Dentists Journal
Top Ten Stories of the Week
9/21/2024
All Dentists Journal · Previous Week · This Week · All Time List · Headlines
Serious Health Issues Caused by Poor Oral Health
Bad teeth are more worrisome than not having a perfect smile. A person’s teeth do have an impact on their health, and this impact goes well beyond what most people think. Your teeth are an indicator of health, and damaged or even crooked teeth can cause you serious health problems.
What Health Problems Do Bad Teeth Cause?
1. Periodontal Disease
Periodontal disease is often indicated by bleeding gums and swollen gums. It often results in infections of the structures around your teeth. Periodontal disease can, according to recent studies, lead to high risks of:

Stroke
Heart disease
Diabetes

Respiratory issues
The best way to prevent periodontal disease is to follow a proper brushing schedule. Use the best electric toothbrush, visit the dentist and follow a professional teeth cleaning schedule.
2. Respiratory Infections
Your teeth are the gateway to your stomach. Bacteria and infections in your gums can lead to you having respiratory problems. The Journal of Periodontology claims that over time, infected gums and teeth can lead to:
Infections in your respiratory tract
Pulmonary disease
COPD
Pneumonia
This is a severe case, and a routine dental cleaning is often the best way to determine if you have tooth decay and infections that are bad enough to have a serious impact on health.
3. Diabetes
Diabetes is a serious issue that is impacting 9.4% of the U.S. population. There is a direct link between diabetes and bad dental health. This link works in both directions. People with bad dental hygiene and poor diets often eat sugary foods that are bad for their teeth.
Diabetics also have a compromised immune system, and this makes them more susceptible to developing bacterial infections.
Bad teeth and severe gum disease also make it more difficult to maintain blood sugar control. Lack of blood sugar control leads to a higher risk of developing diabetes.
4. Dementia
Brain health is also tied to your teeth. A surprising link between oral health and dementia has been made. Tooth loss in seniors was found to be linked to people that have poor walking speeds and poor performance in memory.
A report on dementia and tooth health can be found at the Journal of the American Geriatrics Society.
Dental health has also been linked to endocarditis, cardiovascular disease and pregnancy issues. Endocarditis is when the inner lining of a person’s heart is infected from bacteria from other parts of the body.
Bacteria in the mouth can make its way into a person’s bloodstream and attach to the heart.
Some research, and more needs to be conducted, has found that heart disease may also be affected by gum and tooth health. Oral bacteria may play a role in infections and inflammation that are known to cause stroke, clogged arteries and even heart disease.
Pregnant women who have bad dental health are also at risk of giving birth prematurely and low birth weight. This happens in cases where a person has severe periodontitis.
Neck and head cancers, arthritis and eating disorders may also be linked to oral health.
(09/13/2024)by Harcourt Health
More Information: N
Views: 400

Tips for Relieving Wisdom Tooth Pain
It’s probably been years since you’ve experienced toothache pain from getting your permanent teeth. However, that pain may return because of your wisdom teeth. These third molars can put pressure on your gums when they come in or develop infection from impaction when they have difficulty erupting through the gums, which can cause quite a bit of discomfort.
We’re going to talk about relieving wisdom tooth pain, including tips for recovery after getting them removed. We’ll also discuss home remedies for wisdom teeth pain and why you actually may not need to get your wisdom teeth removed.
What are Wisdom Teeth?
Wisdom teeth are the third molars that come through at the back of your mouth. They are the final adult teeth to come in and generally emerge in the late teens or early twenties, finishing your set of permanent teeth.

In humans’ evolutionary past, wisdom teeth were vital to grind and consume hard foods, like nuts and tough meats. In modern times, however, these third molars have little to no function, and wisdom teeth can become a problem if they affect the gums and cause pain, infection, or other dental problems.
Toothache pain can be mild or fleeting. It can also turn severe and more persistent. If your tooth pain will not go away, you should check in with your dentist.
When Do Wisdom Teeth Come In?
Most people see their wisdom teeth come in between the ages of 17 and 25. That’s about a decade or more after your first permanent teeth begin to grow. That can be a wide range and soreness from teeth developing in the gums can start long before teeth begin to erupt. Wisdom teeth coming in just underscores the importance of getting proper dental care throughout adolescence and early adulthood.

Granted, it may be harder to keep tabs on your child’s dental health or make time for an appointment when they leave home or go off to college. Still, they should do their best to brush and floss regularly and check in with their dentist to help avoid potential infection and limit the potential for wisdom tooth pain.
Does Everyone Have Wisdom Teeth?
Not everyone has wisdom teeth either because they never developed or, more likely, from getting them removed. While research has shown that 53 percent of the world’s population has at least one third molar, it’s somewhat common to have less than four as our bodies adapt evolutionarily to not needing these extra molars to grind hard foods. In fact, some people never develop wisdom teeth at all!
How Do You Know if You are Developing Wisdom Teeth?
You may experience some of the following symptoms when your wisdom teeth start to emerge. These could include:
Redness or swelling in the gums
Jaw pain or tenderness
Facial pain stemming from nerve pressure
Small, white spots emerging behind your second molars in the back of your mouth
If you have children, it will have been years since they experienced teething pain.So, should they start to experience some similar symptoms, it’s possible their wisdom teeth are starting to break through the gums and causing toothache pain.
A check-in with your dentist or orthodontist can help you find concrete answers. They’ll typically take X-Rays that can verify if the third molars are erupting and track their development from that point on.
What Are Some Types of Wisdom Tooth Pain?
You may experience wisdom tooth pain for different reasons. Most common among these are:
Soreness as wisdom teeth develop under the gums and prepare to emerge.
Pain from an infected wisdom tooth—see your dentist for recommendations on how to deal with this issue.
Pain from cavity in wisdom tooth or teeth.
Tooth sensitivity due to crowding or hitting other teeth when you chew.
If you are dealing with general soreness, you may look to relieve wisdom tooth pain with an at-home remedy. Otherwise, consult with a health professional to determine whether you need to get your wisdom teeth removed.
Tips for Relieving Wisdom Tooth Pain
Achy jawlines and teeth can prove quite frustrating. But how do you help relieve wisdom tooth pain? If you’re feeling discomfort because they are just starting to break through the gums, follow these tips for wisdom tooth pain relief.
Eat Soft and Cold Foods
Pain in your third molar can make it difficult to open your mouth and cause sensitivity when chewing. As such, it’s a good idea to work in softer and colder foods, like yogurt, applesauce and ice cream. Be sure to drink plenty of liquids as well.
Take Some Ibuprofen
As an anti-inflammatory, ibuprofen can help relieve wisdom tooth pain before and after removal. If you’ve undergone a procedure to get your wisdom teeth removed, your dentist may prescribe a specific amount to take after extraction. Stop using ibuprofen and speak with a doctor if you continue to experience pain.
Use a Toothache Gel
If your gums are sore from wisdom teeth coming in or your third molars are tender, try a toothache cream or gel to help relieve gum and tooth pain from wisdom teeth. Orajel™ 4X Medicated For Toothache & Gum Cream provides instant pain relief* for severe toothaches and painful gums. It also helps prevent infection and kills harmful bacteria. Orajel™ PM 4X Medicated For Toothache & Gum Cream offers similar relief powered by four active ingredients for fast topical pain relief*, plus chamomile.
Both products have a Ready-Open Tube Tip for easy access. If you prefer a gel to a cream, try Orajel™ 4X Medicated For Toothache Gel, which delivers targeted and long-lasting pain relief*.
*Up to 2 hours relief
Try a Mouth Rinse
Using a mouthwash or rinse may help soothe toothaches and gums. If you’re looking to relieve wisdom tooth pain and have yet to determine whether you need to have them removed, try Orajel™ Toothache Rinse. It’s the only double medicated rinse for the temporary relief of pain due to toothaches and minor irritation of the mouth and gums, or occasional minor irritation, pain, sore mouth and sore throat.
Note that you should only use an over-the-counter rinse or mouthwash before undergoing any procedures to have your wisdom teeth removed. If you’ve already undergone surgery, stick to any rinses your dentist may have prescribed for you. Alternatively, you might try rinsing with warm salt water, but do not start rinsing until the day after your procedure.
Keep Brushing Those Teeth!
You want to ensure you are brushing your teeth when your wisdom teeth are coming in. Additionally, if you’ve gotten your wisdom teeth removed, you should resume brushing teeth (gently) 24 hours after extraction, as directed by your doctor.
Given that your third molars are all the way back in your mouth, some people struggle to brush them properly. That can lead to plaque build-up and infection. It’s a good reminder to brush those teeth properly, even when you’re feeling wisdom teeth pain. Doing so may help prevent toothaches, decay or infection in the future.
Do You Need to Get Your Wisdom Teeth Removed?
You do not necessarily need to get your wisdom teeth removed. A dentist is likely to recommend surgery to remove one or more wisdom teeth if there are signs of impaction, infection, or decay, or if your molars have too much crowding.
Some wisdom teeth may need to be removed if they are trapped beneath the gums. This can cause infection and damage other teeth roots or bone support. Others that emerge partially through the gums can be hard to see and clean and thus attract bacteria, which may result in infection. Your dentist may also advise that you have full-grown wisdom teeth pulled if they create crowding in your mouth and damage nearby teeth.
How Do You Know if Your Wisdom Teeth Need to be Removed?
You may need to get your wisdom tooth removed if it becomes impacted. If a wisdom tooth is impacted, it is stuck below the surface of the gums. Impacted third molars come in at an odd angle because you don’t have enough room in your mouth for them to grow or develop normally.
One or multiple impacted wisdom teeth can cause numerous dental complications, including:
Wisdom teeth pain.
Infection.
Cavities.
Gum disease.
Damage to neighboring teeth.
However, just because you may have an impacted wisdom tooth or teeth does not necessarily mean you have to get them removed. If they are not causing you pain or showing signs of infection, your dentist or oral surgeon may not recommend getting them removed.
What are the Early Stages of a Wisdom Tooth Infection?
Pain, swelling and inflamed gums may be part of the early stages of a wisdom tooth infection. Other signs and symptoms may include:
Bleeding gums.
Unpleasant taste in your mouth.
Difficulty opening the mouth or swallowing.
Fever.
Bad breath.
If you or your teen experience any of these signs or symptoms, schedule an appointment with your local dentist.
When Should You Get Your Wisdom Teeth Removed?
According to the Mayo Clinic, dentists often feel it’s better to get your wisdom teeth removed at a younger age because the roots and bones connected to your teeth are softer. Most people get wisdom teeth removed between the ages of 17 to 25, when they first erupt through the gums. Should your teen begin experiencing wisdom teeth pain, you may look to get the impacted tooth or teeth removed sooner, based on your dentist’s recommendations.
How Late is Too Late to Get Your Wisdom Teeth Removed?
You can still get your wisdom teeth removed after the age of 50. However, the process is likely to be more painful.
The bone density in the mouth of full-grown adults increases over time, making pulling teeth a bit more daunting. You might also face a longer timeline for recovery. So, while it’s never “too late” to get wisdom teeth removed, you’ll want to do so earlier if it’s possible. Talk with your dentist about potential procedures and anything you might do to prepare.
(09/14/2024)by Orajel
More Information: N
Views: 413

Three Simple Changes That Can Help Improve Your Oral Health
Preventing oral health issues can seem like a simple enough responsibility. You take the time to brush your teeth, and floss, and try not to overindulge in sugary, sweet foods and drinks, and as a result, your risk for decay is lowered. The process of preventing smile trouble can be straightforward, but unfortunately, patients still find themselves in need of help with cavities and gum disease. Your Bellaire, TX dentist can support you during regular dental exams, which include a professional teeth cleaning. You still need to do your part between those visits – with a few smart changes, you can improve your smile care routine.
1. Reevaluate Your Brushing And Flossing Habits
If you are concerned about the health of your smile after experiencing an oral health issue, take time to reevaluate your dental care strategy. You should be brushing at least two times a day. Every time you brush, you should dedicate least two minutes to the process, and reach every part of your teeth. Flossing is also something you need to take care of on a daily basis. Flossing is most effective when you are consistent, and when you move the string enough to clear away bacteria at your gum line – this protects you against periodontal problems.

2. Choose Water Over Soft Drinks When You Enjoy A Meal
A simple change from soft drinks to water can make meals healthier for your smile. This reduces your sugar intake, while also making it easier to wash away food particles that might stick to teeth when you eat. Your diet soft drinks may lack sugar, but note that they can still cause problems due to their acidity. Dark colas also pose a problem for teeth stains, which can call for a teeth whitening procedure to fully address.

3. Plan Healthy Snacks At Home, And Avoid The Vending Machine
Your choices between meals may account for more smile trouble than you realize. If your regular snack at work is something you procure from your vending machine, consider replacing it with a healthy snack brought from home. You can select a lower calorie option that provides you with the energy you need, while taking less of a toll on your oral health.
(09/13/2024)by Contemporary Dental
More Information: https://contemporary-dental.com/2019/01/3-simple-changes-that-can-help-improve-your-oral-health/
Views: 320

Misaligned Jaw – Symptoms, Causes and Treatment Options
Jaw misalignment is an alignment condition where your upper teeth do not sit perfectly over the lower ones. Overbites, underbites, and crossbites are some of the most common kinds of jaw misalignments. Overbite is a condition where the upper set of teeth close ahead of the lower ones while the opposite happens in the case of underbites. A crossbite is a dental condition where the upper set of teeth sits inside the lower set. Each of these conditions can cause problems in basic functions like biting and chewing. In several cases, misaligned jaws can cause severe pain and result in various kinds of gum diseases. Let’s delve deeper into the misaligned jaw causes and understand how to fix a misaligned jaw.
Causes of Misaligned Jaw
Genetic reasons along with early childhood habits are some of the primary causes of a misaligned jaw. Several teeth alignment conditions can also result in jaw misalignment. Understanding the root cause of this condition can help in treating it better. Let us look into some of the main causes of a misaligned jaw.
Bruxism- Bruxism is a condition where a person clenches and grinds their teeth. This constant grinding can cause the teeth to move out of their normal position and can lead to inflammation and a crooked jaw.

Temporomandibular Joint (TMJ) Disorder- TMJ is a joint that connects the maxilla (upper jaw) and mandible (lower jaw). The disproportionate structure of TMJ or its misalignment is one of the main causes of irregular jaw shape.
Injury- Accidents and sports injuries are other common causes of a misaligned jaw. Physical contact sports such as boxing, martial arts, football, and rugby are some of the main contributors to jaw injuries.
Hereditary factors- Many patients are born with a misaligned jaw and to fix the jaws to their correct position, several doctors recommend solutions such as retainers and braces. Patients might also be advised to undergo surgery depending on the severity of the situation.
Misaligned jaw symptoms

Misaligned jaw symptoms can range from pain in the jaws to aches in the muscles surrounding them. The symptoms of a misaligned jaw can differ based on the severity of the condition. Let’s look into some of them.
Headache
Shoulder pain
Facial Swelling
Clicking sound made by the jaw
Change in the facial structure
Inability to open the mouth completely
Weakening of teeth
Jaws tightening
Pain in gums
Misaligned jaw treatment
Misaligned jaw treatment differs based on the severity of the condition. A misaligned jaw can be ignored by people in case of mild disorientation. However, in medium to severe cases, doctors might suggest some of the following options.
Braces- Braces are one of the most commonly used treatments for misaligned jaws. They hold on to your teeth firmly and guide them toward their appropriate position. Braces are attached firmly to the teeth and rectify the condition over some time.
Aligners- Aligners are the most popular form of dental treatment. One of the biggest advantages of aligners is that they are convenient to use and can be customized as per your jaw and teeth measurements. Aligners must be worn for 22 hours a day to witness the best results. Another beautiful aspect of using aligners is that one doesn’t have to follow any dietary restrictions and undergo treatment in a carefree manner.
Dental bridges- Jaw misalignment can also be caused due to missing teeth. This is where dental bridges step in and fill up the void in your mouth. A dental bridge helps in restoring bite, smile, and overall health. They provide great value aesthetically and instill confidence in the patient.
Jaw Surgery- Patients can choose to undergo jaw surgery if their jaw is severely misaligned. This option is usually used as the last resort and procedures like Maxillary osteotomy (surgery on the upper jaw) mandibular osteotomy (lower jaw surgery) or genioplasty (chin restructuring) can be performed on the patient.
(09/15/2024)by Flash Aligners
More Information: N
Views: 381

Did you know? An infected tooth can lead to multiple-organ-failure and death
It’s common knowledge that dental issues are cosmetic. But, do you know that ignoring dental disease can result in severe illness and even death? Yes, deaths due to tooth infections often make it in the headlines.
Dental infections are the most preventable and easily treatable medical conditions. However, adults and children in low-income groups find it difficult to access dental care.
Plus, people often fail to acknowledge the seriousness of oral health and illness. They avoid tooth extraction and let the decayed piece in place for years.
Infection’s journey from tooth to the brain

Besides severe pain, a decayed wisdom tooth can also result in facial swelling. If the disease from the infected upper-jaw tooth reaches the brain, the patient may experience a headache.
At this stage, the patient has no other options but to opt for antibiotics and tooth extraction. Failing to do so can even result in death; yes, you read it right, death!
Lack of preventative care combined with inaction despite infection
A combination of tartar, plaque, and harmful bacteria can trigger tooth decay. The condition shows several signs and symptoms. It develops in the grooves and crevices of your molars.

Biannual dental checkups and cleanings at a dental clinic eliminate the chances of developing advanced tooth infections.
Plaque and tartar formation creates a perfect environment for harmful bacteria. They feed on naturally found saliva sugar and multiply. These bad bacteria also release acid that demineralizes and erodes tooth enamel resulting in cavities.
If these holes are not filled on time, the bacterial infection reaches the pulp, tooth nerves, and blood vessels. The situation can escalate quickly if the untreated infection spreads in the brain or other body parts.
A pocket of pus and bacteria
A dental abscess often accompanies a tooth infection. The condition involves the formation of bacteria pockets and pus on gums, inside the teeth, or on the jawbone. It’s a sign that the harmful bacteria have reached the gumline.
The condition is easily diagnosable and treatable during the initial stages. But a delay in starting the treatment can result in serious medical consequences.
Patients are vulnerable to osteomyelitis, cavernous sinus thrombosis, cellulitis, parapharyngeal abscess, and even sepsis.
Put simply, severe infections can affect the person’s health by spreading beyond the face and neck.
What’s sepsis?
When tooth infection enters the bloodstream, it triggers a reaction from the immune system. Sepsis occurs when the immune system overreacts. If left untreated, the medical condition can lead to septic shock, and ultimately, multiple-organ failure.
Stage-wise treatment options
Filling up cavities
Painless and quick treatment is possible if cavities get highlighted and filled without delay.
In case of decay, dentists remove the same with the help of a small drill and fill the treated area to restore the chewing power.
Root canal
If the decay reaches the inner areas of the tooth, it needs a restorative treatment like a root canal.
As a part of the process, the dentist drills the infected areas of the tooth to remove accumulated bacteria and pus. Rubber-like material gutta-percha is used for filling the space post removal of infected tissues. A crown is placed on the tooth to cover it for restoring chewing power.
If the infection has reached the tooth end, your dentist can recommend an additional process called an apicoectomy. It involves a minor surgery on the gums to remove the infected root and surrounding tissues.
Extraction
In some cases, dental decay completely damages the tooth and reaches the root. There is no other alternative option but to extract the dead tooth.
Antibiotics for controlling the infection
Dentists assess the severity of the infection and might prescribe strong antibiotics to stop it from spreading.
During treatment, the professional can ask you to switch to a different medication.
Hospitalization
Parapharyngeal abscess cases require pus draining from the infection site. The process may require hospitalization.
Patients who need surgical intervention to remove infected jawbone portions (apicectomy) also need a hospital stay. Specialists use intravenous drip to administer antibiotics.
Sepsis can cause sudden blood pressure drop, multiple organ failure, and even death. Thus, sepsis patients need hospitalization and ICU treatment with surgery, dialysis, and intravenous antibiotics, depending on the severity of the condition.
What’s the best option to avoid trouble? Simply practicing oral hygiene habits can help you stay ahead of the decay.
Which factors influence the type of treatment for an infected tooth?
The location of the abscess
The extent of the infection
Areas where the disease has spread
The infection’s impact on the immune system
Signs and symptoms to worry about
Some signs indicate if the dental infection has reached other areas of the body. Patients with the following symptoms require immediate medical attention:
Swelling of cheeks or overall face and neck
Burning sensation on facial skin
Painful tongue or mouth
Slight loss of vision or double vision
Severe one-sided headache
Fever
Difficulty in breathing and confusion
The endnote:
Why ignore even a tiny crack in the tooth and then pay for a complicated dental surgery later?
Maintain oral hygiene habits, and get your infected teeth treated on time. Most importantly, don’t delay the extraction of severely decayed teeth.
(09/14/2024)by TruCare Dentistry
More Information: https://www.trucaredentistry.com/blog/did-you-know-an-infected-tooth-can-lead-to-multiple-organ-failure-and-death/
Views: 359

Scary Causes and Symptoms of Epiglottitis
If you opened your news feed over the weekend, you were likely hit with some pretty scary health news from the celebrity world: Comedian, Sarah Silverman, was admitted to intensive care with Epiglottitis. Don’t worry, “What the heck is Epiglottitis?,” were my exact thoughts as well.
Thankfully, Epiglottitis is a fairy rare (particularly in adults) yet life-threatening condition that can occur over a period of days when the tiny cartilage flap (called the epiglottis), located at the base of the tongue, which covers the windpipe (or trachea) becomes inflamed and blocks air flow, according to Healthline.com. Silverman, like many patients, mistook this serious condition as mundane throat discomfort, the type that can occur with allergies, voice over-usage, or drinking a too hot beverage. Please note that the symptoms for Epiglottitis differ slightly for children and adults, and a Hib vaccine can be administered during childhood to help prevent the bacteria that causes most Epiglottitis cases in young children to occur…
1. What Characterizes Epiglottitis?
The Mayo Clinic explains that Epiglottitis is a condition that can occur over a period of days in older children and adults (alternatively, it can come on suddenly in small children). This means you might feel a slight airway restriction, however, your life may not be in jeopardy until the epiglottis (which is that small flap of cartilage covering over your windpipe) swells completely.
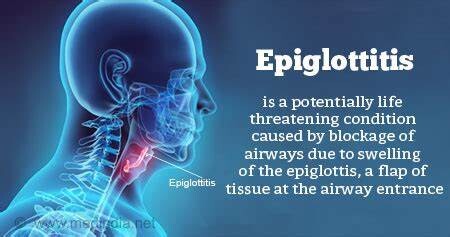
Once this trachea covering swells completely, it can completely block any air flow to the lungs. However, patients may be reluctant to consider Epiglottitis a medical emergency since the symptoms can be gradual and flu-like (i.e., sore throat, difficulty swallowing, raspy voice, etc.).
2. What Causes Epiglottitis?
According to Healthline.com, even though this condition is considered rare, a bacterial infection (caused by Haemophilus influenzae type b, or Hib) during childhood is the most common trigger of Epiglottitis. This type of bacteria is typically contracted when a patient inhales Hib germs from an infected person’s cough or sneeze.
However, the Mayo Clinic suggests that Epiglottitis can also occur due to drug use (i.e., smoking crack cocaine), a throat injury (puncture, due to drinking hot beverages, or from swallowing an object that causes injury), or due to the contraction of a viral, fungal, or bacterial infections (i.e., Streptococcus A, B, or C; shingles, chicken pox, yeast infection, severe diaper rash, pneumonia, or meningitis).

3. Difficulty Swallowing
Both older children and adults with gradually worsening Epoglottitis may express difficulty or pain when swallowing in the early stages. Oftentimes, drooling occurs when patients experience trouble swallowing.
The pain and inflammation of the epiglottis may also be more severe when leaning back or lying down, but upon sitting upright or leaning forward symptoms may seem to subside temporarily.
4. Sore Throat
As mentioned, the symptoms of Epiglottitis can develop over a few days, and become rapidly worse very quickly in older children and adults. Your throat may sound scratchy and your voice may become hoarse (similar to laryngitis) at first.
However, keep in mind that a typical sore throat due to a cold or flu will improve within a week. However, if you experience a sore throat that becomes painful and exceedingly worse, it should demand medical attention, especially if it’s accompanied by the other symptoms listed in this article.
High Fever
For children, a fever with chills is a sign to parents that something is wrong. In this case an elevated temperature soaring to 100.4 degrees Fahrenheit (or above 38 degrees Celcius) may indicate the type of existing viral, fungal, or bacterial infection that can trigger Epiglottitis.
Small children, and even adults with high fever, may appear irritable and restlessness. However, in the case of Epiglottitis, fever will typically accompany other symptoms listed in this article.
6. Abnormal Breathing
Breathing difficulty or breathing abnormalities are the major concern for both children and adults with Epiglottitis, according to NHS Choices (U.K. National Health Service). Breathing may present as high-pitched, noisy, muffled, or raspy in nature.
Children’s breathing may be “stridor” or make a high-pitched, vibrating, musical sounds that indicate a larynx or trachea obstruction. Both adults and children may be unable to catch their breath and resort to mouth breathing.
7. Bluish Skin/Oxygen Deprivation
If an adult or child presents bluish colored skin, this discoloration may indicate oxygen deprivation due to a swollen or blocked airway.
In this case, emergency care should be considered vital and immediate. If you suspect Epiglottitis, or you or a loved one has trouble swallowing/and or breathing seek out the neare
st hospital emergency department as soon as possible while keeping the patient in an upright position to ease breathing.
(09/17/2024)by Emily Lockhart
More Information: N
Views: 290

What Is Uvulitis?
Hanging from the roof of your mouth and at the back of your throat, you will see a protrusion of pink-colored tissue in the shape of a drop. This is known as the uvula. The uvula usually ascends with the soft palate to prevent food and liquids from entering the nose while swallowing. It also aids in a person’s speaking ability. Finally, it can also trigger the gag reflex and prevent choking.
When the uvula becomes swollen, it can cause a foreign object sensation in the back of your throat. This condition is called uvulitis. Swelling of the uvula can occur together with swelling of the surrounding tissues such as tonsils and the throat. A person with uvulitis may also have a sore throat and swallowing may become difficult or painful. If you feel like you might have uvulitis, you can check this out by opening your mouth in front of a mirror and saying “ah”. If your uvula is swollen, it will probably be enlarged and the mucosa will exhibit a red color. But what causes it? Here are 10 swollen uvula causes.
Uvulitis can occur in any person, no matter the age or gender. However, the condition is more common in children than in adults. Some people are also more likely to get uvulitis than others.
Such people include those who have allergies, smokers, those who are constantly exposed to irritating chemicals and other irritants, and those with a weak immune system that makes them vulnerable to infections. If you are at risk of getting uvulitis, especially due to allergies, discuss your condition with a doctor.

Gastroesophageal Reflux Disease (GERD)
Almost half of adults in the United States will experience symptoms of gastroesophageal reflux disease (GERD), at least once a month. GERD is a consequence of the backing up of gastric acid (above the normal limit) into the esophagus, which is the tube that connects the mouth with the stomach. This usually happens after a meal, and it causes symptoms with or without damaging the lining of the esophagus. Examples of typical GERD symptoms are heartburn, regurgitation, and difficulty swallowing.
Additionally, the acid from the stomach can flow upwards and reach the throat and the larynx (voice box), causing a subtype of GERD known as laryngopharyngeal reflux (LPR). Common symptoms of this condition include sore throat, hoarseness, cough, and a lump-sensation in the throat. When the uvula comes into contact with acid reflux in LPR, it can become red and swollen. If you have uvulitis, and suspect of acid-reflux as a possible cause, consult with a specialist for proper diagnosis and treatment.
Infections

Infections, especially those caused by viruses, and bacteria can also lead to uvulitis. Such infections include the common cold, croup, mononucleosis, strep throat, tonsillitis, and STDs.
When these infections affect the oral cavity, they can irritate any of the tissues here, including the uvula and the throat. Cases due to an infection like the common cold are usually short-lived, and go away within a few days.
Trauma
Trauma to the uvula can also cause uvulitis. Such trauma can result from conditions such as GERD, whereby stomach acid injures the throat, including the uvula.
Trauma to the uvula can also occur during surgical procedures such as removal of the tonsils or the insertion of a tube to deliver oxygen into the lungs.
Bacterial Infection
The most common bacteria that affects the throat is streptococcal bacteria. Specifically, Streptococcus pyogenes causes the inflammation of the pharynx and tonsils, leading to what we know as strep throat. Uvulitis can develop in severe cases of strep throat. If you have tonsillitis, for instance, the back of your throat including the uvula can be swollen because of the infection and inflammation. Sometimes, only one tonsil becomes inflamed along with your uvula. In severe cases, this can lead to deviation of the uvula away from the affected tonsil.
Genetics and Uvulitis
Genetics may play a part in some cases of uvulitis. A rare condition called hereditary angioedema can make your throat, face, hands, feet, and uvula swell.
Another rare condition leads to an elongated uvula that is larger than normal. However, although the condition resembles uvulitis, it is not uvulitis, and the only way to treat it is through a surgical intervention known as uvulectomy.
Diagnosis of Uvulitis
Upon visiting your doctor, they will interview you to get a history of your condition. It is important that you inform the doctor of any related symptoms including colds, cough, fever, and abdominal pain. Other important information includes any new foods you have consumed, exposure to chemicals or other materials, and medication you have taken for the condition, including over-the-counter drugs and antibiotics. The doctor will carry out a physical examination and may also swab the uvula or the throat for a laboratory examination.
Your doctor may also ask for a blood test to see whether you have an infection or not and to rule out some infections. In some cases, all these tests can be inconclusive and you may need to see an allergist to assess your case. Provide the allergist with your blood and skin tests to be able to identify the substances and foods that may cause an allergy.
Home Remedies for Uvulitis
If you have uvulitis, or a sore throat, your body is telling you that there is something wrong. Some home remedies can help soothe your swollen uvula and sore throat. These include sucking on ice chips or frozen juice bars, or ice cream. You can also try gargling with warm salt water.
Getting adequate sleep, and sleeping in comfortable surroundings, free from irritants, can also help your body recover and fight any infections. You should also keep your throat and body hydrated by sipping on warm water throughout the day. This will reduce the irritation of your throat.
Medical Treatment for Uvulitis
Treating uvulitis depends on the cause of the condition. Once the cause is resolved, uvulitis will also clear. Some medical conditions, like the common cold, can go away without treatment. Uvulitis due to such conditions clears up once the infection goes away. If, however, the condition causes a lot of discomfort, you can take pain medication and wait for the swelling to reduce. Cases of bacterial infection are treated with antibiotics. Make sure that you complete the course of treatment even after you get relief from the symptoms.
If uvulitis is a result of an allergy, seek a doctors assistance to determine the allergen so you can avoid it. Antihistamines or steroids are used to treat allergies. Uvulitis due to hereditary angioedema can be treated with C1 esterase inhibitors, plasma kallikrein inhibitor, bradykinin receptor antagonist, or androgens.
Long-Term Outlook for Uvulitis
Uvulitis is an uncommon condition that is usually a result of an underlying problem. For this reason, once the cause is dealt with, uvulitis resolves without further treatment. Home remedies, including avoiding trigger foods and other substances and keeping your throat hydrated, can also help.
Serious uvulitis is treated with medication. Discussing your condition with a doctor can help determine the best management plan depending on your condition.
(09/17/2024)by 10Faq
More Information: https://10faq.com/health/what-is-uvulitis/3/
Views: 413

Tooth Sensitive to Cold: Causes, Symptoms and How to Deal With It
Some people experience tooth sensitivity. Tooth sensitivity occurs when you feel pain, discomfort, or irritation when your teeth contact food or beverages at extreme temperatures. Therefore, you may feel pain when you eat ice cream or drink hot coffee.
Dentin hypersensitivity or tooth sensitivity is any pain or discomfort in the teeth due to hot or cold temperatures. For most people, cold temperatures make their teeth ache. Additionally, the condition can affect one or several teeth.
For some people, the symptoms are temporary and eventually heal. For others, it is a chronic problem that affects their everyday life. Even if it is chronic, it is not a life sentence. There are many things you can do to manage tooth sensitivity due to cold temperatures.

But first, learn about what causes the condition, some of the symptoms, and what experts say about tooth sensitivity.
What Causes Tooth Sensitivity to Cold?
Several things cause your teeth to be sensitive to cold temperatures. The most common are:
Tooth decay or gum disease. If your teeth hurt when you eat cold foods and beverages, you could have tooth decay or gum disease. One of the early symptoms of these two conditions is teeth sensitivity to cold temperatures. Sensitivity often starts at the gum line. Therefore, you will feel a weird sensation before it graduates to tooth sensitivity. If your gums recede, then it could also mean sensitivity to cold temperatures.

Effects of oral products. Some people use oral products such as whitening creams and hardening solutions to improve their smiles. However, excessive use of these products leads to tooth sensitivity, especially to cold temperatures. It happens when the oral products abrasively affect the enamel.
Brushing too hard. Being too passionate about cleaning your teeth could lead to tooth sensitivity. Brushing too regularly or applying too much pressure when cleaning your teeth erodes the enamel. This leaves your dentin exposed, leading to tooth sensitivity.
Bruxism. Bruxism is excessive jaw clenching and teeth grinding. Many people develop this habit due to anxiety and stress. It leads to headaches and facial pain. Long-term effects include wearing down your teeth. This makes them sensitive to the cold.
Cracks in the teeth. Your teeth can sustain tiny cracks that grow with time. The cracks are a direct pathway to the nerves. Nerve exposure causes tooth sensitivity.
Gastroesophageal reflux (GERD). Gastroesophageal reflux or GERD is a gastric condition that causes acid to come up from the stomach and esophagus. This exposure to acidity wears down the teeth leading to sensitivity.Excessive vomiting. Conditions that cause excessive vomiting, such as gastroparesis and bulimia, could lead to tooth sensitivity. The acid in vomit wears down the enamel leaving the teeth exposed.
Symptoms of Tooth Sensitivity
Pain or discomfort. You will experience pain or discomfort when you take cold beverages or foods. Most people cannot eat ice cream or drink cold water.
Changes in taste. You may experience changes in taste. There are notable changes in the way things taste, especially sweet and salty foods.
Pus or discharge. Sometimes tooth sensitivity comes with pus or other types of discharge such as blood. This is often a sign of an underlying condition.
Redness and swelling in the gums. This is often in cases of over-brushing, using too many oral products, and applying too much pressure as you clean the teeth.
You may also experience symptoms in other parts of the body, depending on your condition. For example, GERD comes with indigestion and stomach discomfort on top of tooth sensitivity.
Treatment Options for Tooth Sensitivity
Professionals have a few treatment options for people with chronic tooth sensitivity. These treatments are:
Applying fluoride. A professional will apply fluoride to exposed areas with cracks and holes. This helps to strengthen the enamel and dentin. This will reduce sensitivity, and you can feel less pain when eating cold foods.
Gum grafting. The dentist may cover receding gums with gum grafting. This ensures there is less exposure of the nerve endings. It will improve sensitivity to cold foods.
Root canal. In exceptional cases, the dentist may also treat the sensitivity via root canals. This is for progressed cases with underlying issues and conditions.
Sealants. And finally, the dentist will use sealants on the surface of the teeth to treat sensitivity. Sealants seal the tooth to create a barrier that overcomes tooth sensitivity. Therefore, you will be able to eat cold foods more comfortably.
How To Deal With Tooth Sensitivity
If you would like to deal with tooth sensitivity at home, you can. Most people do not go to the dentist until it is necessary. There are natural ways to ease the symptoms and improve your condition at home. So follow these tips to see results.
Incorporate a healthy diet. Avoid acidic foods because they will erode your enamel quickly. Instead, strive to provide your teeth with nutrients for strength and enamel preservation. Dairy and dairy products are great for strong teeth. Additionally, vegetables help to keep gums strong. And finally, carrots and healthy hard foods will moisten your mouth and make it better at fighting bacteria.
Manage stress levels. Learn to manage your stress and work off some of your anxiety. It will keep you from grinding your teeth and clenching your jaw. This preserves the other layer of your teeth.
Be gentle with your teeth. Avoid brushing your teeth too aggressively. You will experience less sensitivity and soreness. Also, switch out your toothbrush for one with softer bristles. And do not use too much toothpaste when you brush two times a day. Additionally, go easy with the whitening products and other oral products.
Do not give up on eating ice cream just yet! You can ease the symptoms of tooth sensitivity and finally enjoy a cold drink. Just be sure to follow these tips actively. If you realize that your symptoms are chronic or have other body issues, visit a dentist for a proper diagnosis. Additionally, follow the expert advice of a qualified dentist for a healthier smile.
(09/18/2024)by All About Smile Dental Group
More Information: https://allaboutsmiledentalgroup.com/blog/tooth-sensitive-to-cold-causes-symptoms-and-how-to-deal-with-it/
Views: 307

What are the Steps to an Oral Examination?
When you visit your dentist for a professional cleaning and oral examination, many services will be provided. While professional cleaning may be the most obvious service provided, the examination is equally crucial, as you’ll be fully screened for a variety of conditions that can potentially impact not just your oral health, but your overall health as well. Here are all of the steps your dentist, hygienist, and support staff will take during your oral examination and cleaning.
Medical and Oral Health History
Your dentist, hygienist, or dental assistant will first ask you about any changes to the function of your jaw or teeth, or any newly diagnosed health conditions. They may ask about new medications, any new onset of tooth or gum sensitivity, headaches, bleeding, etc. The information you provide will be recorded in your dental record.
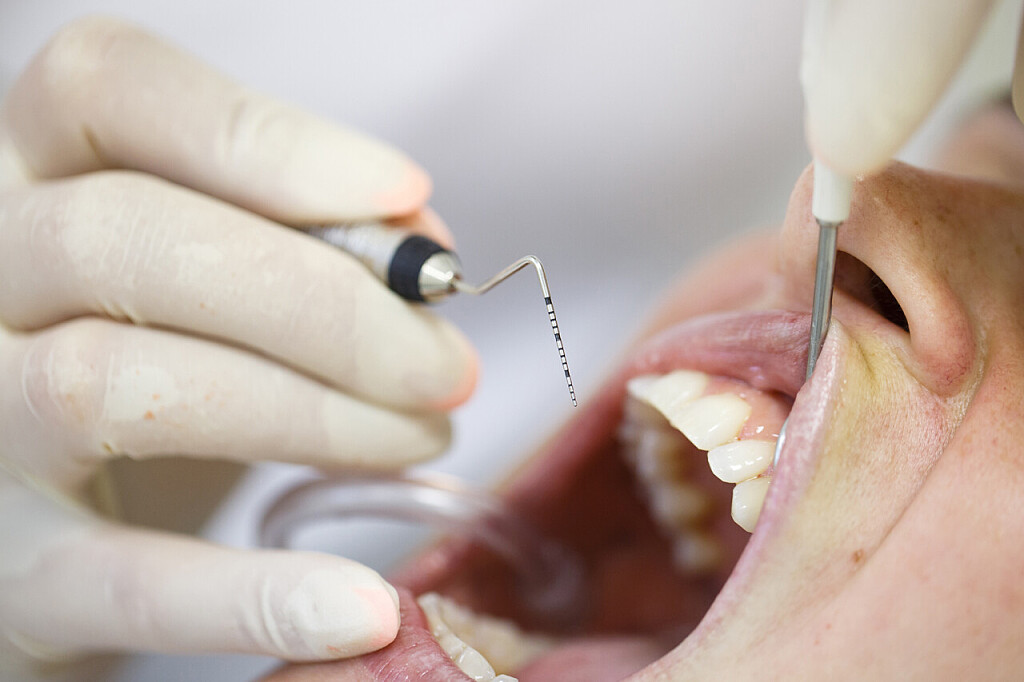
Plaque Removal and Polishing

Your hygienist or dentist will begin removing plaque and tartar buildup on the teeth. Plaque tends to accumulate between teeth, at the gum line, and between teeth. They will use an ultrasonic device to loosen larger pieces of plaque first. Then, a tiny metal tool (hand instrument) will be used to scrape additional plaque from the teeth.
They will then thoroughly floss between all of your teeth, before polishing your teeth with a spinning polisher that will remove any further plaque and leave your teeth feeling clean and smooth.
Preventative Screenings (Occasional)
Your dentist will determine how often you should have X-rays of your teeth and jaws. You are unlikely to need X-rays at every appointment. But if it’s been a year or more since your last x-rays, your dentist may need them.

Likewise, if they need to see beneath the surface you may need X-rays. Incidentally, today’s digital X-rays are entirely painless and take just minutes. They also expose you to far less radiation than older, traditional X-rays. They are available to your dentist for viewing immediately.
X-rays help identify tiny cracks in teeth, cavities in their earliest stages, and loss of bone, indicating gum disease.
Oral Examination
The oral examination will be conducted by the dentist. During this comprehensive examination, the dentist will be looking for any signs of disease, decay, jawbone deterioration, and gum recession. They will look for symptoms including changes to soft tissues, lesion development, or other abnormalities.
They will also thoroughly examine the condition of your teeth. This includes looking for signs of weakening or softening enamel and dentin. They will look for excessive wear on the teeth (worn grooves) indicating jaw clenching or teeth grinding. Your dentist will also look closely at your gums, measuring periodontal pockets, and ensuring that the gums are not swollen or bleeding, indicating gum disease.
Your dentist will also evaluate the function of your jaw, prompting you to open and close your mouth. They may feel the jaw joint as you do so, to confirm the joint is not clicking, and to confirm proper alignment.
Finally, your dentist will conduct a visual inspection of the head and neck to look for any signs of abnormalities that indicate further testing should be scheduled.
If no problems are found during your oral examination and cleaning, you’ll be instructed to return in six months for your next cleaning and exam. If problems are identified during your appointment, your dentist will explain all treatment options and design a custom plan for your care.
(09/18/2024)by Carmel Dental Associates
More Information: https://www.carmeldentalassociates.com/what-are-the-steps-to-an-oral-examination/
Views: 364

How To Stop Grinding Teeth In Sleep Naturally
How To Stop Grinding Teeth In Sleep Naturally: Even though many people are unaware that they grind their teeth, teeth grinding, or bruxism, which affects around one in ten adults, is a problem that should not be overlooked. In this article, I will provide you ten remedies to prevent you from Grinding Teeth during sleep and more.
Let’s get started!
What is night-time teeth grinding?
Teeth grinding (bruxism), a common instinctive response to stress, anxiety, or anger, can occur either while awake or asleep, but it is far less frequently observed during sleep. This is primarily due to the fact that many people are unaware they are doing it.

However, failure to recognize bruxism might have grave consequences. Because people are unaware of the force of their bite during sleep, the force exerted when forcefully clenching the jaw and teeth can cause major problems with both the teeth and jaw.
Studies have revealed that up to 250 pounds of force can be exerted during bouts of sleep bruxism, often known as nighttime teeth grinding. However, many people do not understand the consequences of their activities until it is too late.
How prevalent is tooth grinding during night?
Statistics on sleep bruxism are often difficult to get because many individuals are unaware that they grind their teeth during sleep. However, we have not been deterred. According to studies, 6% to nearly 50% of children experience nighttime tooth grinding to some degree.

This is partly attributed to the fact that a complete set of adult teeth takes between 17 and 25 years to erupt from birth.
Cause of Grinding Teeth In Sleep
Although there is rarely a single cause for nighttime teeth grinding, the disorder is frequently related with stress and worry. It is speculated that this is due to the fact that when we are stressed, our bodies accumulate a great deal of tension throughout the day, and those with sleep bruxism tend to release this tension by grinding their teeth during sleep.
Additionally, teeth grinding can be caused by a variety of sleep disturbances and preexisting conditions. In recent years, numerous studies have connected sleep bruxism to disorders such as obstructive sleep apnea, sleep paralysis, Parkinson’s disease, epilepsy, and ADHD.
Additionally, certain medicines are frequently related to tooth grinding. This covers both legal and illegal substances, such as antidepressants, alcohol, nicotine, and caffeine.
What impact does tooth grinding have?
Long-term, untreated teeth grinding can cause severe damage to the teeth, causing them to feel excruciating pain or possibly disintegrating them over time. In addition, fillings, crowns, and implants can deteriorate with time, posing a potentially expensive and unpleasant repair issue.
Sometimes, one of the most well-known effects of tooth grinding does not impact the individuals themselves. Similar to the sound of nails on a blackboard or a newborn wailing, the sound of teeth grinding is one of those sounds that affects many individuals, including spouses.
10 Natural Remedies to Stop Grinding Teeth In Sleep
Watch what you consume
What you consume as part of your diet can make a significant difference in your ability to manage sleep bruxism. Hard foods like nuts, popcorn, and many candies should be avoided at all costs, while sticky, difficult-to-chew foods such as peanut butter should be approached with extreme caution.
However, foods rich in magnesium, such as leafy green vegetables, yogurts, and brown grains, should be chosen due to their capacity to reduce inflammation during sleep.
Drink warm milk
Drinking warm milk with turmeric can be of great assistance when attempting to overcome teeth grinding-related sleep disturbances organically. This is largely due to the nerve-relaxing impact of tryptophan, an amino acid derived from milk, and the anti-inflammatory and pain-relieving properties of turmeric, a well-known spice.
Avoid alcohol and caffeine
As previously stated, coffee and alcoholic beverages should be avoided when attempting to overcome sleep bruxism. This is due to the effect of these chemicals on disrupting sleep patterns, causing hyperactive jaw muscles and teeth grinding.
Adopt the use of essential oils and aromatherapy
Stress is the most prevalent cause of sleep bruxism, and essential oils might be your best ally in reducing it. Lavender, cedarwood, bergamot, and chamomile have been demonstrated to have notably soothing effects on the brain, and are extensively employed in a variety of aromatherapy-based treatments. Therefore, purchasing an oil diffuser to alleviate your nighttime teeth grinding organically could be a wise investment.
Lavender oil should be rubbed into the jaw
A few drops of lavender oil massaged into the underside of the jaw before bedtime can help release any tension that may have subconsciously accumulated in the mouth over the day. In addition, the circular motion will encourage your mouth to relax, allowing you to fall asleep in a more natural state of relaxation.
Perform meditation
Numerous studies conducted over the years have proved the positive impact of mindfulness on mental health, with practices such as meditation and breathing exercises being especially effective at reducing feelings of stress and anxiety. It has also been demonstrated that meditating to soothing noises, such as ocean waves, raindrops, or traditional white noise, calms the autonomic nervous system, helping to decrease breathing, reduce heart rate, and increase sleeping efficiency.
Get into yoga
Yoga has been proven to be particularly effective at reducing the inflammatory symptoms associated with sleep bruxism. While most forms of exercise can assist to alleviate sleep bruxism in some way, yoga has been found to be particularly effective.
Practicing yoga positions that focus on stretching the neck, jaw, and mouth region, such as the ‘eyes around the clock,’ ‘camel,’ and ‘bridge’ poses, for instance, could help relieve facial tension and inhibit nighttime teeth grinding in a more natural way.
Consider herbal tea
Since nighttime teeth grinding is exacerbated by emotions of nervousness and tension, consuming non-caffeinated herbal tea – such as green or chamomile tea – can be an excellent way to relax your mind and body, relieving the pent-up sensations of stress that are commonly connected with the problem.
Apply a warm compress
Using a hot cloth, compress, or heating pad on a regular basis has been demonstrated to relax the muscles surrounding the teeth, jaw, mouth, and neck. This, in turn, increases the blood supply to these areas, improves circulation, and reduces the potentially detrimental consequences of teeth grinding during sleep.
Wear a Mouthguard or Mandibular Repositioning Device
Mouthguards or MRDs can stop teeth from grinding during sleep. They create a barrier or reposition the jaw to prevent grinding. Mouthguards cushion the teeth and reduce damage, while MRDs move the lower jaw forward to keep the airway open. However, these devices don’t address the underlying cause of teeth grinding. It’s important to seek professional help to develop a treatment plan.
Which natural treatment for nighttime teeth grinding is best for me?
It is important to first seek a professional evaluation from your dentist to determine the severity and cause of your nighttime teeth grinding, also known as bruxism. Once the underlying cause has been identified, appropriate treatment options can be recommended.
In terms of natural treatments, there are several options that may be effective for some individuals. These include stress-reducing techniques, such as meditation or deep breathing exercises, as stress is a common trigger for teeth grinding. Additionally, establishing a relaxing bedtime routine and ensuring adequate sleep may also help reduce nighttime teeth grinding.
It is important to note that while natural treatments may be helpful for some individuals, they should not be used as a substitute for professional dental or medical care. A dentist or other healthcare provider can provide personalized recommendations and monitor the effectiveness of any treatment plan.
Conclude
In conclusion, while there are several natural remedies that may help to alleviate nighttime teeth grinding, it is always advisable to consult a dental professional for an accurate diagnosis and treatment plan.
(09/19/2024)by Spring Orchid Dental
More Information: https://springorchid.com.au/how-to-stop-grinding-teeth-in-sleep-naturally/
Views: 360

