Dentists Journal
Top Ten Stories of the Week
8/31/2024
All Dentists Journal · Previous Week · This Week · All Time List · Headlines

What Causes Submandibular Gland Swelling?
Most of us treat our salivary glands with an "out of sight, out of mind" mentality. But if something goes wrong with them, we'll quickly notice the problem. We rely on these glands to supply the saliva we need to chew, swallow and speak and to wash food debris away from our teeth. Submandibular gland swelling can be associated with dry mouth, infection and other conditions. However, most causes of gland swelling can be treated.
Where Are the Submandibular Glands?
Firstly, what is the submandibular gland? There is one walnut-sized submandibular gland on each side of the face, just in front of the curve of the lower jaw at the back of the mouth. Along with your other salivary glands, these glands supply saliva that contains enzymes to help break down food and minerals that reduce the damaging effects of food acids on your tooth enamel. Saliva also makes the food you chew wet and easy to swallow.
Causes of Submandibular Gland Swelling
If you feel swelling underneath your lower jaw, it could be a swollen submandibular gland. Swollen submandibular glands are usually caused by tiny stones blocking the ducts that channel saliva into the mouth. According to the Merck Manual, these stones can develop from the salts in saliva, especially if a person is dehydrated. When a stone blocks a salivary gland, a condition known as sialolithiasis, an individual may experience swelling and pain over the affected gland. Why these stones form isn't clearly known, though they can be associated with liver disease and gout. According to The Journal of Medical Research, sialolithiasis is the most common salivary gland disease, and the submandibular gland is affected in 83 percent of cases.
Salivary gland infections can result from blocked ducts. In these cases, swelling of the gland may be accompanied by redness and pus.
More rarely, salivary gland swelling occurs due to a tumor. Merck Manuals explains that swelling caused by a cancerous or noncancerous tumor on the salivary glands may be firmer than swelling caused by an infection. A cancerous tumor will likely be very hard and fixed to the gland tissue, while a noncancerous tumor may be movable.
See your dentist to determine what's causing your submandibular gland swelling. They will help you put an effective treatment plan in place.
Treatments for Swollen Salivary Glands
Early treatment of a swollen salivary gland — particularly when caused by a stone — could save you from developing an infection. The National Health Service recommends increasing your saliva production by drinking plenty of water and chewing sugar-free gum. The Government of Alberta suggests gently massaging the stone to help dislodge it.
If you are unable to treat it at home, your doctor or dentist may be able to push the stone out by pressing the submandibular gland or pull it out by using a small instrument, according to Merck Manuals. In rare cases, the stone may need to be removed surgically. If you suffer from a condition that causes salivary gland stones, receiving treatment to alleviate other symptoms may also reduce your risk of developing stones.
If you have an infection in your submandibular gland, your doctor can prescribe antibiotics and, if necessary, drain any pus from an abscess. Swelling caused by a tumor can be addressed by removing the tumor through a surgical procedure. Cancerous tumors should be treated urgently and will likely require monitoring.
To ease the pain of submandibular gland swelling, apply a warm compress to the gland area and rinse your mouth with salt water.
How to Prevent Salivary Gland Swelling
Maintaining a thorough oral care routine reduces mouth bacteria and is an effective first step in preventing swollen salivary glands. Increase your water intake and avoid smoking and using chewing tobacco, because these habits may increase your risk of mouth infections.
Submandibular gland swelling may be caused by a blocked salivary gland that can be easily treated. However, make sure to see your doctor or dentist for an accurate diagnosis to assess this oral care condition.
Oral Care Center articles are reviewed by an oral health medical professional. This information is for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your dentist, physician or other qualified healthcare provider.
(08/23/2024)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/threats-to-dental-health/what-causes-submandibular-gland-swelling
Views: 369

What Happens If You Have Your Uvula Removed?
If you have your uvula removed, it will be replaced with a small tube that is attached to the back of your throat and runs down through your neck. This tube is called a stoma and is used to drain saliva that collects in the tissue around the opening of your mouth.
The stoma will be visible just below your chin, but typically it doesn’t cause much of an aesthetic problem – it looks similar to a dimple or a birthmark.
In most cases, the stoma may take up to six months to heal after surgery. During this time, you may experience some discomfort when moving your tongue or swallowing fluids.
The recovery process for having your uvula removed varies from person to person, but most patients are able to eat solid foods within three weeks of surgery and return to work within two weeks after their procedure.
The uvula is a small piece of flesh that hangs down from the back of your nose. It’s normal to have one and it usually doesn’t cause any problems.
But sometimes the uvula can become enlarged or infected and may need to be removed.
If you’re having surgery to remove your uvula, the surgeon will make a cut in your mouth or throat (pharynx). They will then remove the uvula and stitches may be used to close any wounds. The procedure takes about 20 minutes, but you will need to stay in hospital for 2 days after your surgery.
The uvula is a small piece of tissue that hangs down from the back of the roof of your mouth. The uvula is sometimes called a “grape.”

There are several reasons that people have their uvula removed:
To prevent snoring
To treat sleep apnea (a condition in which breathing stops during sleep)
When the uvula becomes enlarged and obstructs breathing
If you have had your tonsils removed, you may need to have your uvula removed as well because it can become infected or swollen after surgery.
The uvula is a small structure that hangs down from the back of the soft palate. It’s attached to the bottom of your tongue and helps push food upward when you swallow.
The uvula can cause discomfort as you eat, drink and talk. The most common problem is an enlarged uvula. This may happen because of repeated trauma or infections in the throat or mouth, such as tonsillitis (sore throat).
Some people have a large or inflamed uvula, causing them to snore loudly and feel as though they have something stuck in their throat. In some cases, the hangnail-like tissue in the back of their mouth may bother them so much that they can’t tolerate eating certain foods like popcorn or chewing gum due to the added pressure on their throat.
If your uvula is large or prominent enough to cause problems with swallowing and breathing, then removal may be an option for you.
Is it good to remove uvula?
No, it is not good to remove uvula. The Uvula is a small piece of tissue at the back of the mouth. It hangs down and covers the opening to your throat, which is called the pharynx.
The main function of the uvula is to stop food from entering into your nasal passages while you are swallowing. It also helps you speak and can be used as a tool for whistling or singing.
Removing your uvula will only affect your appearance and make it difficult for you to speak clearly or whistle loudly. It does not cause any medical problems like sleep apnea or snoring.
It is not a good idea to remove the uvula, even with a tonsillectomy. The uvula serves as a protective barrier against bacteria entering the larynx and pharynx. If it is removed, there will be a greater risk for infection.
The primary purpose of removing an enlarged uvula is to alleviate breathing problems. However, there are other ways of resolving this issue without resorting to surgery, such as using steroid sprays or taking antihistamines.
The uvula is a small piece of tissue that hangs down from the roof of the mouth. It’s connected to the back of the throat by a thin strip of flesh called the frenulum. The purpose of the uvula is to help you swallow.
The uvula can swell, bleed or become inflamed if you have an infection or cold. If it stays swollen for more than two weeks, you may need surgery to remove it. This is called a tonsillectomy and adenoidectomy, or T&A.
The uvula isn’t essential to health and can be removed if it causes problems with speech, breathing or swallowing. Surgery usually takes about 45 minutes and has few risks, although it does increase your chance for developing an infection afterward.
What is the main function of the uvula?
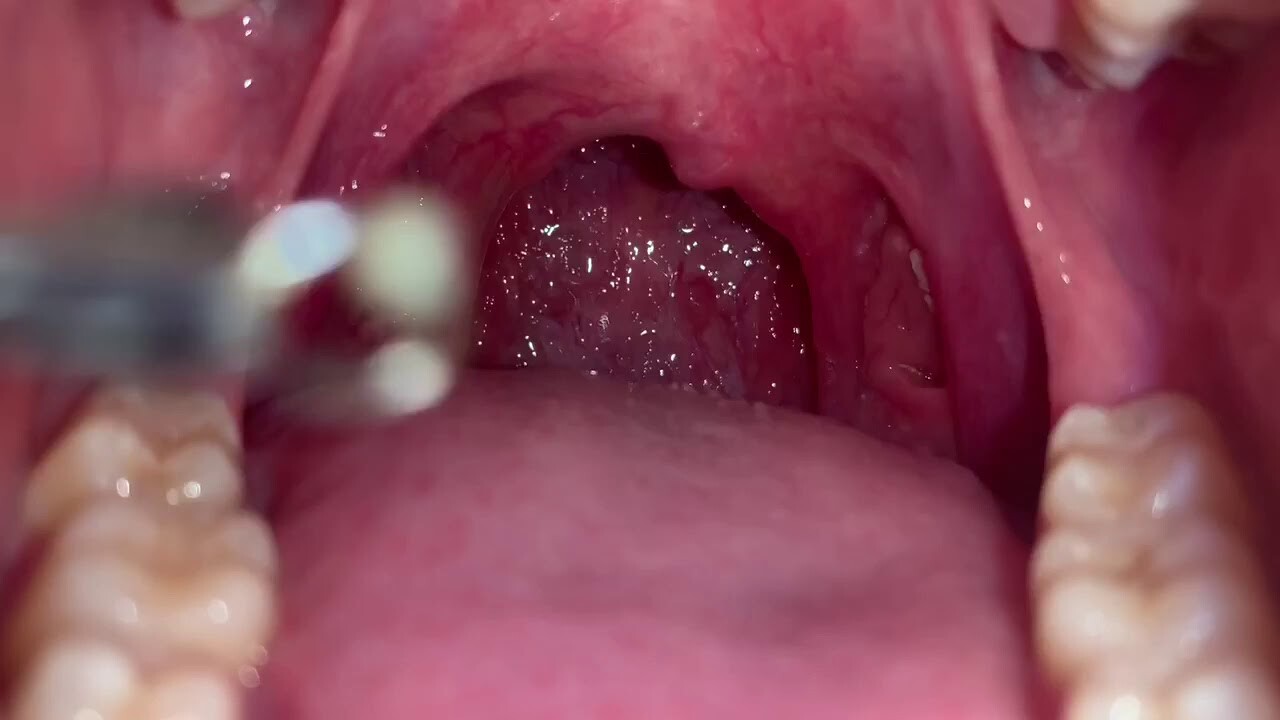
The uvula is a small, fleshy tab of tissue that hangs from the back of your soft palate. It’s usually visible from the front of your mouth.
The uvula’s main function is to help you swallow. As you’re swallowing, the uvula moves up and down, or swings from side to side, to help push food and liquids down into your throat. The uvula also helps make sure you don’t inhale any food while you’re eating. It acts as a safety valve by closing off your throat when it senses something coming in that shouldn’t be there.
The uvula, also known as the palatine uvula, is a small, fleshy, pendent organ in the back of the mouth. This structure is attached to the posterior portion of the soft palate by a membrane called the frenulum linguae.
The main function of this small structure is related to speech and swallowing. It helps with phonation (production of speech sounds), and it also helps prevent food from entering your airway when you swallow.
What does it look like?
The uvula looks like an inverted teardrop hanging from your soft palette at the back of your mouth. It varies in size and color depending on race and gender. It can be anywhere between three millimeters (0.12 inches) and four centimeters (1.6 inches) long with a width between half a millimeter and one centimeter thick (0.2-0.4 inches).
What if my uvula is touching my tongue?
If your uvula is touching your tongue, then it is likely that you have a condition called Uvulopalatopharyngoplasty, or UPPP. This condition is caused by the palatopharyngeal arch collapsing over time. It happens when there is an obstruction in the throat, which causes inflammation and swelling of the palatopharyngeal arch.
There are several different types of surgery that can be performed to correct this issue. The first type of surgery is called a uvulectomy, which involves removing part or all of the uvula. Another option for correcting this issue is laser ablation surgery, which uses heat to destroy tissue in order to shrink swollen tissues and open up airways.
The third option for correcting this issue is an endoscopic tonsillectomy, which involves removing part or all of the tonsils through a small incision just below your jawline so that they no longer obstruct breathing passages.
The uvula is a small, fleshy structure at the back of your mouth. Its role is to help with swallowing. The uvula is also known as the “drip” or “gravy” catcher because it catches excess saliva and other secretions while you sleep.
The uvula can be affected by a number of conditions, including allergies, inflammation and cancer. Sometimes, it’s simply a matter of having an overactive gag reflex — this is more common in children than adults.
If you’re concerned about your uvula touching your tongue, here are some things to consider:
If you’ve been diagnosed with a condition that affects your immune system — such as lupus or rheumatoid arthritis — it could be affecting your uvula. Some people who have these conditions have difficulty swallowing because of sores in the mouth that make eating difficult. In rare cases, this can lead to pneumonia when food gets stuck in the throat and mucus builds up there instead of being swallowed into the stomach where it’s meant to go.
If you have allergies or asthma, you may notice that your uvula becomes swollen during an attack (asthma causes swelling in certain parts of the body).
Can you choke on your uvula?
Yes, you can choke on your uvula. The uvula is the fleshy pendulous mass that hangs from the back of the soft palate. It is a common misconception that it’s the point of exit for taste buds, but in fact it has no taste buds at all. Your tongue contains up to 10,000 taste buds, whereas your uvula only has one or two.
The size of your uvula varies from person to person and can be swollen or enlarged as a result of an allergy or infection. When this happens, coughing and swallowing can become difficult as it blocks the throat and causes choking sensations.
In addition to an enlarged uvula being a choking hazard, it may also cause other problems such as snoring and sleep apnea due to its close proximity to the soft tissues in your throat.
Yes, it is possible to choke on your uvula.
The uvula is the small, dangling piece of flesh that hangs from the soft palate at the back of your mouth. It’s a quick-moving organ and will not tolerate being choked by food or other items in the throat. The uvula can easily be damaged by being choked, making it essential to remove anything blocking its movement.
If you’re choking on food and cannot breathe, follow these steps:
Yell for help. You need someone else to perform this next step. If no one is around to help you, shout as loudly as possible to attract attention. If someone else is nearby, they can call 911 for emergency assistance or use the Heimlich maneuver on you until your airway is clear.
If you’re able to speak but have difficulty breathing because something has lodged in your throat, cough hard several times until whatever is choking you pops out of your mouth and onto the floor (or wherever). This will release pressure on your windpipe so that you can breathe again.
What is the uvula quizlet?
The uvula is a small, fleshy, rod-shaped structure at the back of your mouth. It hangs down from the soft palate and is visible when you open your mouth wide. The uvula has no known function in humans. In some animals, however, it helps them breathe by filtering air.
In humans, the uvula serves no purpose other than to make sounds when we speak or sing. Some people have a longer uvula than others; this does not affect their ability to speak or sing.
The uvula is a tiny, fleshy piece of tissue that hangs down from the back of the soft palate and is visible at the back of your mouth. The uvula has many functions, including helping to keep the throat moist and aiding in speech by amplifying sounds. The uvula also helps prevent food and liquids from entering your windpipe when you swallow.
The Uvula Quizlet is a great way to learn more about what this part of your body does and how it is involved in different functions.
Is uvula the same as tonsils?
Tonsils vs Uvula
The uvula is a small piece of tissue attached to the back of your soft palate (the soft part at the back of your tongue). The uvula has no known function other than to make speech sound funny. The tonsils are also located at the back of your throat but are much larger and more complex structures than the uvula.
Tonsils protect against infection by trapping bacteria and viruses before they reach other parts of your body via mucus that drains into your throat from glands near them. They also help destroy bacteria when you swallow them. So why do people have them removed?
A tonsillectomy (removal of the tonsils) may be recommended if you have recurrent infection or inflammation that does not respond to antibiotics or other treatments. In rare cases, it may be necessary for cancer treatment as well.
Why does my uvula hurt when I swallow?
Uvula pain can be a symptom of many different conditions, such as sinusitis and postnasal drip. If you have a sore uvula, it’s important to see your doctor to determine the cause of your pain.
You may notice your uvula if you have an infection in your throat or upper respiratory tract. The uvula is the small piece of tissue that hangs down from the back of your tongue. It looks like a tiny ball attached to the back of your mouth near your throat. When you swallow, it moves up and down with each swallow.
In most cases, a sore or painful uvula is caused by something you ate or drank that irritated the back part of your throat — sometimes called regurgitation (gastric reflux). This can happen when there’s irritation from acid reflux or gastroesophageal reflux disease (GERD). GERD occurs when stomach acid travels back up into the esophagus (food tube), causing heartburn and other symptoms such as hoarseness, coughing, chest pain, shortness of breath and difficulty swallowing.
A throat infection can also cause pain around the uvula because bacteria irritate those tissues in the back of your throat when they migrate through
Uvula pain is a common problem that can be caused by a number of different things. The uvula is the small, flesh-colored tissue hanging down from your soft palate at the back of your mouth. The most common cause of uvula pain is swollen tonsils.
In rare cases, the uvula may be swollen due to a tumor or other problem with its blood supply. It’s also possible that your uvula could be infected or damaged by trauma (such as biting it).
Swollen Tonsils
Swollen tonsils are the most common cause of uvula pain. Swollen tonsils can occur when you have an infection in your throat or sinuses (sinusitis). This swelling can cause the uvula to get trapped between your tongue and the roof of your mouth, which makes eating and swallowing difficult.
Infection-related swelling usually goes away on its own after about 10 days (or less if treated with antibiotics). If it doesn’t go away after several months, you should see your doctor for more tests and treatment options.
What is it when your uvula is swollen?
What is it when your uvula is swollen?
The uvula is a small, thin piece of tissue at the back of the soft palate (the soft part at the back of your mouth). It hangs down and helps you swallow.
It may be swollen due to an infection or cold, but there are other causes too.
A swollen uvula can make swallowing difficult and noisy, as the uvula swells up into your throat. If you have trouble swallowing while you have a cold or infection in your throat, see a doctor.
(08/23/2024)by Dolpxy
More Information: N
Views: 452

Halitosis: the answer is in the mouth?
Halitosis is the signal that warns us that we have a problem of the mouth, not the stomach as has been thought until now. In addition, six out of ten cases, behind the problem of halitosis is hidden a periodontal pathology. Clear the origin of halitosis, experts’ stress that not always diagnosed correctly.
Halitosis is a problem underdiagnosed and therefore undertreated. A problem was related to the stomach. Until now. Because experts insist that this is a sign of mouth problems. Thus, according to point, in nine out of ten cases of halitosis (bad breath) is caused by a problem in the oral cavity and in six out of ten there is a periodontal disease diagnoses (periodontisis, gingivitis).

The halitosis is a problem that goes much further, as it is a sign that something is wrong in our bodies particularly in our mouths, so we must pay special attention. As experts suggest, halitosis requires diagnosis and treatment. Its origin is mainly due to the presence in the oral cavity of volatile sulfur compounds. Compounds that can be altered both its quantity and its quality by mouth bacteria, amino acids, protein substrates, the physical and chemical conditions and, particularly, saliva.
In addition, doctors also detected another problem, the pseudohalitosis, when there is no presence of bad odor from the mouth but the patient believes it does have this disease. When the confirmation that there is a problem of halitosis does not convince the patient would be facing what is called halitophobia, a variant that requires not only medical care but the help of a specialist in psychology.

Among the treatments for halitosis, and aims to reduce the presence of odor-causing bacteria from both the language and the grooves or periodontal pockets, experts highlight the interesting results being achieved with Halite, a pioneer in the treatment control and halitosis.
Prevention, as elsewhere in relation to health, also plays an important role. At this point, experts suggest that the best way to prevent this is with a suitable care of the oral cavity, especially the gums. Daily hygiene measures are essential, since a correct brushing to a lingual hygiene with a suitable scraper. Another measure to consider relates to food, it is advisable not to follow a high protein diet as it can worsen the symptoms of halitosis.
(08/24/2024)by From Doctor
More Information: https://fromdoctor.com/halitosis-the-answer-is-in-the-mouth.html
Views: 296

Do You Have a Sore throat after Wisdom Tooth Surgery?
It’s time for the dreaded wisdom teeth to come out. It’s a little scary, but the surgery will be quick and relatively painless. Let’s talk about the recovery. It’s not always easy, but it’s completely doable.
A number of patients report a sore throat after their wisdom tooth extraction surgery, but it won’t be the end of the world.
This pain is caused by swollen muscles that are in close proximity to the extraction site. It’s usually caused by a slight infection, but isn’t serious unless the pain persists for weeks or more. It should only linger for about 3 days after the surgery.
But until the pain subsides there are things you can do! Your sore throat after your wisdom tooth surgery is completely normal and you can have it subside in no time with some simple remedies.

Salt water remedy
Gargling salt water is a remedy for most any mouth pain. It contains natural healing properties that soothes pain and reduces inflammation. It also tends to speed up the healing process and remove bacteria.
Dentists and doctors recommend rinsing the mouth with ½ teaspoon of salt mixed into a cup of warm water. Because salt water is all natural, this method can be applied as many times as needed.
However, when spitting out the water, be careful not to apply too much force. This can create dry sockets in the mouth and lead to further issues. Be gentle as you rinse and spit.
A cold compress or cold treats
A sore throat after oral surgery is typically due to swelling. In order to decrease swelling, a cold compress or ice pack can be applied to the throat…20 minutes on and then 20 minutes off until the swelling goes down is recommended. Popsicles, ice cream, or other cold treats can also ease the pain internally and add a little sweetness to the recovery process.
Hot tea and lots of liquids
Teas such as chamomile or peppermint can greatly soothe a sore throat. Being careful not to make the tea harmfully hot, this can be a quick and simple remedy. Water and other gentle, non-citrus fluids are helpful to keep the throat hydrated and flush out bacteria.
Lemon and honey
Both lemon and honey also have natural soothing properties that can ease a sore throat. While these are both very helpful to healing the side effects of a mouth surgery, overuse could cause problems on the surgery site. As always, it is important to monitor and use moderation when using these ingredients.
Eat soft foods
Try to eat at typical meal times, but choose soft foods that will go down easily and won’t get stuck in your throat or hurt the healing wound. Foods like yogurt, soup, and ice cream can benefit and even help soothe a sore throat.
While it is normal to have a sore throat for a few days after a tooth extraction, it could be cause for concern if the pain and soreness persists more than a week or if it hinders your ability to speak.
While long term issues are very rare, and sore throats after surgery can end up being completely unrelated anyway, this pain is not something that should be ignored just in case.
At this point, you should contact your doctor or dentist. They’re always happy to help!
Your throat should be ready for talking and your mouth should be ready for eating again a few days after your tooth extraction. In the meantime, enjoy as much ice cream and popsicles as possible and rest that mouth! You will be back and ready to take your life back in no time!
(08/24/2024)by Oral Surgery Specialists Of Atlanta
More Information: https://www.oralsurgeryspecialistsatlanta.com/blog/do-you-have-a-sore-throat-after-wisdom-tooth-surgery/
Views: 339
All About Osteosarcoma of the Jaw
Before discussing what osteosarcoma of the jaw is, it may be helpful to explain what sarcoma is in general. Sarcoma is a type of cancer that affects the body's connective tissues—the bones, cartilage, muscles, tendons, ligaments, fat, skin, nerves and blood vessels. This malignancy most commonly occurs in soft tissues, but it can also develop within the bones; when this happens, it’s referred to as "osteosarcoma" or "osteogenic sarcoma."
Although osteosarcoma can affect any bone in the body, it most commonly develops in the upper arm bone (humerus), the thigh bone (femur) and the shin bone (tibia). However, approximately 6% to 7% of osteosarcoma cases occur in the jawbone.
Jaw osteosarcoma tends to behave differently than other sarcomas. For example, when compared to osteosarcoma in longer bones, jaw osteosarcoma generally:
Develops 10 to 20 years later in life

Is less likely to spread (metastasize) to distant areas of the body
Produces higher survival rates
As such, it's important to look at jaw osteosarcoma on its own. Below, we explore causes, risk factors, symptoms and treatment options.
Jaw osteosarcoma causes and risk factors

Researchers are still working to determine precisely what causes osteosarcoma of the jaw (as well as osteosarcoma in general). However, studies suggest that the following factors may all increase a person's risk of developing jaw osteosarcoma:
Exposure to ionizing radiation and/or chromic oxide (a radioactive scanning agent)
Paget's disease
Fibrous dysplasia
Certain genetic mutations
It's important to note that while rapid bone growth is commonly considered to be a risk factor for certain other types of osteosarcoma, it’s likely not a major risk factor for jaw osteosarcoma. This is because osteosarcoma of the jaw often develops 10 to 20 years after adolescence (when growth spurts often occur), suggesting that there’s not a strong connection between jaw osteosarcoma and sudden bone growth.
Jaw osteosarcoma symptoms
Individuals with osteosarcoma of the jaw most commonly complain of swelling (this is different than with long bone osteosarcoma, where the most common complaint is bone pain during activity). Other osteosarcoma of the jaw symptoms may include:
Pain
Tingling (paresthesia)
Ulcerations
Jaw osteosarcoma treatment
The course of treatment recommended for osteosarcoma of the jaw will vary from one patient to another. With that being said, physicians often recommend surgically removing the cancer from the jawbone. Because the jawbone is considerably more delicate and complex than longer bones in the body, jaw osteosarcoma surgery can be particularly challenging. Treatment for osteosarcoma of the jaw may also involve chemotherapy and/or radiation therapy.
Where to go for jaw osteosarcoma diagnosis and treatment
If you’re concerned that you might have osteosarcoma of the jaw, it’s important to promptly consult with a physician, since early detection and treatment can improve outcomes and quality of life. You can rely on Moffitt Cancer Center for prompt jaw osteosarcoma diagnosis and the most innovative types treatment. Our multispecialty team has extensive experience treating various types of osteosarcoma—including jaw osteosarcoma—and you can trust that we’ll provide you with a highly individualized treatment experience, start to finish.
(08/26/2024)by Moffitt Cancer Center
More Information: https://www.moffitt.org/cancers/sarcoma/faqs/about-osteosarcoma-of-the-jaw/
Views: 388
Reasons for Bitter Taste in Mouth and Ways to Treat It
Bitter taste or any altered taste sensation is called dysgeusia. Feeling a bitter taste in the mouth or experiencing any altered taste sensation may not be a disease by itself, but rather a symptom of an underlying condition.
Most of the time, a bitter taste remains in the mouth after eating a pungent or sour food. That taste sensation goes away by itself after some time. However, if an underlying illness is present, then a bitter taste can be experienced spontaneously, even without eating any food.
In an article published in the American Journal of Medicine, the National Health and Nutrition Examination Survey (NHANES) 2011–2012 reported that more than 5% of the over 142 million US respondents experienced taste disorders, and increasing age was associated with the increasing prevalence of taste disorders.
Common Causes for a Bitter Taste in the Mouth

1. Gastroesophageal reflux disease (GERD)
GERD occurs due to the reflux of acidic juices produced by the stomach up into the esophagus, which is the muscular tube connecting the throat and the stomach. This regurgitation of the acidic stomach contents can render a bitter or sour taste in your mouth.
GERD often leads to an altered sense of taste and smell that is also common in gastroparesis, a chronic stomach motility disorder that prevents stomach emptying.
2. Medications

Many medications, including antibiotics, blood pressure, and heart medications, thyroid medications, psychiatric medications, anti-cancer drugs, cause an altered taste in the mouth.
3. Oral and dental causes
A bitter taste in the mouth can be the result of poor oral hygiene, gum disease, mouth ulcers, cavities, ill-fitting dentures, or fungal infections such as oral thrush.
Also, the use of various types of cement or local anesthesia during dental procedures can temporarily alter the sense of taste, but it usually resolves within a few hours after treatment.
4. Radiation therapy
This treatment modality can damage the taste buds, associated nerves, and/or salivary glands and can alter taste sensation.
5. Chronic diseases
Diabetes, kidney disease, thyroid disease, and upper respiratory infections such as the common cold, sinusitis, and flu may sometimes affect the taste sensation.
6. Nutrient deficiencies
Zinc, vitamin A, and vitamin B12 deficiencies can cause taste disturbances.
7. Sweets
Some sweet substances may taste bitter if consumed immediately after brushing the teeth, due to the ingredients (such as sodium lauryl sulfate) in some toothpaste.
8. Menopause
Abnormal taste sensations (salt, peppery, or sour) are seen during menopause in some women, along with burning mouth syndrome.
9. Xerostomia (dry mouth)
This condition causes an alteration in taste sensation. Dry mouth occurs when saliva production by the salivary glands is decreased, which may be due to medications, chemotherapy or radiotherapy, increased tobacco use, aging, etc.
Accompanying Symptoms
Bitter taste in the mouth is usually accompanied by the following symptoms:
Loss of sense of smell
Burning mouth syndrome – Burning, stinging, and/or itching of the mouth, especially the tongue, sometimes extending to the lips and other areas of the mouth
Nasal congestion (stuffy nose)
Other altered taste sensations, such as a metallic taste in the mouth
Dry mouth
Medical Treatment
The treatment for an altered sense of taste depends on the underlying cause:
If the bitter taste or any altered taste sensation is caused by medications, then reviewing the patient’s medical history and evaluating a change in medication is recommended.
If it is caused by a chronic condition or underlying illness, then evaluation and treatment of the condition are recommended.
Zinc supplementation is given to patients with a zinc deficiency, and according to some studies, it is even given in patients with unknown reasons for the taste alteration. Taste sensation alterations due to radiation therapy or chemotherapy will gradually reduce in a few months after the cessation of treatment. Zinc supplementation might also be helpful in these patients.
A bitter taste in the mouth after tooth brushing or getting any dental treatment is transient and goes away on its own in a few hours.
Identifying the exact cause for the bitter taste in your mouth is a multi-step procedure, which involves:
Taking your medical history
Reviewing your medications
Examining your head, neck, and oral cavity
Subsequently, the doctor may order a few additional tests:
Different kinds of taste tests are performed. The patient is asked to taste sweet, salty, sour, and bitter taste solutions and to identify their quality and intensity to assess the taste sensation.
Swab tests are sometimes done if a bacterial or fungal infection is suspected.
In some cases, trauma or head injury may affect the nerves supplying the taste buds and may cause an altered or loss of taste sensation. In these cases, a CT scan or MRI may be required.
Blood tests and/or urine tests are performed to diagnose any underlying medical conditions.
Here are some common tried-and-tested tips and measures to reduce the bitter taste in your mouth:
Maintaining good oral hygiene, which includes brushing twice a day, flossing, tongue cleaning, and using a mouth rinse, helps reduce the bitter taste if it is due to gum disease or other oral infections.
Chewing sugar-free gum and drinking more water helps reduce dry mouth and the altered taste sensation.
Reducing the consumption of foods that taste metallic or bitter, such as red meat, coffee, and tea, will reduce the altered taste sensation.
Eating a nutrient-rich diet that includes eggs, dairy, fish, fruits and vegetables will help.
Adding seasoning and spices to food enhances its flavor.
Developing a bitter taste in your mouth is usually not a serious problem and can be resolved by evaluating the underlying problem and treating it. Good oral hygiene, a nutritious diet, and drinking lots of water are some of the most commonly recommended solutions.
A doctor should be seen if other symptoms are experienced or if there is any loss of appetite. In light of the new coronavirus pandemic, it is advised to see a doctor if any recent loss of taste or smell is noticed.
(08/25/2024)by Emedihealth
More Information: https://www.emedihealth.com/oral-health/mouth-jaw/bitter-taste-in-mouth
Views: 307

How to Solve The Five Most Common Dental Problems?
Oral hygiene is one of those areas that most people find easy to neglect. However, a little effort up front goes a long way toward preventing cavities, gum disease, and other issues that are, unfortunately, quite common. As you review the list below, don't hesitate to get proactive and start implementing preventive solutions as soon as possible.
1. Sensitive Teeth
Sensitive teeth can be painful, and they can also end up having a significant impact on which foods you are able to eat. If you've noticed that your teeth have become sensitive to sugary foods, then it's time to put away the candy and get more disciplined with your diet. Drinking icy water, hot coffee, or hot tea can also trigger sensitive teeth.
While sensitive teeth can be a symptom of many underlying conditions, gum issues are among the most common causes. Brushing your teeth too aggressively can cause gums to recede, but so can normal aging. If you've already eliminated bothersome foods and checked your brushing habits, then the next step may be to come in for a checkup.

2. Gum Disease
Buildup of tartar and plaque on the gums can cause gingivitis, and gingivitis can lead to painful inflammation. When gingivitis progresses without treatment, it can turn into a serious condition known as periodontitis. Fortunately, it's easy to catch gingivitis early.
Common symptoms include discoloration around the gum line or swollen and sensitive gums. In addition to brushing your teeth once in the morning and once in the evening, flossing regularly also provides a solid defense against gingivitis.
3. Decaying Teeth

When many people think of dental problems, cavities are what immediately come to mind. However, it's more accurate to think of tooth decay as a process. If decay is able to set in and start damaging a tooth's enamel, then eventually it will eventually begin damaging that tooth's root unless treated. Like gum disease, tooth decay isn't difficult to prevent. Brushing, flossing, and scheduling regular dental appointments can certainly help you avoid pesky cavities and stay away from costly dental surgery.
4. An Infected Root
Most often, an infected root is the result of untreated tooth decay. As suggested by its painful nature, a root infection is an emergency situation. As the infection progresses, you may notice swelling in your checks, sore gums, pain in your jaw, and even swelling of the lymph nodes. The best way to prevent a root infection is to follow our advice for preventing cavities and gum disease.
5. Missing Teeth
This is the only common problem on this list that isn't necessarily due to poor dental hygiene. Through no fault of your own, an unfortunate accident can result in missing teeth. Regardless of the cause, however, it's important to replace a missing tooth as soon as possible. Fortunately, we offer dental implant services that can help.
(08/27/2024)by Brookmere Dental Group
More Information: https://www.brookmeredental.com/how-to-solve-your-5-most-common-dental-problems/
Views: 331
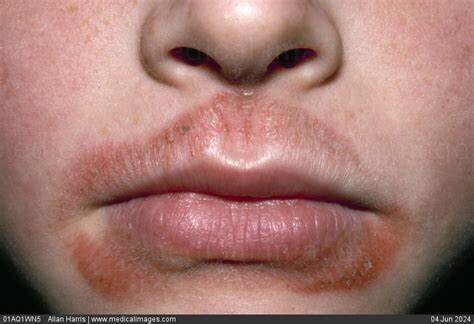
Dry Skin Around the Mouth and Chin: Causes, Treatments and Prevention
Dry skin around the mouth and chin is a common skin issue that can cause redness and mild to extreme discomfort. While it is typically caused by lifestyle choices and environmental factors, dryness can also be caused by a poor skin care regimen.
Enhancing your skin care regimen is key to treating and preventing dry skin around the mouth. Skin hydration can be improved through regular application of creams and ointments, while SPF creams work to protect your skin from environmental damage.The exact treatment for your skin will depend on what is causing your dry skin to occur.
What Causes Dry Skin Around the Mouth
Dry skin around the mouth can be caused by a number of external factors, including the use of harsh skin care products or as a result of your environment.
The skin’s outermost layer, known as the epidermis, acts as a barrier that protects the body and underlying layers of skin from damaging chemicals, pollutants and irritants. It also helps to maintain skin’s hydration and softness.

Sebum is a yellow, oily substance produced by the skin’s sebaceous glands to bolster hydration. It is vital in keeping skin moisturized and protected; low sebum production can lead to dry skin around the mouth and chin.
Fatty acids and cholesterol are also among the most important lipids for skin hydration. They improve the skin’s elasticity and help to heal a damaged skin barrier.
While external damage to the skin’s barrier is often the cause of dehydrated skin, certain medical conditions can also be responsible, such as perioral dermatitis and angular cheilitis (AC) which can both lead to drier skin.
Dehydration
At its core, dry skin is caused by a lack of moisture in the outermost layer of skin. This can simply be the result of general dehydration due to a lack of water consumption. Most adults should drink about 2 liters of water a day, however many consume far less than this recommended amount.
The lips and mouth are among the first areas where the visible symptoms of chronic dehydration occur. Before altering your skin care regimen, first increase your water consumption levels and track your skin’s progress over several days to see if the issue resolves.
Naturally dry skin
One of the most common causes of dry skin is a naturally low level of sebum production. Some experience lower than average levels of sebum production throughout their life due to genetics. Dry skin types require ongoing dry skin management as part of their regular skin care routine.
Changes in hormone levels can sometimes briefly alter sebum production levels; for these cases, dry skin may only require temporary measures.
Lifestyle
Dry skin around the mouth and chin can be the result of poor habits and lifestyle choices including:
Ineffective cleansing that leaves behind irritating makeup and other impurities
Use of harsh skin care products
Excessive sun exposure
Using hot water that strips the skin of its natural oils
Excessive lip-licking that can dry out and irritate the mouth and skin
Skin care products
Some skin care products can compromise the outer layer of skin, hindering the epidermal barrier function and causing a significant loss of water that can lead to dehydrated scaly and flaky skin.
For example, astringents and exfoliants are well-known for their drying effects and can have a detrimental effect on dry, flaky skin. Reduce the use of these products or avoid altogether to preserve moisture in the area around the mouth and chin.
Skin care product preservatives
Cleansers, toners, lip balms, toothpastes and moisturizers often contain preservatives that can cause redness, sensitivity and extremely dry skin around the mouth. Some products can also trigger eczema and contact dermatitis.The following ingredients may irritate the skin and should be avoided:
Alcohol (denatured)
Formaldehyde
Parabens (including “natural” parabens)
Phenoxyethanol
Phthalates
Sodium lauryl sulfate (SLS)
Sodium laureth sulphate (SLES)
Allergies and irritants
Colorants and pigments can be found in a number of cosmetics and in most cases, they can be easily identified on a product’s label.
There are two types of colorants: artificial and natural. Artificially-derived colorants, such as barium sulfate–which is used as a whitening agent–and aluminum powder, are particularly common and can provoke an allergic reaction.
Artificial colorants can also increase the risk of irritation and may cause inflammation, dryness, or cracked skin around the lips.
Medical conditions
Perioral dermatitis is an inflammatory skin condition found in both adults and children. This condition is characterized by a red, scaly or bumpy rash. Inflammation, redness around the mouth and mild itching or burning can also occur.
Topical corticosteroid cream has been known to aggravate the condition and overuse of heavy face creams and moisturizers may also cause irritation, particularly on sensitive skin.
Angular cheilitis is a bacterial infection of the lips that causes inflammation in one or both corners of the mouth. It can lead to redness, swelling and cracked skin.
Contact dermatitis is caused by coming into contact with substances that provoke an allergic reaction. Lip balms, lipsticks, soaps, toothpaste and hair removal products can typically lead to a red, itchy rash near the lips.
Dry Skin in the T-Zone
The T-zone–the central area of the face that includes the forehead, mouth and chin–is often plagued by overly oily skin, or in some cases, particularly dry skin. This is especially true in the winter months due to harsh weather conditions and the drying effects of central heating that can damage the outer layer of skin.
Taking basic precautions such as wearing a hat and scarf can help protect most of the T-zone from winter damage. Moisturizer and lip balm use should also be increased in winter months to compensate for the drying effects of indoor heating.
While it may be tempting to forego sunscreen in the winter, the snow’s reflective surface can increase sun damage to the T-zone area; protect this area with an SPF sunscreen and lip balm.
As the T-zone area is both particularly delicate and oil-prone, it is often the focus of skin care routines. As a result, the area can easily become overburdened by harsh skin care products causing dryness.
When applying products to the area, it is important to read instructions and to use the products as directed. Watch for early signs of irritation, and discontinue use before serious dryness occurs.
How to Treat Dry Skin Around the Mouth
Dry skin around the mouth can often be treated effectively with the right hydrating products. When managing dry skin, avoid using products with a high oil content and strong scents as these may further irritate the skin.
Moisturizers have multiple functions and while many formulas help to improve the appearance of skin and help it retain moisture, some can deteriorate the skin’s condition and weaken the outer layer. This is why it’s important to know which ingredients are in your skin care products.
Cleansing routine
Cleansers are designed to clean the skin, remove makeup and general buildup accumulated throughout the day. However, many cleansers include surfactants: soaps that strip the skin and cause damage to essential skin proteins and lipids. As a result, skin can feel tight, dry and irritated.
A mild and gentle cleanser is advised for dehydrated skin. Using a cleansers containing hydrating agents such as lipids, occlusives, and humectants will help retain the skin’s natural oils and reduce skin damage.
Cleansing oils and balms are particularly beneficial for dry skin. Key ingredients to look out for include hyaluronic acid (HA) and ceramides. HA locks in moisture, helping skin appear plump, while ceramides are fats that help prevent further moisture loss.
Gentle exfoliation
Gentle exfoliation can improve the skin’s texture and help buff away the natural buildup of dead cells. Exfoliate the area around the mouth and chin with a gentle formula using a slow circular motion.
How often you exfoliate your face will depend on how sensitive your skin is. Start by exfoliating once per week and increase to a maximum of once every three days. If irritation occurs, decrease the frequency of exfoliation.
You can also exfoliate your lips, if they are especially dry. When doing so, seek out the most gentle physical exfoliant available.It is important to keep lip exfoliation to a minimum, at most once per week.
Facial hydrating serum
Follow your cleanser with a facial hydrating serum that is silicone- and petroleum-free, and has a low oil content. Ingredients that promote hydration include glycerin and HA.
Particular care should be taken with HA. While it can be an effective barrier to moisture loss when used properly, overuse can draw moisture out of the body leading to dry skin. Always use it sparingly and follow with a hydrating moisturizer and broad-spectrum SPF to protect your skin from damaging UV rays.
Broad-spectrum SPF
The sun is known to have a drying effect on the skin, especially if the skin isn’t protected properly. It can deplete the skin’s supply of natural lubricating oils and worsen dry facial skin.
Apply a broad-spectrum sunscreen daily following your face moisturizer. This will protect you against harmful UVA and UV rays which are known to accelerate the aging process and damage the skin barrier.
Some lip balms also contain SPF, which will help protect and condition dry skin on the lips and around the mouth. Always use an SPF of 30 or higher for maximum protection and coverage.
Effective Preventative Methods
For individuals already consuming adequate amounts of water, the use of topical emollients will improve the skin’s barrier function and improve the look and feel of dry skin. Using skin care products with added emollients (moisturizers) will help lock in the skin’s natural oils for healthier looking skin.
In addition to this, skin care products and cosmetics containing preservatives, fragrances and artificial colorants should be avoided, as they may trigger allergies.
Generally, it’s best to avoid overexposure to the sun, excessive washing and products with irritants or harsh chemicals, as this can further aggravate the affected area.
When to See a Doctor
It can sometimes be difficult to identify the root cause of dry skin. If you are unable to isolate the cause of your dry skin, seek out professional help. Similarly, if you believe that an underlying medical condition is causing your dry skin, a professional will be able to confirm your suspicion.
If you are concerned that your condition may be linked to medically-prescribed topical creams or other prescription skin care product it is best to seek professional advice before discontinuing use.
Takeaway
When dry skin occurs around the mouth, try to identify the problem before treating the condition. It may be easier to prevent further damage than to treat an ongoing issue.
The first step in treating dry skin is to change harmful lifestyle habits and see if those changes result in a noticeable improvement. Eliminate certain products from your skin care regimen, particularly those containing preservatives, fragrances and synthetic colorants. Change any cleansers or moisturizers containing surfactants to formulas that are more hydrating.
If dryness continues, add a facial serum with ingredients such as HA to your skin care regimen to help retain your skin’s natural moisture. You can also use a gentle exfoliator to buff away the natural buildup of dead skin cells. To protect your skin against harmful UV rays and environmental factors, apply a lightweight broad-spectrum SPF following your moisturizer.
Finally, ensure you are drinking plenty of water and liquids to stay hydrated throughout the day.
If the problem persists, consult a doctor or dermatologist who may be able to identify the root cause.
(08/26/2024)by Dermo Collective
More Information: https://dermcollective.com/dry-skin-around-the-mouth-and-chin/
Views: 317

Common Diseases That Cause Tooth Decay
No part of the body functions truly independently, and your teeth are no exception. Tooth decay can be caused by much more than just poor oral hygiene. Tooth decay is often a symptom or warning sign of something much larger, and possibly more dangerous, happening in the body. In fact, there are common diseases that cause tooth decay.
When you visit your local dentist for an exam, like our Mount Prospect dentist, we are looking at more than just the physical appearance of your teeth. If you’ve ever wondered why we ask so many questions about your lifestyle and the rest of your medical history, it’s because we are trying to understand the entire picture, along with what your mouth and oral health is telling us.
Common Diseases That Cause Tooth Decay
The mouth is a window to the rest of the body and will often show warning signs that there’s something bigger going on. Here are some of the diseases that frequently cause tooth decay. If you suffer from any of these conditions, be sure to discuss with your dentist at your next appointment.

Diabetes
Diabetes has perhaps the most significant cause and effect relationship with tooth decay. Whether you have type I or type II diabetes, your body’s blood sugar is elevated because of lowered insulin levels. This impacts many parts of the body, and the mouth is a big part of that.
One of the most common symptoms of diabetes is a dry mouth, which is due to a lack of saliva. Beyond making your mouth feel more comfortable, saliva also helps protect your teeth against the bacteria that cause tooth decay. If you don’t have enough saliva, your teeth are more vulnerable, and your risk of developing cavities is higher.
As the tooth decay continues to build up, the risk for gum disease also increases. Gum disease is caused as bacteria continues to build up in your mouth. In fact, about a quarter of all people diagnosed with diabetes also develop gum disease.

To further complicate the situation, gum disease causes blood sugar levels to rise, which can, in turn, increase the severity of the diabetes. It’s a vicious cycle that needs to be addressed as soon as symptoms begin to develop.
Autoimmune Conditions
Autoimmune conditions are a family of diseases that involve the body attacking parts of itself. This can include everything from major organ systems, like the kidneys, to smaller systems like salivary glands. Many of these diseases have some impact on the mouth, but the one most directly tied to oral health is Sjögren’s syndrome.
Sjögren’s reduces the amount of saliva the mouth produces, which has the same effects we described earlier with diabetes. In extreme cases, patients may not even produce saliva at all.
People with Sjögren’s may need to visit the dentist more frequently than twice per year to keep tabs on tooth decay that results from decreased saliva production. There are also over the counter lozenges, mouthwashes, and other products that can help increase saliva production and manage symptoms day-to-day.
Anorexia and Bulimia
Both anorexia and bulimia are severe eating disorders. They occur when men or women have an extreme fear of becoming overweight and either eat less or regurgitate food as a result.
Both conditions have implications on the teeth because the body is not getting the minerals, vitamins, proteins and other nutrients that it needs to maintain good oral health and prevent tooth decay from forming. When people with anorexia do eat, they tend to fill up on sugary, salty, unhealthy foods that are bad for your teeth.
In addition, a person who is bulimic may binge eat and then vomit. When this occurs the acids that break down your food eat away at the tooth enamel, which leads to decay over time. Other effects of bulimia include bad breath, swollen glands, and teeth that appear to be worn down.
Avoid Tooth Decay with Total Body Care
These are just a few of the more common diseases that cause tooth decay. The connections between your mouth and the rest of your body are not always apparent which is why it’s important to share your medical history with your dentist.
(08/27/2024)by 1st Family Dental
More Information: N
Views: 273

Why Do I Experience Gum Pain In Back Of Mouth?
Our gums are made of soft tissues. That is the reason why it could easily get sore. Gum pain in back of mouth is often related to other symptoms such as bleeding, swelling, and pain while eating.
Other symptoms are hard to determine; it might require you to visit MyLocalDentists’ Burwood clinic to determine what causes your gums to be painful. Furthermore, you might notice that your teeth and gums are more painful while brushing or flossing. Oral products with alcohol might also cause stinging pain in the mouth.
General Causes of Gum Pain
In most cases, pain in the gums and teeth is due to poor oral health. Neglecting your oral care can cause many damages such as gum disease, canker sores, bad breath, infections, gingivitis, and many more. Let us find out the most common reasons why your gums at the back are painful and swollen, starting with:
Gingivitis
Gingivitis is a common kind of gum disease that causes irritation, inflammation, and gum redness. It is also one of the leading causes of bleeding gums that lead to soreness. Apart from painful gums, it might also come with other complications such as:
tender and receding gums
bad breath

puffy gum line
Poor oral hygiene is the number one reason why gingivitis occurs. Not brushing the teeth daily gives the bacteria easy access to penetrate the gum and cause infection.
Oral Thrush
Another thing that usually affects the mouth is the fungal infection, also known as oral thrush. It is commonly diagnosed in babies, older adults, and those who spend plenty of time in hospitals. The fungus that causes this is also the same that causes vaginal yeast infection.
Trush comes with white spots on the inner cheeks and tongue. Eventually, the spots will reach the gums in the back of the mouth and the tonsils. Once the spots reach the gums, they will start to feel sore and irritated. While this is not as serious as periodontal disease, it is still essential to seek treatments.
Periodontitis
Periodontitis is a serious gum infection that needs to be treated immediately. This gum disease usually starts from neglected gingivitis and grows gradually. It is the result of plaque buildup that damages the bones and tissue around the teeth. Eventually, the teeth will become loose, and the risk of losing a tooth or two might follow. Severe cases include the following signs:
swollen gums
inflammation
tooth abscess
teeth gaps
painful gums
pain when eating food
changes in bite
The treatment for periodontitis needs the professional help of a dentist. While improving your oral hygiene might help, root planing and scaling as early as possible are still the best options to prevent tooth loss. These treatments will eliminate the bacteria residing inside the tooth and under the gums.
Gum Pain in Women
Surprisingly, gender has a major in gum pain as well. While pain in the gums could happen to anyone, women experience them for specific reasons. A woman might seem healthy on the outside, but several factors could affect their dental health, such as:
Hormonal changes
Taking birth control pills and puberty are the main causes of changes in the hormones in women. These changes in a woman’s body can impact how the body provides blood to other parts, including gums. Lack of blood supply can cause your gum to be more sensitive, leading to dental stress.
In addition to swollen gums in the back of the mouth, changes in hormones could also lead to:
puffy and red gum
bleeding gums
tender gum
If you suspect that this is your case, give your family dentist a call for pain relief. Professional teeth cleaning in addition to brushing and flossing is also essential. You can visit EmergencyDentistAdelaideDR.com.au if you need urgent dental care.
Pregnancy
When a woman gets pregnant, her hormones are on high performance. This shows significant changes in their dental and overall health. The most compromised parts of her body during pregnancy are her teeth and gums. Pregnant women are also at higher risk of gum disease. Bleeding gums and painful guns might occur with soreness as well. In line with this, most oral health issues will end after giving birth.
Menopausal stage
Reaching the menopausal stage causes a lot of changes in a woman’s body. After menopause, she might experience the following:
hot and cold sensitivity
dry mouth
mouth burns
taste changes
Saliva production is important to keep the mouth clean; reduced production will cause bacteria to grow and eventually lead to gum disease and oral health problems, including gum pain. Fortunately, you can fight dryness by staying hydrated and using oral products such as dental spray. You may also chew on ice to keep your mouth moisturized.
Unusual but common causes of gum pain
Canker sores
Canker sores are the tiny sores that grow under the tongue, inner cheeks, and gum base. They feel soft and tender and typically appear in clusters. Furthermore, they might cause pain and swelling. The good news is that the soreness will go away on its own in few days.
Dental Appliances
It is most imperative to practice proper oral hygiene if you are wearing braces or prostheses. Your gum base might feel swollen right after their application due to the friction that scratches the gum tissue. Brush your teeth gently and floss diligently to improve your oral health.
Overall, the best way to prevent gum disease and gum pain is by practicing good oral hygiene. Professional teeth cleaning accompanied by the following will greatly help:
Avoid excessive use of tobacco products
Floss daily
Choose a toothpaste with fluoride
Seek treatment early on
Prioritize healthy diet
(08/28/2024)by Cheney Clinic
More Information: https://www.cheneyclinic.com/gum-pain-in-back-of-mouth/
Views: 328

