream soups, soft cheeses, including cottage cheese, smoothies and milkshakes, pudding and custard, meatloaf, mashed potatoes (fortify by mixing in powdered milk to boost nutrition, sorbet and frozen yogurt, tortillas (soften by microwaving or steaming), yogurt, soft-cooked, shredded chicken and meat, protein shakes, tofu,ripe fruits, cut into pieces like peaches and nectarines, peanut butter, saltines and matzoh, mashed bananas, cooked veggies, like carrots, squash, green beans, spinach and other greens, spinach soufflé, hummus, canned or cooked fruit.
Swallowing problems can occasionally happen, but if it persists, talk to your doctor since it could be related to something serious. Causes of swallowing issues vary and treatment depends on what is causing the problem. If you are having trouble swallowing, to prevent choking and aspiration avoid these foods: Alcoholic beverages, extremely hot foods and beverages, caffeine, spicy foods, popcorn, bran cereal, nuts, cottage cheese (unless pureed), skins of fruits, celery, dry, crumbly, or sticky foods (such as bread, cake, peanut butter, banana).
Depending on level of swallowing difficulty, the following foods may be included in the diet. These foods are grouped into four different categories:
Thin liquids that dissolve quickly in the mouth such as frozen yogurt, ice cream, gelatin and broth.
Nectar-like liquids where liquid coats and drips off a spoon such as nectars, milkshakes, cream soup and vegetable juices.
Honey-like liquids that flow off a spoon in a ribbon like in yogurt, tomato sauce and honey.
Spoon-thick liquids that are thickened to pudding consistency such as pudding, custard or hot cereal.
(09/30/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,286

HIV/AIDS and Dental Health
If you, or someone you know, is living with HIV/AIDS, the American Dental Association recommends that dental health care be part of all HIV/AIDS treatment plans. That’s because people living with HIV/AIDS are more susceptible to infections including dental infections, which can affect their overall health.
What Is HIV/AIDS?

HIV (human immunodeficiency virus) is a virus that attacks a specific type of T cell known as CD4 cells. T cells are an important part of the body’s immune system which is needed to fight infection. If left untreated, HIV can destroy so many CD4 cells that a person can no longer fight off infections and disease. AIDS (acquired immunodeficiency syndrome) is the last state of HIV infection where the immune system is so very weak that infection and cancer can take over.
How Does HIV/AIDS Affect the Mouth?

Your mouth may be the first part of your body to be affected when infected with HIV. Because infection with HIV will weakened your immune system, this means you will be susceptible to infections and other problems. In your mouth, this can cause pain and tooth loss. People with HIV may experience the following mouth issues:
Dry mouth
Thrush
White lesions on the sides of the tongue (oral hairy leukoplakia)
Red band gingivitis
Ulcerative periodontitis
Karposi’s Sarcoma
Outbreaks of herpes simplex virus
Canker sores
Mouth ulcers
Dental and mouth problems related to HIV can be painful, which can cause trouble chewing or swallowing. This may prevent you from taking your HIV medication. It can also result in malnutrition, as you may have trouble eating and absorbing enough essential nutrients. A compromised digestive system may affect the absorption of your HIV drug treatment.
How Can I Cope with Dental and Mouth Issues Related To HIV?
Most mouth health problems related to HIV are treatable. Talk to your dentist about what treatment is best for you. The best ways to prevent these issues are to do the following:
Visit your dentist for regularly scheduled appointments.
Brush and floss your teeth twice daily for two minutes.
Take your HIV medicine on schedule.
Tell your doctor if your HIV medicine is causing dry mouth. Ask what treatment is best for you.
If you do not have a regular dentist, ask your primary care provider or clinic for a referral.
(11/14/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,281

Cancer and Dental Health
More than one-third of all cancer patients develop complications that affect the mouth, according to the National Institute of Dental and Craniofacial Research. These mild to severe side effects can include mouth sores, infection, dry mouth, sensitive gums and jaw pain.
Your mouth health is an important part of your overall health, so make your dentist part of your cancer care team. If you don’t have a regular dentist, use the ADA Find-A-Dentist tool to search for an ADA member dentist in your area.

How Cancer Affects Your Mouth:

Cancer and its treatments, like chemotherapy, can weaken your immune system. If your mouth is not as healthy as possible prior to your cancer treatment, you may be more susceptible to infection. If the infection is serious enough, it can delay your cancer treatment. In addition, radiation therapy, especially in the area of the head and neck, can damage salivary glands which can cause thick, sticky saliva and extreme dry mouth. A dry mouth can increase your chances of tooth decay and infection.
Maintaining your mouth at its best health before, during and after cancer treatment could help lessen some side effects and allow you to focus on your overall healing.
If your mouth is not as healthy as possible prior to your cancer treatment, you may be more susceptible to infection. If the infection is serious enough, it can delay treatment.
Your dentist can evaluate your dental health and discuss which treatment options you should consider prior to starting cancer treatment. By treating areas of concern you may reduce possible dental side effects associated with chemotherapy and radiation. Some treatment options may include fluoride treatments to prevent cavities, filling existing cavities, treating gum disease, removing infected teeth or restoring crowns or bridge work to ensure you will be able to chew your food.
During the course of your cancer treatment you may experience mild to severe side effects. Be sure to consult with your cancer care team prior to dental checkups, especially if you have a port under your skin for receiving medication or feeding. This is important because patients with a port may also take anti-blood clotting medications, which can increase bleeding during dental and medical procedures and the risk of infection.
After cancer treatment, you may find yourself experiencing some dental issues or simply needing a regular checkup. As you're working toward your best health, don't forget to take care of your mouth. After all, it is the gateway to the rest of your body.
Visit Your Dentist:
Routine check-ups and cleanings are essential, so visit your dentist on a regular basis. Due to the effects of cancer treatment, you may have moderate to severe tooth decay as a result of dry mouth since saliva (spit) is essential in rinsing the mouth of food particles and plaque. Treatment may include filling cavities, root canals, or crown and bridge work.
(12/09/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,272

US Top Dental School University of Michigan
The University of Michigan School of Dentistry is one of the nation's leading dental schools engaged in oral health care education, research, patient care and community service. General dental care clinics and specialty clinics providing advanced treatment enable the school to offer dental services and programs to patients throughout Michigan. The dental school of the University of Michigan, located in Ann Arbor, Michigan was established in 1875. It is currently the number one ranked dental school in the U.S. and fifth in the world according to two independent rankings.
Major renovations and expansion started in the fall of 2018. Updates were made to further the school’s state-of-the-art facilities for teaching dental students, serving patients from around Michigan and conducting world-class research that advances the dental profession. House at the University is the Sindecuse Museum of Denistry. One of a few museums of it's type around the world. d within the School of Dentistry, is one of a handful of museums throughout the world devoted to preserving and exhibiting the history of dentistry
(07/03/2020)More Information: https://www.mybestdentists.com/dental-schools/UniversityofMichigan
Views: 3,263

University of Michigan Charts a Virtual Course in Pandemic-Era Instruction
The University of Michigan School of Dentistry, ranked the best dental school in the United States by Quacquarelli Symonds and the best in the world by the Academic Ranking of World Universities, moved quickly to launch remote teaching when the president of the university and the governor of the state both mandated shutdowns of all clinics and classes in March.
Virtual Lectures:

“The university said all teaching needed to be remote, and that was on Thursday or Friday. By Monday, we had to change, which was obviously a very short time to do that,” said Carlos González-Cabezas, DDS, MSD, PhD, associate dean for academic affairs and the Richard Christiansen Collegiate Professor of Oral and Craniofacial Global Initiatives.

The university immediately provided resources to help faculty develop online versions of their courses. For example, synchronous lectures happened online in real time so students could engage in questions and discussions, while asynchronous lectures were posted and archived so students could watch them on their own schedule.
Also, the university began training faculty in new methods for conducting secure yet accurate assessments of student performance. Many of these techniques involved moving away from traditional multiple choice questions and toward questions involving more critical thinking. Constant communication between faculty and the administration was key as well.
Hands-On Instruction:
These changes enabled the school to finish the remaining few weeks in its 2019-2020 academic year. As restrictions were lifted later in the spring, though, the school pivoted to bring back hands-on work in the preclinic with new infection control protocols.
“We were able to open the preclinic with half of the class at a time and using PPE (personal protective equipment),” González-Cabezas said. “Basically leaving an empty bench between the students, which meant that we had to double the number of sessions that we had to do. We had to extend the number of sessions to evenings and sometimes to Saturdays too.”
By July, things began to improve. The school expanded the number of clinical sessions and started doing rotations again. The PPE shortages got better. And while the clinics continued to use only about half of its chairs, it also began conducting airflow analysis to see how it could best prevent virus transmissions between chairs. And to fill in the gaps in clinical learning, the school ramped up its collaborative discussions too.
“We created clinical study clubs. We had faculty coaches with groups of about 12 students, and they started to meet regularly about three or four times per week to discuss actual patients, from diagnosis to treatment planning and interpretation of data, radiographs, and photographs,” González-Cabezas said.
Morale On Campus:
Yet González-Cabezas also noted that students seem to be more productive. There is a better student-to-faculty ratio, he said, with more one-on-one teaching. Students also are more focused because they know they can’t waste any time, he added. In fact, students can be found practicing between 7:30 and 11 pm, without much chit-chat between them.
“They’re just very focused. They’re down to business, because they know they have fewer chances,” González-Cabezas said.
As the state of Michigan moves into tougher lockdowns with the latest virus surge, though, the work remains difficult.
“The faculty can tell you they are tired. The increased number of sessions, and teaching remotely, is a challenge. It’s been already quite a few months, so people are getting tired. But it’s been an amazing, overwhelming response of support from both the faculty and the students,” he said.
“The students participate right now in all the decisions we make, how we make changes about these crazy schedules that we have. They’re all part of the decision making. We discuss how to do it better, how to do remote teaching better. They understand they are being partners with us, which has been really refreshing,” he said.
Looking Ahead:
González-Cabezas expects many of the changes that the school instituted to navigate the pandemic to remain once the crisis is over and things return to normal—or settle into a new normal.
“Some of the remote teaching will stay. I do think now we’re getting to a better place from a pedagogy perspective in the design of courses, syllabi, and learning goals than we were before because we were forced to look at these very carefully, and I think those things will stay,” he said.
Administrative routines will change as well. For example, in-person department meetings before the pandemic typically saw about 50% attendance. Since they’ve moved to a virtual format, attendance is now at least 75%, González-Cabezas said. Also, faculty who need to write grant proposals, papers, or similar work will be doing that work from home.
“People will feel more comfortable to stay at home than in the past,” he said.
Of course, González-Cabezas said, all of these changes were the result of a team effort and the work of his predecessor, Diane Hoelscher, DDS, MS, who managed the effects of the pandemic before he assumed his position on July 1.
“We responded very well for keeping safety as the primary goal and being able to carry out our mission, which was a very difficult balance,” he said. “And we’re still navigating that. The safety of our students, faculty, staff, and our patients is the number one priority. How to do that without stopping the school has been a challenge, but I think we’ve done reasonably well.”
(12/12/2020)by University of Michigan
More Information: https://www.mybestdentists.com/dental-schools/UniversityofMichigan
Views: 3,262

NYU study shows oral cancer pain may predict likelihood of cancer spreading
An oral cancer patient's pain intensity score could predict cancer metastasis, helping with future testing options and surgical decision-making, according to a study from the New York University College of Dentistry.
The authors of "Oncogenes Overexpressed in Metastatic Oral Cancers from Patients with Pain: Potential Pain Mediators Released in Exosomes," published in September by Scientific Reports, an open-access journal from Nature Research, used a questionnaire to document the pain experienced by 72 oral cancer patients before oral cancer surgery.
While most patients reported some pain, those with the most pain were more likely to have cancer that had spread to lymph nodes in the neck, suggesting patients with less pain were at lower risk of metastasis, according to the study. "While we need to undertake a follow-up study, our current data reveal that a patient's pain intensity score works as well as the current method — depth of invasion, or how deeply a tumor has invaded nearby tissue — as an index to predict metastasis," lead author Aditi Bhattacharya, Ph.D., said in an NYU news release about the study.

To help understand why metastatic cancers are more painful, the researchers looked for differences in gene expression in metastatic cancers from patients with high levels of pain and nonmetastatic cancers from patients not experiencing pain and identified 40 genes that were more highly expressed in painful metastatic cancers, suggesting those genes are associated with oral cancer metastasis and mediate cancer pain, according to the study.
One cause of cancer pain is attributable to the release of mediators from cancers that sensitize nerves near the tumor. Many of the 40 genes identified in this study code for proteins found in exosomes, small vesicles that break away from a cell and can be taken up by other cells. This is a potential mechanism for how oral cancer cells affect nerves, according to the study.
When the researchers injected the paws of mice with the extracellular fluid of oral cancer cells grown in culture, only those animals injected with the fluid containing exosomes experienced pain. This suggests exosomes from cancer may be responsible for oral cancer pain, according to the study."The identified genes are targets for therapy aimed at stopping pain and cancer. In addition, exosomes shed from cancers can be detected in saliva, blood and urine, offering the potential for an objective molecular test to diagnose risk of metastasis," said Donna Albertson, Ph.D., professor in the department of oral and maxillofacial surgery at the NYU College of Dentistry, an investigator at the NYU Bluestone Center for Clinical Research and the study's corresponding author.
When oral cancer spreads to lymph nodes in the neck, a patient's chance of survival is cut by half, according to the release. Because it's often unclear through imaging and physical assessment if oral cancer has spread, most oral cancer surgeries include preemptively removing lymph nodes, even though research shows as many as 70% of these prophylactic neck dissections are unnecessary, the release stated.

"Clinicians and researchers are keen to define a biomarker that accurately predicts metastasis," said Dr. Bhattacharya, who is also an assistant professor in the department of oral and maxillofacial surgery at the NYU College of Dentistry and an investigator at the NYU Bluestone Center for Clinical Research.
"Given that patients with metastatic oral cancer experience more pain, we thought that a patient’s level of pain might help predict metastasis. A surgeon could then use this knowledge to only remove lymph nodes in patients with cancers that are most likely to metastasize."
The study was supported by grants from the National Institutes of Health.
(11/17/2020)by NYU
More Information: https://www.mybestdentists.com/dental-schools/NewYorkUniversity
Views: 3,250

A dental exam starts with conversation, not with teeth says Dr Dean Telthorst
Dean F. Telthorst has been in practice for over 30 years and armed with training from the prestigious Pankey Institute for Advanced Dental Studies, he strongly believes in taking the time to understand his patients desires and individual situations. “A dental exam starts with conversation, not with teeth,” he says. “It’s important that I have some understanding of the person that is before me. Only then can I recommend practical and appropriate dental treatment.”
Dr. Telthorst is meticulous and thorough in his work, which includes porcelain crowns, veneers, bonded white fillings, oral surgery, and the treatment of periodontal disease. “Patients hear these dental terms,” he observes, “but frequently don’t understand what it means for them today and the implications for their future.” Dr. Telthorst believes that part of his job is to educate patients about their dental treatment so they can make informed choices.
Earned his Doctor of Dental Surgery degree from the University of Missouri in 1983. Became a Fellow of the Academy of General Dentistry in 1998 Attended the Pankey Institute for Advanced Dental Studies 2001, 2002, 2003, 2004, 2006 Member of the American Dental Association, Missouri Dental Association, Greater St. Louis Dental Society Is a delegate to the Missouri Dental Association’s annual House of Delegates meeting Served on the Board of Directors for the Greater St. Louis Dental Society 2006 – 2008
He became a fellow of the Academy of Dentistry International in 2012. Received the Greater St Louis Dental Society Distinguished Service Award in 2015 President of the Dental Society 2018
Hobbies: motorcycling, photography
What I love about my job: Getting to know my patients and showing them how easy it is to stay healthy
(09/02/2020)More Information: https://mybestdentists.com/DeanFTelthorst
Views: 3,245

Simple oral health steps help improve elite athletes' performance
Elite athletes who adopted simple oral health measures, such as using high fluoride toothpaste and cleaning between their teeth, reported significantly reduced negative effects on performance related to poor oral health, finds a study led by UCL.
The new research, published in BMJ Open Sport & Exercise Medicine, is the latest in a series of studies led by the UCL Centre for Oral Health and Performance (COHP), based at UCL Eastman Dental Institute, which have found that elite athletes have substantial rates of oral disease, including tooth decay and gum inflammation, and these symptoms negatively affected their wellbeing and sporting performance.

To help address this, researchers at UCL COHP designed a behavioral change program aimed at better educating elite athletes about oral health and providing some simple interventions to improve their daily oral health routines.
Explaining the study, lead author, Dr. Julie Gallagher (UCL Eastman Dental Institute), said: "Poor oral health of elite athletes is common and is associated with negative performance. However, compared with other health and training pressures, oral health care is not a high priority in elite sport.
"We therefore wanted to develop a program which was aligned with the existing high-performance culture of the athletes and their teams. Underpinning the study was health behavior psychology, which included education, self-motivation, goal setting, and an easy to use toolkit, ensuring the athletes had a readily available opportunity to improve."
In total, 62 athletes from two Great Britain Olympic Teams, rowing and cycling, and one Premiership Rugby Club, Gloucester Rugby, were recruited to the study.
Athletes and support teams were asked to watch a 10-minute presentation which focussed on building motivation to improve oral health, and three 90-second information films, featuring GB rower Zak Lee-Green, which focussed on increasing oral health knowledge and skills to perform optimum oral health behavior.

In addition,each athlete received an oral health screening to check for diseases such as caries (tooth decay) and gingivitis (gum inflammation). They were then given a bespoke follow up report with tailored advice and an oral health toolkit, containing a manual toothbrush, prescription fluoride toothpaste and flosspicks. As a minimum, they were also asked to brush their teeth for two minutes twice a day, to include brushing before training in the morning and before bed in the evening.
In total 89% of athletes completed the four-month study. On completion athletes were asked to fill in an oral health knowledge questionnaire, undergo a follow-up gingival (oral disease) assessment and evaluate the oral health kit.
Dr. Nigel Jones, Head of Medical Services at British Cycling, said: "The topic of oral health amongst athletes is an important one, especially as it can be linked to performance. My role with the Great Britain Cycling Team is to ensure the holistic well-being of our cyclists, and as oral health can have a big impact on immune function as well as being important in its own right, I wanted to support this project. The learnings which the riders took from the study have been invaluable and will be deployed across the whole team as we ramp up our preparations for the Tokyo Olympic and Paralympic Games next year."
Researchers believe the bespoke model they have developed could be used for other health promotion needs in elite sport.
(08/05/2020)by University College London (UCL)
More Information: https://www.mybestdentists.com/dental-schools/UCLEastmanDentalInstitute
Views: 3,242
Dr. Daniel J. Klemmedson discusses passion for dentistry
"Mrs. Klemmedson, Daniel has eight cavities." The pronouncement, made during a boyhood visit to the dentist, remains ingrained in Dr. Daniel Klemmedson's mind.
"I spent way too much time in the dentist's office," said Dr. Klemmedson. In spite of all the time he spent in the dentist’s chair, it was beside the chair where Dr. Klemmedson saw his future. As he remembers it, he was attracted to the convenience.
"I liked the fact that my dentist in Tucson lived in his office," Dr. Klemmedson said. "His office was attached to his house, and I thought that was pretty cool. "What started out as a career of convenience — either be a dentist or marry a dentist — became a passion, layered with greater complexity than what he had imagined as a teenager.

"What other profession allows for full use of intellectual abilities as well as surgical skills?" he asked. "We are the definition of primary care: Diagnosis, education, prevention and clinical care over a lifetime. The autonomy of practice choice, self-regulation and work-life balance cannot be beat."Dr. Klemmedson's career in organized dentistry will culminate Oct. 19 when he is installed as the 157th president of the American Dental Association at the virtual House of Delegates meeting. Because of the COVID-19 pandemic, the ADA Board of Trustees voted to hold the ADA FDC 2020 meeting and subsequently the House of Delegates virtually this year.
'I didn’t know how to stop'Dr. Klemmedson was born in Missoula, Montana, in 1954. His father's job in forestry and watershed management and his doctoral research at the University of California-Berkley forced the family to move around a bit during Dr. Klemmedson's youth: California, Boise, Idaho, and finally, Tucson, Arizona, where Dr. Klemmedson finished junior high, high school and ultimately obtained a bachelor's degree in biology from the University of Arizona.During a college summer, he served as a counselor for Camp Wildcat, a student-run organization at the University of Arizona that provided underprivileged children the opportunity to go camping in the mountains outside Tucson.
It was there he met another counselor: his wife, Adaline. They ultimately married before he started dental school at the University of Southern California in 1976.
Adaline got a job in the fundraising and development division for one of the vice presidents at USC, and benefited from a program to reduce Dr. Klemmedson's dental school tuition by half. A good portion of the remainder of his tuition was paid by the state of Arizona, which had no dental schools at the time so they collaborated with neighboring states to help residents financially.
As a result, Dr. Klemmedson graduated dental school relatively debt free. Without the debt and the stress that typically comes with it, Dr. Klemmedson had a lot more choices when it came to his next steps. His choice? More school."I did not know how to stop," Dr. Klemmedson said.Dr. Klemmedson completed a three-year oral and maxillofacial surgery residency at the Los Angeles County/USC Medical Center in 1983, obtained his medical degree from the University of Southern California School of Medicine in 1985 and completed a transitional internship in the Tucson Hospitals Medical Education Program in 1986.

You read that right: Dr. Klemmedson is a dentist, oral surgeon and M.D.After obtaining all of his degrees, Adaline ultimately put her foot down."Do you like what you do?" she asked. The answer was yes."Then get a job," she responded.
Dr. Klemmedson met his future partners while providing anesthesia for them during a clinical rotation at Tucson Medical Center. Drs. Theodore Kiersch and Edward Schneider were involved in organized oral surgery and invited him to a meeting at the Western Society of Oral and Maxillofacial Surgeons before he joined their practice."One of my partners became a trustee of the American Association of Oral and Maxillofacial Surgeons," said Dr. Klemmedson.
"I was constantly surrounded by organized dentistry and experienced the benefits first-hand."Dr. Klemmedson eventually became president of the Arizona Dental Association, vice chair of the ADA Council on Dental Benefit Programs, a member of the ADA Board of Trustees and now president-elect.He's switched partners a few times and currently has a practice in Tucson and a satellite one in Sierra Vista, Arizona, less than 10 miles from the Mexican border, where many of his patients come from the Fort Huachuca military base or are veterans from the area.For the past 30 years, Dr. Klemmedson has joined primary care and specialty physicians, audiologists, nutrition specialists, sociologists, dentists, orthodontists and oral and maxillofacial surgeons as a member of the Children's Clinics' cleft palate-craniofacial team.
Dr. Klemmedson coordinates surgical care with plastic surgeons and ear, nose and throat surgeons to address the many specific needs his pediatric patients require from birth to adulthood. His primary area of concentration is with the maxillary cleft closure and bone grafting, orthognathic surgery and dentoalveolar surgery.
During the little free time he does have, Dr. Klemmedson "putters around the yard" with his cacti and succulents; exercises every morning at 4:30 a.m.; is an avid cyclist, having ridden across major portions of Australia; and supports his wife's endeavors."My wife, she's kind of the star of the family to be honest," Dr. Klemmedson said. "She leads and I follow."Adaline ultimately became the program director of the Institute for Marine and Coastal Studies at USC.
In Tucson, she also worked in health care, ultimately retiring as a vice president of the teaching hospital associated with the University of Arizona College of Medicine. After retiring, she became a community volunteer and philanthropist "serving as the chair of more local groups in Tucson than I can name," Dr. Klemmedson said.
(08/18/2020)by Kelly Ganski
More Information: https://www.mybestdentists.com/in-the-news/AmericanDentalAssociation
Views: 3,220

Everything you need to know about canker sores
Canker sores are easily identified in the mouth; they are a widespread, well-known condition.
Although they can be very uncomfortable, they are rarely a cause for concern.
In this article, we ask if there is anything that can be done to relieve canker sores, and if there are times when they require medical attention.

A canker sore is a type of mouth ulcer, known medically as an aphthous ulcer. Canker sores are one of the most common complaints of the mouth.
They can occur at any age but are more likely in younger adults and women.
Children as young as two years may develop canker sores, but they do not normally appear until adolescence.
Although most people only have occasional canker sores, around 20-30 percent of people have recurrent episodes.
Canker sores are sometimes split into two categories:
Simple canker sores: they appear 3-4 times a year; they generally occur in people aged 10-20, and last about one week.
Complex canker sores: less common, larger, and more painful. They may last up to one month and leave a scar. Complex canker sores are often due to an underlying condition, such as a compromised immune system, Crohn’s disease, or vitamin deficiency.
Causes

Researchers have not yet provided a scientific explanation of why canker sores develop; however, there are some factors that are known to be involved, including viral infection.
The causes of recurrent cases of canker sore – known as recurrent oral aphthous ulcers or recurrent aphthous stomatitis – are also unclear, although there are links with a number of factors including a family history of aphthous ulcers, and allergies.
Ulcers are sometimes associated with other conditions needing medical attention, such as inflammatory bowel disease, compromised immunity, allergies, and nutritional deficiency.
The following factors are thought to be involved in the development of canker sores:
1. Hormonal changes.
2. Physical trauma (damage to the lining of the mouth, such as during dental treatment).
3. Drugs
4. Food hypersensitivity – for instance, citrus fruits and tomatoes can trigger or worsen a canker sore.
5. Nutritional deficiencies, including iron, folic acid, zinc, and vitamin B12.
6. Stress
A report by the United States Surgeon General estimates that up to 25 percent of the general population are affected by recurrent canker sores, noting there may be higher numbers among selected groups, such as health professional students.
Symptoms
Canker sores cause local pain and can be easily irritated. In simple cases, these are the only symptoms, although the pain may cause feelings of being fed up with the mouth ulcer.
Common features of canker sores include:
Well-defined, round, smaller than a centimeter across, and usually shallow in the mouth’s lining – mucosal surface.
Sometimes there is a tingling sensation before they appear.
White or yellow-gray center surrounded by an inflammatory red margin.
Often fading to gray over time.
Normally in the front part of the mouth, on its floor, inside of the lip (labial mouth), inside of the cheeks (buccal), or under the front or sides of the tongue.
Sometimes affecting the gums and, relatively uncommonly, the surface of the back part of the mouth.
Typically persists for 1-2 weeks before healing.
In some, more severe cases, symptoms can include:
1. feeling sluggish
2. swollen lymph nodes
3. fever
Canker sores and cold sores are different conditions:
Canker sores appear as white circles with a red halo; cold sores are normally fluid-filled blisters.
Canker sores appear inside the mouth; cold sores appear outside the mouth- often under the nose, around the lips, or under the chin.
Canker sores are not contagious; cold sores are caused by the herpes simplex virus (HSV) and, more rarely, HSV-2 (the genital herpes virus). Cold sores are contagious.
Common canker sores usually heal without the need for medical treatment. More severe or recurrent cases may be eased by prescribed treatments, although these do not “cure” the ulcers.
The home remedy below is suggested by the U.S. Library of Medicine and can be followed three or four times a day:
Rinse with mild, over-the-counter mouthwash or salt water (do not swallow).
Make a mixture that is half hydrogen peroxide and half water.
Use a cotton swab to apply some of the mixture directly to the sore.
Dab a small amount of milk of magnesia on the sore.
So-called alternative therapies may also be worth trying. A review of the management of canker sores written for the journal American Family Physician, listed a number of options, although it noted that there had been no randomized controlled trials to properly test safety and efficacy:
Anecdotes of relief and better healing from sucking on zinc gluconate lozenges (sold for the common cold).
Vitamin C, vitamin B complex, and lysine “may speed healing when taken orally at the onset of lesions.”
Sage and chamomile mouthwash 4-6 times a day may help – infuse equal parts of the two herbs in water.
Carrot, celery, and cantaloupe juices “have been reported as helpful.”
(08/06/2020)by UIC
More Information: https://www.mybestdentists.com/dental-schools/UniversityofIllinois
Views: 3,218

Dr Aleksander Iofin and his partner Dr Kim practice is located at Rockefeller center in New York City and both are experts in their fields
Dr. Aleksander Iofin practices endodontics full-time at Rockefeller center in New York City and teaches part-time as an Assistant Clinical Professor of the Department of Endodontics at Columbia University College of Dental Medicine and Adjunct Assistant Professor at the School of Dental Medicine, University of Pennsylvania.
He was recognized by the Dean of the Columbia University College of Dental Medicine for his dedicated service teaching post-doctoral students since 2005.

Dr. Iofin graduated from Rutgers University with highest honors and received his dental degree from Harvard School of Dental Medicine with honors for his graduation thesis. His endodontic specialty training was completed at the Department of Endodontics at New York University College of Dentistry.
Currently, Dr. Iofin is a Board-eligible member of the American Association of Endodontists. In addition to teaching at Columbia University, Department of Endodontics, he also has lectured on modern endodontic techniques using the microscope and microendodontic instrumentation at the Greater New York Dental Meeting, the New York County Dental Society, the Rockefeller Study Club as well as other dental clubs in the New York area.
Dr. Iofin is a co-author of the 2018 Microsurgery in Endodontics textbook.
Dr. Iofin served as President of the New York State Association of Endodontists.
He is also a former member of the Board of Directors of the NY County Dental Society.
Dr. Iofin and his wife, a pediatric dentist, are proud parents of two daughters.
His interests include literature, theater and travel. He is also an avid sports fan who enjoys skiing and soccer.
His partner is Syngcuk Kim, DDS, PhD (third photo)

Dr. Kim is the Louis I. Grossman Professor and chairman of the Department of Endodontics and the Associate Dean for Global Education at the School of Dental Medicine, University of Pennsylvania
Dr. Kim earned his dental degree and certificate in Endodontics from the School of Dental and Oral Surgery at Columbia University in New York. Dr. Kim also received his Ph.D. degree in circulatory physiology from the Department of Physiology at the Medical School, Columbia University. Dr. Kim is well known and respected for his research in dental pulp physiology and microcirculation and the American Association of Endodontists has awarded him the Louis I. Grossman Award for outstanding research.
Dr. Kim is one of the pioneers in the field of microsurgical endodontics and is an internationally renowned speaker. He is the primary author of the book titled “Color Atlas of Microsurgery in Endodontics”.
(09/05/2020)
More Information: https://mybestdentists.com/AleksanderIofin
Views: 3,216

Can we make bones tooth formation heal faster?
A new paper in Science Advances describes for the first time how minerals come together at the molecular level to form bones and other hard tissues, like teeth and enamel.
The University of Illinois Chicago researchers who published the paper described their experiments -- which captured high-resolution, real-time images of the mineralization process in an artificial saliva model -- and their discovery of distinct pathways that support bone and teeth formation, or biomineralization.
"Until now these pathways, particularly at the early stages when molecules are first starting to organize into a structure, have not been understood clearly," Reza Shahbazian-Yasser, UIC professor of mechanical and industrial engineering at the College of Engineering and corresponding author of the paper.
Shahbazian-Yasser and his colleagues observed that both direct and indirect formations of hydroxyapatite crystals -- the foundation of hard tissues -- can be achieved by local variations in energetic pathways for nucleation and growth.
"The control over the dissolution of amorphous calcium phosphate affects the assembly of hydroxyapatite crystals into larger aggregates," Shahbazian-Yasser said. "Using technology developed at UIC, we found evidence that these pathways coexist simultaneously -- explaining why different groups had reported seemingly different or opposite results. In addition, we now understood how hydroxyapatite materials nucleate and grow on amorphous calcium phosphate templates. The control over the nucleation and growth of hydroxyapatite will aid in developing new drugs and medical treatments to heal lost or broken bone faster or cure tooth cavities."
To capture the images, the researchers used a unique micro-device that made it possible to use electron microscopy with a liquid model. Using this method, the researchers were able to monitor chemical reactions in the model on the smallest scale.
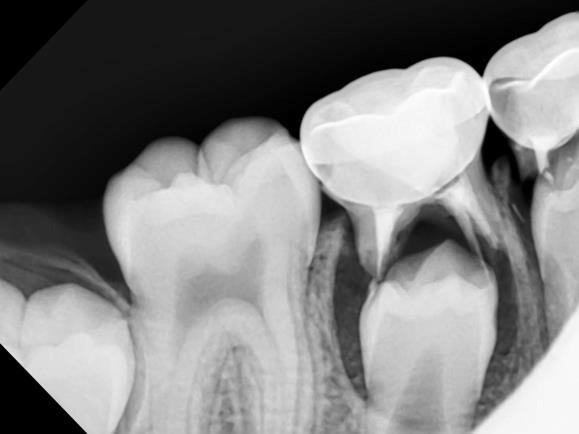
"Our study provides clear, new evidence of how minerals organize and grow into bone materials, and this finding has many important implications for further research on bone or teeth healing," Shahbazian-Yasser said.
"By better understanding these pathways, scientists are one step closer to engineering ways to better treat dental diseases and bone injuries -- like those from traumatic injuries -- or prevent medical conditions that can develop when normal mineralization processes in the body go awry," he said.
Medical conditions caused by dysfunctional mineralization in the body can include everything from a tendency to develop cavities to osteoporosis.
"In the next step, we would like to learn how molecular modifiers can affect the process of biomineralization, which is important to develop effective drugs," Shahbazian-Yasser said.
(12/30/2020)by UIC
More Information: https://www.mybestdentists.com/dental-schools/UniversityofIllinois
Views: 3,214

Dr Godorecci was a four-year Letterman, Running back on his college football team
Dr. Jim Godorecci was born and raised in Media, Pennsylvania. A graduate of Archmere Academy, Dr. Godorecci received his Bachelor's degree from Gettysburg College, where he was a four-year Letterman, Running Back on the football team. In becoming the outstanding dentist he is today, Dr. Godorecci graduated from the University of Pennsylvania School of Dental Medicine and completed an Oral Surgery externship at Parkland Memorial Hospital in Dallas, Texas.
Dr. Godorecci has developed expert skills and a deep compassion for his patients over 20 years of practicing family, cosmetic and restorative dentistry, in Chester and Delaware Counties. Dr. Godorecci has completed continuing education and training in areas such as dental implants, porcelain veneers, orthodontics and endodontics to ensure his patients receive the most effective and comfortable care possible.

When Dr. Godorecci is not at a continuing education course, he can be found spending time with his family, biking, cooking and coaching community sports. He and his wife, Kari, live in Paoli with their four children, and two Labrador retrievers. Jim and Kari enjoy being active in their children's activities, school and community events.
In acquiring Main Line Dental Aesthetics, in 2010, Dr. Godorecci has fulfilled his lifetime career goal of living and practicing in the same community. Dr. Godorecci has established long term relationships with families and now offers quality services in a beautiful, relaxing and home-like atmosphere.
(09/03/2020)More Information: https://mybestdentists.com/JamesAlfredGodorecciJr
Views: 3,214
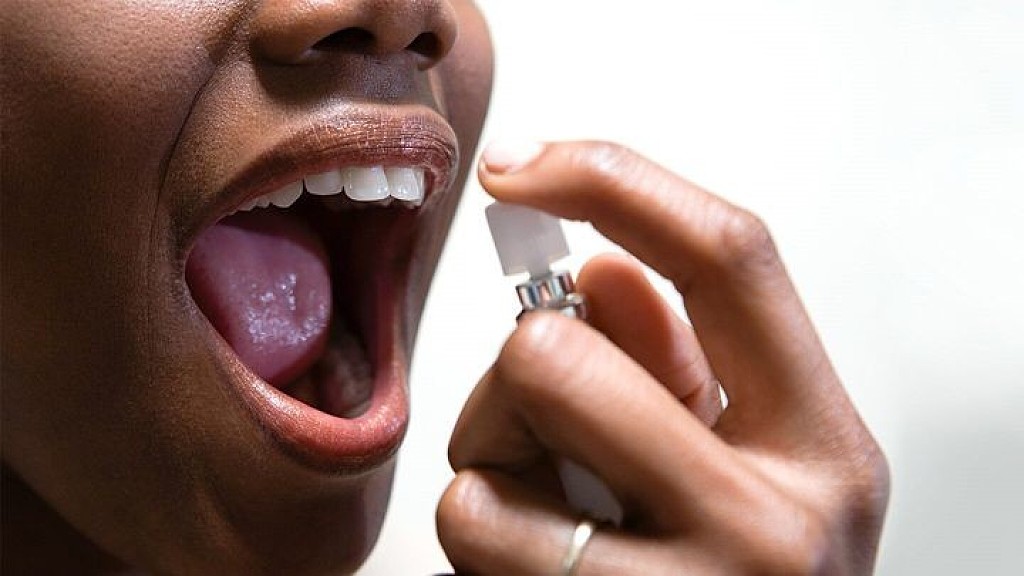
How dental issues can cause bad breath?
Almost everyone experiences bad breath once in a while. But for some people, bad breath is a daily problem, and they struggle to find a solution. Approximately 30% of the population complains of some sort of bad breath. Halitosis (Latin for “bad breath”) often occurs after a garlicky meal or in the morning after waking. Other causes of temporary halitosis include some beverages (including alcoholic drinks or coffee) and tobacco smoking.
Some people may not be aware of their own halitosis and learn about it from a relative, friend, or coworker, causing some degree of discomfort and distress. In severe cases, bad breath may negatively impact personal relationships and a person’s quality of life.

What causes bad breath? And what can you do about it?
Bad breath can originate both inside and outside of the mouth. Bad breath is typically caused by bacteria present on the teeth and debris on the tongue. So it’s no surprise that most cases of halitosis are associated with poor oral hygiene, gum diseases such as gingivitis and periodontitis, and dry mouth, a condition in which the salivary glands cannot make enough saliva to keep your mouth moist. A visit with a dentist may help rule out periodontal disease and identify any mouth problem that could be contributing to bad breath.
Tonsillitis, respiratory infections such as sinusitis or bronchitis, and some gastrointestinal diseases may be responsible for a small number of cases of bad breath. Advanced liver or kidney disease and uncontrolled diabetes can also lead to unpleasant breath. In these cases, a person is likely to experience significant symptoms beyond bad breath, and should seek medical attention.
Sometimes people think they have bad breath, even when their breath is objectively fine. This is called “pseudo-halitosis.” Halitophobia, or fear of bad breath, is real and may persist despite reassurance from a doctor. People with pseudo-halitosis respond well to reassurance, and may benefit from speaking with a therapist or psychiatrist who has expertise in the field.
A person complaining of bad breath can be initially evaluated by a primary care physician (PCP). The doctor will begin with a thorough medical and dental history and an oral exam. Tests may be done to confirm the presence of halitosis by measuring the strength of bad breath on a predefined scale, and by using instruments to detect specific compounds related to halitosis. The intensity of malodor is usually assessed by the doctor smelling the air that the person breathes out through the nose or mouth, or from judging the odor of a tongue scraping, a length of dental floss, or a dental appliance such as a night guard.

Your PCP may refer you to a dentist if there is evidence of dental or gum problems, which is the cause in the majority of people with bad breath. Visits with other medical specialists are warranted when an underlying medical problem requires attention.
Tips to improve bad breath
Here are some helpful tips to improve bad breath:
Brush your teeth at least twice a day, after meals, with a fluoridated toothpaste.
Avoid tobacco smoking and chewing tobacco-based products.
Rinse and gargle with an alcohol-free mouthwash before bed.
If you have dry mouth, make sure to drink enough fluids throughout the day and use over-the-counter moisturizing agents, such as a dry mouth spray, rinses, or dry mouth moisturizing gel. If you don’t see any improvement, you may want to schedule a visit with an oral medicine specialist. Oral medicine doctors provide comprehensive care for mucosal diseases, salivary gland disorders, orofacial pain conditions, and oral complications of cancer therapies, among other things.
Visit your dentist regularly. Remember, oral causes are responsible for most cases of bad breath!
(10/07/2020)by Harvard School of Dental Medicine
More Information: https://www.mybestdentists.com/dental-schools/HarvardSchoolofDentalMedicine
Views: 3,199

We highly recommend your child visit the dentist before his or her 1st birthday
Dr. Chin and Associates strive to make your child’s first visit gratifying and positive by introducing them to the teeth cleaning and dental care in a particular and considerate manner. We have created this visit to create a warm and friendly environment that your child feels comfortable and at home in. We introduce them to dentists and explain all procedures and answer any questions parents or guardians might have.
We suggest refraining from using words around your child that might strike unnecessary fear, such as needle, pull, drill or hurt. Our office staff has been intentionally trained to use words that convey the same message, but are pleasant and non-frightening to the child.
(09/11/2020)More Information: https://mybestdentists.com/DavidAlanChin
Views: 3,187

It’s important to realize that your dentist sees much more than just your teeth
Many Americans today enjoy excellent oral health and are keeping their natural teeth throughout their lives. But this is not the case for everyone. Cavities are still the most prevalent chronic disease of childhood.
Too many people mistakenly believe that they need to see a dentist only if they are in pain or think something is wrong, but they're missing the bigger picture. A dental visit means being examined by a doctor of oral health capable of diagnosing and treating conditions that can range from routine to extremely complex.

A Team Approach
The team approach to dentistry promotes continuity of care that is comprehensive, convenient, cost effective and efficient. Members of the team include dental assistants, lab technicians and dental hygienists. Leading the team is the dentist, a doctor specializing in oral health who has earned either a Doctor of Dental Medicine (DMD) degree or a Doctor of Dental Surgery (DDS) degree, which are essentially the same.

The Dentist's Role
Dentists are doctors who specialize in oral health. Their responsibilities include:
Diagnosing oral diseases, Promoting oral health and disease prevention, Creating treatment plans to maintain or restore the oral health of their patients, Interpreting x-rays and diagnostic tests, Ensuring the safe administration of anesthetics, Monitoring growth and development of the teeth and jaws, Performing surgical procedures on the teeth, bone and soft tissues of the oral cavity.
More than Just Teeth and Gums
Dentists' areas of care include not only their patients' teeth and gums but also the muscles of the head, neck and jaw, the tongue, salivary glands, the nervous system of the head and neck and other areas. During a comprehensive exam, dentists examine the teeth and gums, but they also look for lumps, swellings, discolorations, ulcerations — any abnormality. When appropriate, they perform procedures such as biopsies, diagnostic tests for chronic or infectious diseases, salivary gland function, and screening tests for oral cancer.
In addition, dentists can spot early warning signs in the mouth that may indicate disease elsewhere in the body. Dentists' training also enables them to recognize situations that warrant referring patients for care by dental specialists or physicians.
Education and Clinical Training
The level of education and clinical training required to earn a dental degree, and the high academic standards of dental schools, are on par with those of medical schools and are essential to preparing dentists for the safe and effective practice of modern oral health care.
Most dental students have earned Bachelor of Science degrees or their equivalent, and all have passed rigorous admission examinations.
The curricula during the first two years of dental and medical schools are essentially the same — students must complete such biomedical science courses as anatomy, biochemistry, physiology, microbiology, immunology and pathology. During the second two years, dental students' coursework focuses on clinical practice — diagnosing and treating oral diseases.
Why Oral Health Matters
Numerous recent scientific studies indicate associations between oral health and a variety of general health conditions — including diabetes and heart disease. In response, the World Health Organization has integrated oral health into its chronic disease prevention efforts "as the risks to health are linked."
The American Dental Association recommends that dental visits begin no later than a child's first birthday to establish a "dental home." Dentists can provide guidance to children and parents, deliver preventive oral health services, and diagnose and treat dental disease in its earliest stages.
Dentists' areas of care include not only their patients' teeth and gums but also the muscles of the head, neck and jaw, the tongue, salivary glands, the nervous system of the head and neck and other areas.
(12/08/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,172

ADA Practice Transitions expands nationally in October
When Dr. Shanna L. Gagnon was looking for an associate dentist to join her practice, she considered one factor as the most important in finding a successful hire: practice philosophy.
“Personality definitely plays a role as well, but if the doctor and the new associate do not have the same philosophy of care, it will not work out,” she said. To ensure she found an associate with a similar practice philosophy in her search, Dr. Gagnon decided to try a new service offered by the ADA a try.“I took the ADAPT application very seriously and put a lot of thought into it as I filled out my profile,” she said. “I figured that the more complete and honest the profile, the more likely I would be matched with the right candidate.”

In July, Dr. Gagnon officially welcomed Dr. Jessica Sikora to her practice, Gagnon Dental in Farmingdale, Maine. The two were matched by ADA Practice Transitions (ADAPT), a service backed by the ADA focused on helping dentists make the process of joining or leaving a practice predictable and successful. This occurred as Dr. Sikora neared graduation from the University of New England College of Dental Medicine earlier this year.
Come October, dentists nationwide will be able to take advantage of the ADA Practice Transitions like Drs. Gagnon and Sikora.The service announced Sept. 9 it is expanding its services to all 50 states and is encouraging dentists to answer three quick questions at ADAPracticeTransitions.com to become an ADAPT Insider and receive early access to create a profile before the October opening. By filling out the form, dentists will also be entered to win a $100 Amazon gift card.

Dr. Gagnon, who serves on the Maine Dental Association board of directors, was impressed by a presentation on ADA Practice Transitions last fall, and began her profile right away, as Maine was an early pilot state for ADA Practice Transitions.
“I could not be happier with my new associate, Dr. Sikora,” she said. “It is very obvious that the ADA has done their homework in attempting to set up a successful matching service.”ADA Practice Transitions piloted the service in Wisconsin, Maine, Indiana, Iowa, Kentucky, Michigan, Minnesota and New Hampshire for dentists seeking to join or purchase a practice in those states who are looking to hire an associate or find someone to purchase their practice.
“ADA members, volunteer leaders and state associations all over the country have expressed interest in what ADA Practice Transitions is doing, and so we are happy to be able to expand nationally,” said Dr. Kirk Norbo, ADA Business Innovation Group board chair. “Part of the value of ADA Practice Transitions is its ability to use the platform to match dentists nationwide for those who are seeking to move to a different state. We anticipate that over time, the ADA Practice Transitions platform and methodology will become the first choice for dentists seeking a transition.”
Through ADA Practice Transitions, dentists receive:
• Matches with dentists or practices that aligns with their personal and professional goals.
• Step-by-step support from a dedicated ADA advisor.
• Customized resources and help defining the right path.
ADA Practice Transitions helps retiring owners find the right person to continue to care for their patients, and helps owners hire associates who share a similar philosophy of care, ensuring a successful transition and continuity of care for patients.In addition, ADA Practice Transitions helps buyers and associates find the practice that fits their criteria and shares their goals.
ADA Practice Transitions can also help a dentist explore and narrow down their options to provide more confidence in taking their next steps.
(09/12/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,160

One in 10 older dental patients inappropriately prescribed opioids
A new study by researchers at the University of Illinois Chicago and the University of Pittsburgh suggests that a significant proportion of older patients receiving opioids at dental visits also use psychotropic medications—a potentially harmful combination. Their findings are published in the journal Pharmacotherapy.
Rates of polypharmacy, or taking multiple medications, are high among older adults who are more likely to be managing more than one health issue at any given time. Psychotropic medications that act on the central nervous system, such as antianxiety or antidepressant medications, are especially dangerous if taken with opioids because they can interact with each other and have negative effects.
"Some of the most concerning negative outcomes of these combinations include overdosing on opioids or falling, which can necessitate a visit to the hospital, which in itself carries greater risk for older adults," said Gregory Calip, associate professor of pharmacy systems, outcomes and policy at the UIC College of Pharmacy and corresponding author on the paper.
The researchers looked at medical, dental and pharmacy claims data from 40,800 older adult dental patients who visited a dentist between 2011 and 2015 and were prescribed opioids. The data was from the IBM Watson MarketScan databases.

The average age of the patients included in the study was 69 years old and 45% were female. Of these patients, 10% were taking medications that are associated with increased risks for harm with opioid prescriptions.
There were a total of 947 hospitalizations or emergency room visits among these patients.
The researchers found that among patients prescribed opioids by their dentist, 1 in 10 were already taking a prescription medication that should not be prescribed with opioids.
They also found that patients inappropriately prescribed an opioid medication combination by their dentist were 23% more likely to be hospitalized or visit an emergency department in the 30 days after the dental visit where they were prescribed an opioid, compared with dental patients who were not prescribed an opioid medication.
"Dentists are among the top prescribers of opioids," said Katie Suda, professor of medicine at the University of Pittsburgh School of Medicine and principal investigator of the study. "It seems that the increased messaging regarding limiting opioid prescriptions has been aimed primarily at medical physicians and not tailored to other specialist providers, including dentists. This can have dire consequences. As we saw in our study, opioid interactions with other medications was likely responsible for the significant rise in emergency room visits and hospitalizations."
"Although the percentage of opioids prescribed by dentists has decreased in the last 20 years, dentists must continue interprofessional collaboration with primary care physicians, pharmacists, and other health care providers to address devastating and preventable drug interactions affecting vulnerable patients who look to them for safe and compassionate care," said Dr. Susan Rowan, executive associate dean and associate dean for clinical affairs at the UIC College of Dentistry.
(09/18/2020)by University of Illinois at Chicago
More Information: https://www.mybestdentists.com/dental-schools/UniversityofIllinois
Views: 3,156

What is Cosmetic Dentistry?
Cosmetic dentistry combines the best dentistry practices to give you a smile that is both healthy and attractive. A beautiful smile can change your life. It can brighten your entire outlook on life, improving your self-confidence and creating great first impressions.
However, it is important to understand that cosmetic dentistry is not just about aesthetics; it also places a strong emphasis on treating your condition so that you can maintain excellent oral health for years to come. This balance between the functional and aesthetic sides of dentistry makes cosmetic dental restorations the best option to treat your condition.
(06/10/2020)More Information: https://www.mybestdentists.com/TrevaDianeLee
Views: 3,148

Diabetes and Your Smile
Did you know that 29.1 million people living in the United States have diabetes? That’s 9.3% of the population. Approximately 1.7 million new cases are diagnosed each year—and 8.1 million people living with diabetes don’t even know they have it.Diabetes affects your body’s ability to process sugar. All food you eat is turned to sugar and used for energy. In Type I diabetes, the body doesn’t make enough insulin, a hormone that carries sugar from your blood to the cells that need it for energy. In Type II diabetes, the body stops responding to insulin. Both cases result in high blood sugar levels, which can cause problems with your eyes, nerves, kidneys, heart and other parts of your body.So what does this have to do with that smile of yours — and how can you protect it? First, it’s important to understand the signs of diabetes and the roles they play in your mouth.
The Symptoms of Untreated Diabetes
The warning signs of diabetes affect every part of your body. After a blood test, you may be told by a doctor that you have high blood sugar. You may feel excessively thirsty or have to urinate a lot. Weight loss and fatigue are other common symptoms. Diabetes can also cause you to lose consciousness if your blood sugar falls too low.If diabetes is left untreated, it can take a toll on your mouth as well. Here's how:

You may have less saliva, causing your mouth to feel dry. (Dry mouth is also caused by certain medications.)
Because saliva protects your teeth, you’re also at a higher risk of cavities.

Gums may become inflamed and bleed often (gingivitis).
You may have problems tasting food.
You may experience delayed wound healing.
You may be susceptible to infections inside of your mouth.
For children with diabetes, teeth may erupt at an age earlier than is typical.
Why People with Diabetes Are More Prone to Gum Disease
All people have more tiny bacteria living in their mouth now than there are people on this planet. If they make their home in your gums, you can end up with periodontal disease. This chronic, inflammatory disease can destroy your gums, all the tissues holding your teeth and even your bones.Periodontal disease is the most common dental disease affecting those living with diabetes, affecting nearly 22% of those diagnosed. Especially with increasing age, poor blood sugar control increases the risk for gum problems. In fact, people with diabetes are at a higher risk for gum problems because of poor blood sugar control. As with all infections, serious gum disease may cause blood sugar to rise. This makes diabetes harder to control because you are more susceptible to infections and are less able to fight the bacteria invading the gums.
How Your Dentist Can Help You Fight Diabetes
Regular dental visits are important. Research suggests that treating gum disease can help improve blood sugar control in patients living with diabetes, decreasing the progression of the disease. Practicing good oral hygiene and having professional deep cleanings done by your dentist can help to lower your HbA1c. (This is a lab test that shows your average level of blood sugar over the previous three months. It indicates how well you are controlling your diabetes.)
Your Diabetes Dental Health Action Plan
Teamwork involving self-care and professional care from your dentist will be beneficial in keeping your healthy smile as well as potentially slowing progression of diabetes. Here are five oral health-related things you can do to for optimal wellness:
Control your blood sugar levels. Use your diabetes-related medications as directed, changing to a healthier diet and even exercising more can help. Good blood sugar control will also help your body fight any bacterial or fungal infections in your mouth and help relieve dry mouth caused by diabetes.
Avoid smoking.
If you wear any type of denture, clean it each day.
Make sure to brush twice a day with a soft brush and clean between your teeth daily.
See your dentist for regular checkups.
(10/21/2020)
by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,145

Dr Treva Lee's drive to become a dentist originally sprang from her desire to help her friends and neighbors
Dr. Lee earned her dental degree from the University of California at Los Angeles and completed her residency in Hospital Dentistry at University Medical Center in Fresno. She has also completed more than 600 hours of postgraduate continuing education. Dr. Lee believes that having a solid education is critical to ensuring the highest level of patient care.
Dr. Treva Diane Lee grew up in the Central San Joaquin Valley and is a Bullard High School graduate. She attended UC Berkeley and received her Bachelor's degree with Honors in the Food, Nutrition, and Dietetics major.
To Dr. Lee, the community is very important. You may not know that her drive to become a dentist originally sprang from her desire to help her friends and neighbors from Fresno and Madera counties.
As a dentist, Dr. Lee focuses on providing top-notch, personalized attention to her patients. To give back to her community, Dr. Lee provides complimentary screenings at local schools during Children’s Dental Health Month, gives care to the less fortunate in Ocoroni, Mexico through LIGA, participates in TeamSmile, combining major sporting events and children's dental care, Give Kids A Smile, fundraising for local Alzheimer's organizations with the Senior Living Network, and local charities with Parker's Team/Central Valley Charitable Cycling Association.
Dr. Lee is an active member of many notable professional organizations, including achieving a Mastership in the Academy of General Dentistry,and International Congress of Oral Implantologists (ICOI) (of which she is a Fellow), the American Dental Association, International Association for Orthodontics, the Dental Organization for Conscious Sedation, the American Association of Women Dentists, the California Dental Association, and the Fresno Madera Dental Society. Dr. Lee is also active with the Clovis Chamber of Commerce and the Fresno Women's Network.
She is also a gifted speaker, having lectured at high schools in the area, and is a certified instructor at San Joaquin Valley College.
Serving the area around Clovis and Fresno, dentist Treva Lee, D.D.S., has the skill, expertise, and training necessary to provide high-quality, easy-care dental services that can really make a difference in her patients' lives.
She knows that to give the best care to her patients from Fresno and Madera counties, she must be a dentist with more than just good technique. This is why she is also committed to better understanding and getting to know her patients personally, thereby knowing the best ways to help them.
(11/09/2020)More Information: https://mybestdentists.com/TrevaDianeLee
Views: 3,130

