Dentists Journal
Top Ten Stories of the Week
9/7/2024
All Dentists Journal · Previous Week · This Week · All Time List · Headlines
What Are Oral Warts?
Oral warts and other types of mouth sores are normal for people who have HIV and AIDS. This article will talk about the kind of mouth issues that people with HIV can normally develop, and how to get rid of them. After reading the article, you can click on this link to know more about the topic of oral care for people with AIDS and HIV.
Oral issues for people with HIV
People who have HIV usually develop different types of mouth issues because of their weakened immune system. The mouth complications that develop in these patients are often more difficult to treat and they may also interfere with the HIV medication.
Are mouth issues contagious?

There are many types of mouth complications that can develop in a patient with HIV. Some of these complications may be contagious, and others may not be. Most of them can be treated with antiviral medications and frequent visits to the doctor.
As for oral warts for people with HPV or Human papillomavirus, they can be positively contagious if there is fluid within the wart and the surface of the wart is broken. There is a chance that another person can get the virus because of the fluid of the wart. Depending on where they are located in the mouth, these warts may be picked at and can bleed. They can also be very bothersome for the person who has them and can also affect the person’s self-esteem.
Prevention
One good way to prevent any type of oral issue is to have regular visits to a dentist. A person who suffers from HIV or AIDS has to have more frequent visits to the dentist in comparison to people who do not have the disease.

Dental visits will keep the person’s oral health in check and it will allow the dentists to administer treatment to any potential oral health issues that may be developing. They will be able to prescribe treatments and medications that will work in conjunction with the person’s HIV medication to keep any oral health issues at bay. Just the mere taking of the HAART medication or Highly active antiretroviral therapy for HIV can be a big help in keeping mouth sores and oral warts from occurring.
Getting treatment for mouth sores and oral warts
If you have oral warts or any other type of mouth sores, approach your doctor. They will help you get the right treatment for these oral issues and they can also advise you on different types of prevention techniques to avoid this situation again in the future.
On top of medical treatment and advice, your doctor or dentist can also recommend a support group you can join. Talking to and dealing with people who are going through the same conditions you are will help you better deal with your medical condition. It will also give you a chance to exchange input with other people and make the best out of your situation as well as give you a more positive outlook.
(08/30/2024)by Ending AIDS
More Information: https://endingaids.org/oral-warts/
Views: 372

Why Does My Jaw Hurt on Only One Side?
While sleeping, you’re jolted awake by a sudden pain on only one side of your jaw. Although the situation can be alarming and confusing, don’t worry – it typically isn’t a cause of immediate concern. However, that doesn’t stop the questions from running through your head. What does it mean? When should you see a dentist? How can you alleviate the discomfort? Luckily, we’ve got all the answers you’re searching for and more – just keep reading!
What Causes Jaw Pain?
There are several reasons why you may experience jaw pain on one side, including:
TMJ Disorders

A temporomandibular joint (TMJ) disorder affects the joint that connects your skull and jaw. A disc separates the bones in this joint and helps it move properly. If it becomes misaligned or the joint is damaged, you might experience pain and other symptoms like tenderness, earaches, clicking or popping when opening your mouth, difficulty opening and closing your mouth.
Oral Health Problems
In some cases, jaw pain on one side can indicate underlying oral health problems. Some common issues that cause jaw pain are cavities, an abscessed tooth, gum disease, tooth decay, growth of wisdom teeth, missing or crooked teeth, and clenching or grinding your teeth.
Sinusitis

Inflammation in your nasal cavities can cause sinusitis. Since the nasal cavities are located behind the cheeks, inflammation can cause pain in one or both sides of your jaw. Usually, this pain is accompanied by other symptoms like nasal congestion, yellow or green mucus, facial swelling, fatigue, and difficulty smelling or tasting.
When to See a Dentist
As mentioned earlier, jaw pain on one side isn’t usually considered a dire situation. But if the discomfort is accompanied by other symptoms, it could indicate a more severe condition – one that will require immediate treatment.
If you experience any of the following, contact your emergency dentist right away:
A persistent or recurring pain that doesn’t go away within a few days
Difficulty eating, drinking, swallowing, or breathing
Swelling or a fever that doesn’t go away
Significant pain that vanishes after a burst of salty liquid that tastes and smells unpleasant
How to Alleviate Jaw Pain
Do you have mild pain in your jaw? You may not need medical treatment! Here are a few ways you can get relief:
Apply a hot or cold compress. Heat can help your muscles relax, giving you relief from aches and stiffness. Alternatively, a cold compress can numb the pain and reduce swelling.
Take over-the-counter pain relief. Medications like acetaminophen (Tylenol) and ibuprofen (Advil) can temporarily relieve your pain.
Rest your jaw as much as possible. Stick to a diet of soft foods that don’t require a lot of chewing. It’ll help you avoid overworking your jaw muscles!
Massage your jaw. It can help release pain and tension in your jaw. Try some techniques on your own or visit a specialist for help (i.e., healthcare provider, physical therapist, massage therapist).
If you’re experiencing jaw pain on one side, use the tips outlined above for some relief. Although it should typically resolve on its own within a few days, you can always seek treatment from your dentist for peace of mind!
(08/30/2024)by Zumbro Family Dental
More Information: https://www.zumbrofamilydental.com/blog/why-does-my-jaw-hurt-on-only-one-side/
Views: 292
A Surprising Autoimmune Trigger Hiding In Your Mouth
Does this sound like you?
You’ve been ill with an autoimmune disease for a while, but you can’t recall a battle with Epstein-Barr virus, and none of the usual triggers ring true with you, or you have worked through the ones you had and aren’t seeing the results you expect. Another seemingly unrelated health issue is that despite brushing and flossing twice a day, following with mouthwash, your dentist is not happy with your oral health. You visit her regularly only to get more bad news about the spread of gum disease or the need for a root canal. An added worry on top of your autoimmunity issues!
What if your poor oral health was the trigger for your autoimmune disease?
We can’t blame your dentist or doctor for not spotting the connection. The trouble may lie in western medicine’s continued focus on treating the mouth separately to the rest of the body – but we’re beginning to catch up. There is increased focus on the importance of oral-systemic health.
The mouth is an important gateway to the rest of your body, and often the first line of defence in regards to inflammation and the autoimmune response. It is a heavily vascular area, meaning that any toxins or bacteria getting past its defences can travel around the body quickly, causing damage and instigating an autoimmune response.
There are over 100 diseases of the body originating in the mouth.

Is your autoimmune disorder one of them?
What Is the Oral Microbiome?
The oral microbiome cannot be seen, but it’s one of the most fascinating parts of the inside of your mouth. Your mouth is warm, moist, full of food particles – the perfect place for microorganisms to thrive – and that’s a good thing! Your oral microbiome behaves similarly to your gut microbiome – the ‘good’ bacteria keeps the ‘bad’ bacteria in check. The bacteria feed on food debris from your chewing.
Your oral microbiome is made up of similar bacteria to that in your gut, which adheres to your teeth as a biofilm. Biofilms are made up of communities of bacteria interlinked and able to communicate and collaborate with each other to build up resistance to your immune system.
When your mouth is healthy, the good microorganisms work together to contribute to your body’s workings in the following ways:
Digesting food debris

Generating energy
Colonisation resistance
Maturing epithelium cells and maintaining mucosal barriers (basically, maintaining a healthy environment by doing structural maintenance)
When your oral microbiome misbehaves, it initially causes mild diseases of the mouth, which can be treated by a dentist. However, an oral disease can trigger an autoimmune disease in susceptible individuals and can perpetuate it in others.
When Your Oral Microbiome Goes Wrong
When you’re healthy, the makeup of your oral microbiome remains stable. However, eating large quantities of refined sugar, having poor saliva levels, or maintaining poor oral hygiene can affect your oral microbiome for the worse. Dental implants, bridgework and prosthetics can all disrupt your oral microbiome, as the microorganisms are unable to stick to the man-made surfaces.
An unhealthy oral microbiome can cause:
Dental caries or cavities – small holes in the enamel of your teeth, caused by acid secreting bacteria.
Subgingival plaque, leading to –
Gingivitis – more commonly known as gum disease, is the condition where your gums become sore, inflamed, or swollen. Caused by a buildup of plaque – excreted by the bad bacteria in your mouth that feeds on food debris and sugar – gingivitis is best treated before it can progress into the more serious periodontal disease.
Periodontitis – otherwise known as periodontal disease. When you develop this disease, your gum tissue begins to pull away from your teeth and form little crevices: perfect for nasty bacteria to bed down in and multiply, causing infection.
Pulp infection in the centre of your tooth, leading to a root canal or tooth removal.
However, the results of an unhealthy oral microbiome don’t start and end in the mouth. Due to the link between oral and systemic health, an unhealthy mouth can trigger a whole host of autoimmune issues in the rest of your body.
Periodontitis may cause a systemic anti inflammatory response and depending on your genetic and environmental predispositions can trigger:
Poorly managed type 2 diabetes
Cardiovascular disease, which is also an autoimmune disease
Rheumatoid Arthritis
Remember, there are over 100 systemic diseases that begin in your mouth. Yet, most of the time, dentistry is seen as a separate field to medicine, when really the disciplines need to be tied closer together.
(08/31/2024)by Robyn Puglia
More Information: https://robynpuglia.com/a-surprising-autoimmune-trigger-hiding-in-your-mouth/
Views: 427

What do you do if a filling falls out of your tooth?
It’s not every day that you lose a dental filling and quite frankly it’s not something people would be researching in advance just in case it was to happen. But alas, the fateful day has arrived and you now find yourself searching for an answer either because you’ve lost a filling or a family member has lost one.
Before you start panicking and thinking of the worst, let me just say that everything is going to be alright. I’m going to explain everything you need to know and what to do if your dental filling falls out.
Dental fillings don’t last forever
You might be wondering why did my filling fall out? There are a number of reasons why your dental filling has come loose or dislodged, and this includes not maintaining your daily oral care routine. If you’re guilty of letting a few days slide here and there, only flossing a few times a week, any tooth can start to develop dental decay (caries) which weakens the tooth or the filling.
Other reasons include:

Trauma to the tooth or impact to the mouth
Biting something hard or crunchy
Grinding your teeth
Tooth decay around the filling
If your filling comes loose or falls out, it’s important that you book in an appointment with your dentist as soon as possible to get it replaced.

5 Steps on what do I do if my dental filling falls out?
If your filling has fallen out, here’s 5 steps on what to do next.
Book an appointment with your dentist as soon as possible for a new filling. Let them know what’s happened and if you’re currently in pain. Make sure to ask for suggestions on how to protect your exposed tooth from any further damage if they are unable to see you right away.
Gargle salt water to keep the area clean. Mix ½ teaspoon of salt into a cup of warm water and give it a stir. Gargling salt water will help kill any harmful bacteria and remove any food debris that could potentially damage the tooth.
Maintain your daily oral care. This goes without saying, make sure to brush and floss your teeth at least twice a day. Pay extra attention to the area where the filling came out and brush gently.
Avoid biting or chewing on the exposed tooth.
Consider using a temporary filling material. Available at most local pharmacies, however make sure to consult with your dentist first. Remember, this is only a temporary solution until you are able to see your dentist.
Is a filling falling out a dental emergency?
To a certain degree, it’s a dental emergency, but at the same time it’s not. For the most part, if you simply follow the 5 steps mentioned above you’re going to be alright, so there’s no need to panic!
Make a few minor adjustments to your diet to include softer foods and avoid sugary things like soft drinks and candy, as they will only speed up tooth decay.
Can I eat if my filling falls out?
In short, yes you are perfectly OK to eat food providing you avoid any sugary drinks and food, and stay away from hard and crunchy items.
Avoid chewing on the exposed tooth, as this may cause further damage. As usual, make sure you’re brushing and flossing your teeth twice a day.
What should you do if you’re in pain?
If you’re unable to see your dentist for a few days and you’re in pain, here are some temporary options of relief:
Consider over-the-counter, nonsteroidal anti-inflammatory medication such as ibuprofen to help reduce pain and swelling.
You may also consider over-the-counter pain relief medication such as panadol to help reduce the pain.
Alternatively, you can apply clove oil to the exposed tooth and gum to help relieve pain, which can be purchased at any health food store or pharmacy.
Applying a cold compress or ice pack for 15minutes is always an effective method of relieving pain and swelling.
What happens if I ignore a loose filling?
Ignoring to replace a loose filling can result in further damage to the unprotected tooth. Not doing anything at all — none of the 5 steps mentioned above — allows bacteria and food particles into the space, causing tooth decay.
If exposed long enough, bacteria can make its way beneath the outer enamel and into the dentin. Exposed dentin can become very sensitive, and with further decay and damage to the exposed tooth, may require more extensive dental treatments. This includes a root canal, dental crown, or a tooth extraction.
What happens if you swallow a tooth filling?
If you managed to swallow your dental filling, don’t be alarmed as it should pass safely through your body. What’s more concerning is either breathing it in or inhaling it, as a loose filling can get lodged in the lungs and cause irritation, and potentially an infection.
We strongly recommend seeking medical attention as soon as possible.
How can you prevent a filling from coming loose?
When it comes to preventing a filling from falling out, there are no tricks. The key is to simply practice good oral hygiene and regular dental checkups. Here are some pointers to help prevent a filling from coming loose:
Brush and floss your teeth at least twice a day
See your dentist for regular checkups, scale and cleans
Brush or use a tongue scraper to remove any bacteria and freshen your breath
Make sure to use the right toothbrush and replace it every 3 to 4 months
Visiting your dentist at least every 6 months can help spot any potential problems with a filling or any other dental issues early before they become a serious problem. They will be able to advise if your filling is worn out and needs replacing before it falls out. When was the last time you saw your dentist?
(08/31/2024)by Dr Saurabh Rai
More Information: https://www.tandaradental.com.au/what-do-you-do-if-a-filling-falls-out-of-your-tooth/
Views: 416
Tooth Abscesses Versus Tooth Infections: What Is The Difference?
When teeth are healthy, strong and free from infection, they feel so comfortable that you are not aware of them. It is a very different story when a tooth becomes infected, and the pain of a tooth infection can be considerable. A dental abscess can feel even worse, but we find patients are frequently confused by the differences between these conditions.
What is a Tooth Infection?
Your mouth is home to hundreds of species of bacteria, many of which are benign, but some are harmful and can cause infection. Usually, your teeth have a hard outer coating of enamel that protects them and prevents bacteria from entering the tooth. You can have an infected tooth if you have a very deep cavity that isn’t treated, have gum disease (periodontal disease) or if a tooth is cracked. When a tooth is cracked, it lets in harmful bacteria. Even a small crack in a tooth can open up every time you bite down.
If tooth enamel is damaged through trauma or decay, these harmful bacteria can penetrate the tooth, soon reaching the tooth pulp. Your tooth pulp is right in the centre and contains the tooth nerve, connective tissues and blood vessels and extends into the tooth roots via root canals. When it becomes infected, it is extremely painful. The tooth nerve can also become damaged and inflamed if you take a blow to the mouth.
What are the Signs and Symptoms of a Tooth Infection?

Tooth infection symptoms usually include:
Throbbing pain in the affected tooth
Pain when you try to bite or chew on the tooth
Increased sensitivity to hot and cold foods and drinks
Sometimes a tooth will initially feel painful, but the discomfort might disappear. This doesn’t mean the infection is gone. It could mean the tooth nerve has died, so the tooth no longer feels painful, but the infection is still present. A tooth infection will not clear up on its own; your immune system cannot fight the infection as it can’t send antibodies to the inner part of the tooth. Instead, the infection will continue to spread beyond the tooth and the tooth root. It can start to affect the area between the tooth and your jawbone and turn into a tooth abscess.

What is a Tooth Abscess?
You have a tooth abscess if an untreated tooth infection spreads beyond your tooth root, and there are two main types of dental abscesses. Periapical abscesses are formed right at the tip of a tooth root. Periodontal abscesses form in the bone right next to the affected tooth and may be present if you have gum disease. If you have advanced gum disease, your gums can pull away from your teeth, creating deep pockets, called periodontal pockets, where bacteria can thrive, eventually causing an abscess.
What are the Signs and Symptoms of a Tooth Abscess?
An abscessed tooth can cause pain, but this isn’t always the case. Other symptoms include:
Swollen gums around the affected tooth
Pain when chewing
A persistent bad taste
Bad breath
Jaw pain
A severely abscessed tooth can cause a pimple to form on the gum, that if you press it will ooze pus. A dental abscess can affect overall health, as the bacteria can spread to other parts of the body. Signs to be aware of include swollen lymph nodes, facial swelling, fever and a general sense of feeling unwell. A tooth abscess may also cause trouble breathing or swallowing and a headache.
If you are concerned you have a dental abscess and think the infection has spread, you must seek emergency medical care. In rare cases, a severe tooth infection can spread to the brain and may become life-threatening.
Although similar conditions cause tooth infections and dental abscesses, treatment isn’t always the same. If you do have a painful tooth, contact Tandara Dental Centre as soon as possible. Dental pain isn’t normal and indicates a problem with a tooth that needs professional care. The sooner we can see you, the greater the chance we can successfully treat a tooth infection and save the tooth. It is much harder to save abscessed teeth.
What About Using Home Remedies for a Tooth Infection?
We know it is easy to look online and discover all sorts of remedies for tooth infections. However, home remedies for a tooth infection will not eliminate the bacteria causing this problem. You will need professional dental care. The sooner you see a dentist, the more quickly we can get rid of discomfort and pain and prevent the infection from spreading.
Diagnosing a Tooth Infection
When you visit Tandara Dental Centre, we can gently examine the tooth and quickly diagnose the reason for tooth pain. Our dentist will most likely take a dental x-ray of the tooth, showing the extent of the infection. Once we have this information, we can decide the best way to treat the infection and hopefully save the tooth.
Treating a Tooth Infection
If the infection has not spread into the surrounding tissue and is confined to the central part of the tooth, our dentist may recommend root canal treatment.
What is Root Canal Treatment?
Also called endodontic treatment, root canal treatment removes the infected dental pulp and the tissues extending into the root canals in the tooth roots. It is an intricate process that takes several visits to complete. Your tooth will feel much more comfortable after your initial visit to get rid of the infected tissues in the tooth, but it could still feel a bit sensitive for a while until it settles down.
Once all the infected tissue is removed, the tooth is disinfected, and medication is placed in the tooth to eliminate any remaining bacteria. We will insert a temporary filling to allow the medication to work. After several weeks, our dentist will remove the temporary filling, clean the tooth again and insert more medication and another temporary filling. The tooth is left to settle down for another few weeks to make sure it is infection-free. The next stage is to seal the tooth permanently with a material called gutta-percha. Sometimes a post is inserted into the tooth for additional strength.
Because a severely infected tooth has almost certainly lost a substantial part of its structure, it is restored with a dental crown. The crown fits over the entire tooth, sealing and protecting it from further infection. The crown restores appearance and strength, so you will be able to eat and talk comfortably and confidently. Your root treated tooth is now ‘non-vital’ as the nerve is removed and, consequently, more brittle but could last for years or life.
Sometimes a tooth that has received root canal treatment can become re-infected. At this stage, we would need to assess the tooth very carefully. It might be possible to perform a second root canal treatment to remove the infection, but we will need to discuss the possible risks and benefits of this approach. Treatment could be quite involved and costly and may have a limited chance of success. If this is the case, we might suggest removing the tooth and looking at suitable ways to replace it, such as placing a dental implant that can provide a long-term solution.
Diagnosing a Tooth Abscess
If we discover your tooth infection has spread beyond the tooth and that you have a tooth abscess, we will still try very hard to save the tooth. When we take the x-ray of your tooth, we can see if the abscess is treatable and any chance of saving the tooth. It depends on how far the infection has spread beyond the tooth.
Treating a Tooth Abscess
You will almost certainly need antibiotics, and the abscess or pocket of pus on the gums might need to be lanced so it can be drained. When we can catch a tooth abscess soon enough, root canal treatment could save it. Unfortunately, if the infection is severe, the only solution may be to remove the tooth to help the infection drain adequately. Leaving the tooth in place could cause additional oral health problems, especially as the infection will have killed the tooth nerve, and there will be no blood flow to the tooth root to help fight the infection.
What About Wisdom Tooth Infections?
Your wisdom teeth usually come through during the late teens and early twenties and can cause problems if they cannot erupt properly and become impacted or stuck underneath the adjacent teeth. Often there is inadequate room for wisdom teeth, so they can cause problems with overcrowding, affecting the adjacent teeth. Some wisdom teeth will partially erupt, so they are tricky to keep clean and become decayed and infected more easily. An impacted and infected wisdom tooth can cause toothache and jaw pain and must be removed.
If your wisdom teeth have yet to make an appearance, we will monitor them closely, checking their position in your jaw using digital dental x-rays. We prefer to take a wait and see approach, but if it is obvious these teeth cannot erupt without causing problems, we will suggest removing them before you get a wisdom tooth infection due to an impacted tooth.
What to Expect if You Need a Tooth Removed?
Tooth extraction is usually a routine procedure, and if you do need this treatment, we will do everything we can to ensure you feel comfortable. If you need a straightforward tooth extraction, local anaesthetic is usually enough to numb the tooth so we can quickly remove it. You should not feel any pain as the tooth is taken out.
If tooth removal is more complicated, it may require a surgical extraction, for example, if a wisdom tooth is partially or completely hidden in the gum. In this case, we can provide additional sedation if needed, so you feel deeply relaxed or will fall asleep during treatment. The tooth is then removed by making a small opening in the gum and jawbone to expose it. The tooth might be sectioned or cut into smaller pieces before we remove it, so we only need to make a small incision that will heal more quickly and comfortably.
What to Expect After Tooth Extraction?
Healing after tooth extraction should be uneventful and comfortable, and we will provide lots of information on how to care for the surgery site. An infection after tooth extraction only occurs in a tiny percentage of cases. When it does happen, it is very treatable. It could be a condition called dry socket, where the blood clot protecting an empty tooth socket becomes dislodged, allowing the socket to become infected and increasingly painful. In this case, we can clean out the socket so it can heal more easily.
Can I Prevent a Tooth Infection and Tooth Abscess?
Practising good oral hygiene can reduce the risk of developing a tooth infection and gum disease. We much prefer this preventive approach rather than seeing patients in pain or discomfort that could have been avoided.
Preventive Dentistry
Preventive dentistry is not complicated or time-consuming and could save you from pain and avoid spending hours in our dental chair. It is also much more cost-effective.
Regular Professional Dental Care
When you visit a dentist for regular checkups and cleanings, any signs of problems, such as gum disease or small lesions in teeth, are detected and easily treated before they can develop into larger and more troublesome issues. When we can catch dental problems in their early stages, the risk of developing tooth infections and tooth abscesses declines.
Professionally cleaning your teeth removes all the plaque and tartar buildup from teeth, reducing tooth decay and gum disease risks. Dental education is another important factor. When we clean your teeth, we can easily identify areas that need a bit more attention when you brush and floss. Our dental team can discuss how to clean your teeth more effectively and, if needed, can demonstrate different techniques and tools to use.
Taking Care of Your Oral Health at Home
A good oral hygiene routine takes less than ten minutes each day and will help you enjoy optimal oral health between checkups. The routine is extremely straightforward, simply involving brushing your teeth twice a day for two minutes each time. You need the full two minutes to clean all tooth surfaces thoroughly. If you use an electric toothbrush, it will have a built-in timer, but if you prefer a manual brush, be sure to set the timer on your phone or keep a small timer in the bathroom for this purpose. It is very easy to underestimate two minutes! You must floss your teeth once a day because plaque bacteria and food debris can easily become trapped between your teeth, greatly increasing the risk of a tooth infection or gum disease. Flossing is easy once you know how to do it correctly, so be sure to ask us for help if you struggle with this task. We can show you some techniques or other tools to try.
Tooth infections and tooth abscesses are unpleasant and can cause tooth loss but are often preventable with the proper dental care. By working together, we can help you achieve and maintain your best level of oral health.
(09/01/2024)by Tandara Dental Centre
More Information: N
Views: 336

Why does my tooth feel pressure when I bite it?
Have you ever bitten down on something hard like an ice cube or hard candy and felt an uncomfortable pressure or even pain in your tooth? This sensation is caused by the forces that are applied to the tooth when you bite down. Understanding why teeth feel pressure and pain during biting can help explain how your teeth work and why dental problems like cavities, cracked teeth, and root infections develop.
Human teeth are complex structures composed of multiple layers of mineralized tissues. Each tissue layer plays an important role. Here are the key anatomical components of a tooth:
Enamel
The outermost layer of the tooth made of the hardest substance in the body. Enamel is >95% mineral, with very little water or organic material.

It ranges from 2-3 mm thick and covers the visible crown portion of the tooth.
Enamel helps protect the inner tooth layers from bacterial acids and physical wear. It distributes bite forces across the underlying dentin.
Dentin
The layer immediately under the enamel that forms the bulk of the tooth structure.

Dentin contains 70% minerals like hydroxyapatite crystals reinforced with an organic collagen matrix. This gives dentin more flexibility than enamel.
It has tiny fluid-filled tubular structures leading towards the pulp that allow for sensory transmission.
Pulp
The innermost chamber filled with soft connective tissues, blood vessels, nerves, and lymphatic vessels.
The pulp provides nourishment to keep the tooth alive and sensory innervation.
It extends like a funnel down through the tooth roots. The openings at the root ends are called apical foramina.
Cementum
This bone-like calcified substance covers the dentin of the tooth roots.
It is softer than enamel and dentin but helps anchor the periodontal ligament fibers.
Cementum is produced continually to compensate for wear, keeping the attachment strong.
Periodontal ligament
The periodontal ligament is a dense fibrous connective tissue that essentially suspends the tooth in the jawbone socket and attaches via cementum.
This ligament has an excellent blood supply and contains mechanoreceptor nerve endings that provide sensory feedback.
It allows the tooth to withstand chewing forces and provides proprioceptive information about tooth positioning.
Why Do Teeth Feel Pressure When Bitten?
When you bite down, the force is transmitted through the enamel and dentin layers towards the pulp chamber. The pressure then compresses the soft pulp tissue, including the nerve fibers inside. This compression causes the nerve endings to fire and send signals indicating tooth pressure up to the brain via the trigeminal nerve.
The fluid in the dentin tubules also shifts, which bends and stimulates the nerve fibers near the pulp border to generate pressure sensations. Even slight stresses on the teeth may induce fluid flows inside the dentin that are perceived by the nerves.
The exact mechanisms that cause teeth to feel pressure include:
Force transmission
Enamel and dentin distribute and transfer bite force inwards towards the pulp chamber. This effectively squeezes the pulp.
Nerve compression
The pulp contains bundles of sensory nerves that are compressed by inward pressure on the tooth. This deformation of nerve fibers triggers electrochemical signals.
Fluid shifts
Pressure generates fluid shifts and flows inside dentin tubules and the pulp that stimulate nerve fibers.
Tooth deformation
Stress and strain deform the hard tooth structure slightly, activating nerve endings.
Periodontal sensation
Fibers of the periodontal ligament are also compressed and stimulated, contributing to pressure signals.
Odontoblast stimulation
The cells that line the pulp chamber (odontoblasts) may release signaling molecules in response to deformation, heightening nerve sensitivity.
Factors Affecting Pressure Sensation
Several factors can influence the intensity and location of the pressure feeling when biting down on a tooth:
Bite force
Harder bites exert more force and pressure on the teeth. More force equals more nerve stimulation.
Tooth health
Structural defects like cracks, caries, and large restorations reduce the enamel integrity. This results in less even force distribution and higher pressures on the pulp.
Restorations
Dental work like metal or ceramic fillings, inlays, onlays, crowns, bridges, and implants all transmit biting forces differently than natural tooth structure. More force may be placed on particular areas of the tooth, heightening sensitivity.
Occlusion patterns
The way the upper and lower teeth contact (occlude) affects how forces are distributed across and between teeth. Irregular contacts concentrate more pressure in certain areas.
Tooth type
The size, shape, and nerve density of different teeth affects pressure sensation. Incisors often feel more sensation than molars when loaded.
Age
As the pulp chamber naturally shrinks and dentin thickens with age, there may be progressively less sensation of pressure from biting.
Individual factors
People have varying levels of sensation in their teeth based on the neurologic structure. Some are just more sensitive.
Why is Pressure Sensation Important?
The ability to sense pressure and forces applied to our teeth is extremely important for several reasons:
Biting and chewing adjustment
Pressure provides feedback to the brain, allowing you to subconsciously adjust bite force and chewing to prevent damage to teeth. You bite hard enough to chew effectively but not so hard as to fracture teeth.
Tactile information
Along with touch receptors in the tongue, lips and cheeks, tooth pressure contributes to the detailed sensory information about food objects in the mouth. This guides positioning for effective chewing.
Dental disease detection
Unusual pressure sensations can provide an early warning of underlying dental problems like cracks, leaking fillings, or pulp inflammation. Catching issues early prevents more extensive damage.
Tooth vitality sensing
Monitoring nerve vitality through electric pulp testing relies on the teeth sensing pressure and transmitting those signals. A lack of sensation indicates the tooth pulp may be necrotic or compromised.
Protective neural reflexes
Extreme pressure sensed by the pulp nerves triggers reflexes to rapidly open the jaws and avoid fracture or periodontal injury.
Tooth eruption and development
Forces sensed by the periodontal ligaments help guide the emergence of teeth into proper alignment. Proper occlusion depends on this feedback.
When to Seek Help
While minor temperature or pressure sensitivity is common and not concerning, you should consult your dentist promptly if you experience:
Persistent sensitivity lasting more than 2-3 weeks
Pain that disrupts sleep or eating
Sensitivity with no apparent cause like cracks, erosion, or gingival recession
Sudden sharp sensitivity while drinking hot or cold fluids
Loosening teeth or changes in occlusion
Swelling of gums indicating potential infection
Any mouth pain that cannot be explained
Getting evaluated quickly allows early intervention before major pulp or root damage occurs. Not all sensitivity requires immediate treatment, but a dentist can monitor it for changes over time.
Conclusion
The sensation of pressure when biting arises from the innervation and force transmission properties of the tooth structure interacting with the oral environment.
This sensitivity is important for controlling bite forces, detecting dental issues early, and preserving tooth vitality.
Loss of pressure sensation can have serious consequences like excessive biting, unchecked infections, and unnecessary tooth loss.
Restorations aim to prevent damage in numb teeth or regenerate some sensory function.
In other cases, sensitivity results from exposed dentin rather than actual pulpal damage. Dietary acids, gum disease, and bruxism often contribute to this type of sensitivity.
Managing factors like brushing habits, enamel wear, and occlusal strains can help reduce discomfort from pressure sensitivity.
Severe or persistent sensitivity should be promptly evaluated by a dentist to check for underlying disease.
The intricacies of tooth anatomy and neurology determine the sensations perceived during biting and chewing. With proper home care and professional dental treatment, your natural pressure detectors can remain sensitive yet resistant to damage for decades to come.
(09/02/2024)by CDHP Dental Health Project
More Information: N
Views: 307
Can Poor Oral Health Make You Sick?
Dental hygiene is one of the most important health habits we can practice. We’re taught early on how important it is to take care of your teeth, passing that on to the next generation.
Although we know it’s essential to keep up on our flossing and brushing to ensure that our teeth stay clean and strong, many people don’t know how oral health can affect your whole body.
So, can poor oral health make you sick? Here’s a guide on six issues caused by bad dental hygiene and how holistic dentistry can help you and your family.
Many people know that good hygiene ensures that your teeth stay healthy and strong as time goes on, but it can also help prevent other health issues. Your body works as one system, which means that having problems in one area can often lead to other issues or symptoms.
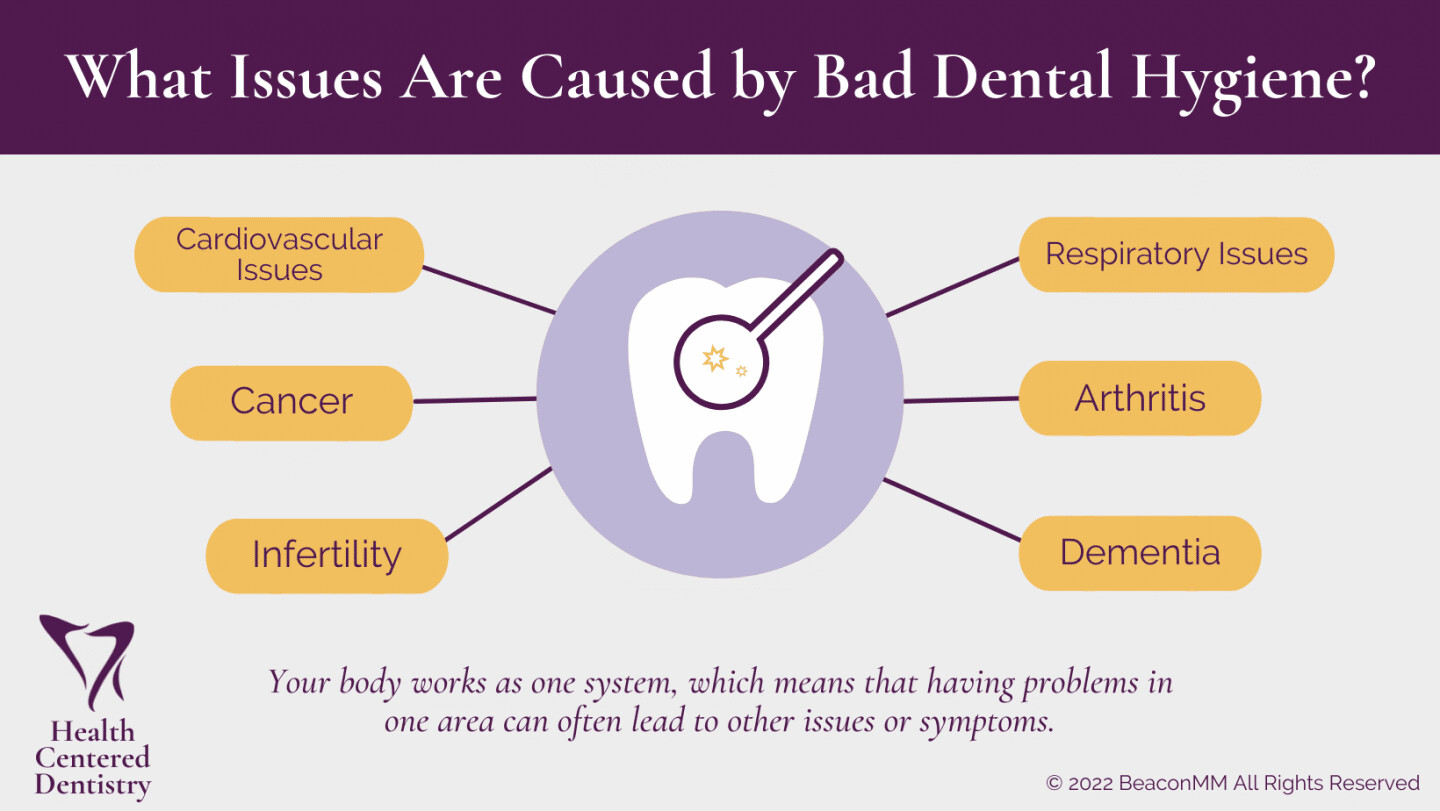
When you don’t take care of your teeth, you may experience stained teeth, decaying teeth, gum disease, and more. But what are some health issues that can arise from bad dental hygiene? The following are some health problems that have been linked to poor oral health.
1. Cardiovascular Issues
Poor dental health means an increased risk of bacterial infection in the bloodstream. This can affect the heart valves, which is particularly important for people with artificial heart valves.
There are also tooth loss patterns that are connected to coronary artery disease. Although poor oral health care isn’t the key to heart disease prevention, it can still affect your cardiovascular system.

2. Cancer
A study done in 2013 published by the Cancer Prevention Research journal found that people with poor oral health were at a 56% higher risk for developing human papillomavirus (HPV). Although this is commonly known as a sexually transmitted disease, certain types can form and infect the mouth and throat (oral HPV).
Oral HPV thrives at the base of the tongue and around the tonsils, causing oropharyngeal cancers. When the bacteria are allowed to grow and thrive in the mouth due to bad oral health practices, they can infect the mouth and throat, causing changes in cell growth.
3. Infertility
Women’s infertility can occur with poor oral health, as gum disease has been linked to fertility problems. Some women with endometriosis and polycystic ovarian syndrome are at greater risk of gum disease and can increase the risk of infertility problems. Women should maintain great oral hygiene, leading to increased chances of fertility, conception, and healthy babies.
Men also face infertility with poor oral health practices as they often end up with tooth decay and gum disease. These results are linked to low sperm counts and unhealthy semen, which increases the risk of male factor infertility.
4. Respiratory Issues
Respiratory issues are common with poor oral health. Your teeth and gums are reservoirs for bacteria to grow and travel down to the lungs and harm them. Plaque can also be a big issue, making it even more important to brush your teeth thoroughly. Some bacteria can also be inhaled into the lungs on tiny droplets of saliva.
People with gum disease can also worsen chronic inflammation in lung diseases like asthma and COPD. This can cause lung damage and further lung inflammation.
5. Arthritis
Having poor oral health and rheumatoid arthritis can be a bad combination for your health. This type of arthritis is a chronic inflammatory disorder that can affect the joints and other body systems. It occurs when your immune system attacks the tissues instead of the outside invaders.
Since this is an inflammatory disease, it can affect your oral health. This can often be the source of tooth decay and oral infections. To prevent poor oral health, ensure that you are staying on top of brushing and flossing your teeth to avoid issues of tooth loss or infections.
6. Dementia
A recent analysis led by NIA scientists suggests that bacteria that cause gum disease have been linked to the development of Alzheimer’s disease and related dementias, particularly vascular dementia. The team compared different age groups at a baseline with up to 26 years of follow-up for more than 6,000 participants. They analyzed antibodies against 19 oral bacteria and found that the Porphyromonas gingivalis is the most common culprit of gum disease.
The study results showed that older adults with signs of gum disease and mouth infections are more likely to develop Alzheimer’s during the study. And among those 65 years or older, the Alzheimer’s diagnoses and deaths were associated with antibodies against the oral bacterium. The long-term follow-up on this study suggested that oral infections proceeded with the diagnosis of dementia.
What Does Good Oral Hygiene Include?
Having good oral hygiene starting at a young age can save you from many issues in the future. As a kid through adulthood, it can help prevent problems such as cavities that hurt our teeth and are sometimes not fun to treat. Later in our lives, we can benefit from our good oral hygiene when our teeth stay healthy and strong, so we don’t need help from things like dentures.
There are some tips that you can follow to maintain good oral hygiene. For some, this may take an active effort to change your oral hygiene routine, but the habit will set in after a while, and you won’t have to make a second thought about it.
Some healthy oral habits to do include:
Brush your teeth thoroughly twice a day
Floss daily between the teeth to remove dental plaque
Visit your dentist at least once a year, even if you have no natural teeth or have dentures (it’s recommended to visit every six months)
Do not use any tobacco products
Limit alcoholic drinks
If you have diabetes, maintain control of the disease to limit the risk of gum disease
If your medication causes dry mouth, talk with your doctor about another option
See your doctor or dentist if you have sudden changes in taste and smell
These tips can help mitigate problems that come from poor oral hygiene. When you stay on top of your dental routine, it will help keep your teeth healthy and help clean stains caused by foods and drinks.
How Can Holistic Dentistry Help You?
A holistic dentist is a medical professional who takes a more natural, whole-body approach to treatment options. They see that your oral health is linked to your overall well-being and want to ensure that you’re getting treatments based on your overall health needs.
When visiting a holistic dentist, you’ll get the general care of flossing, brushing, and medicinal treatments. However, they may also recommend extra treatments such as:
Changes in your nutrition
Ozone treatment
Amalgam-free fillings
Comprehensive consultations and exams
Oral pH testing
They work to elevate your overall health and ensure that your dental hygiene is also treated. A holistic approach to dentistry can help you maintain your overall health and prevent further problems.
Health Centered Dentistry is a family dentistry in Anchorage, Alaska. We focus on integrative, whole-body dental care for your whole family. No matter the age, we’ll provide services such as regular check-ups, cosmetic procedures, restorative treatments, and oral surgery. Our most popular holistic services include safe amalgam removal, ozone, and testing for Vitamin C and pH levels.
We provide high-end dentistry services by expert staff using the most up-to-date dentistry equipment such as CBCT scans, CREC same-day dentistry, and implant surgical guides.
If you’re looking for a healthier approach to your dentistry services, holistic dentistry is the way to go. We have several amenity options that help you feel comfortable during our visit.
(09/02/2024)by Health Centered Dentistry
More Information: N
Views: 296

Gum Pain After Temporary Crown?
Dental procedures often involve intricate steps to ensure the health and longevity of your teeth. One such step is the placement of a temporary crown, a common practice in restorative dentistry.
While it's an essential part of the tooth restoration process, it's not uncommon for patients to experience some degree of gum discomfort or even pain following the procedure.
In this article, we’ll into the nuances of temporary crowns – from their purpose in dental treatments to the typical experiences of gum discomfort following their placement. Understanding that a certain level of gum pain is normal can help alleviate concerns as you navigate through this phase of dental care.
Quick Answer: Why Are My Gums Hurting After a Temporary Crown?
Temporary crowns are essential in protecting teeth after preparation for permanent crowns, but they can cause some gum discomfort.
Normal discomfort includes mild to moderate gum pain, especially in the first few days post-procedure, due to the minor damage that gets done to the gumline during a crown preparation and the temporary crown's less precise fit.
Severe pain, significant swelling, or bleeding are not normal and warrant immediate dental consultation.

Temporary crowns may not fit as comfortably as permanent ones, leading to more gum irritation.
Proper oral hygiene and care can help manage discomfort until the placement of the permanent crown.
The Temporary Crown Procedure
The journey to a permanent crown begins with a procedure that often requires a temporary placeholder. This step is crucial for multiple reasons.
The Temporary Crown Procedure
The journey to a permanent crown begins with a procedure that often requires a temporary placeholder. This step is crucial for multiple reasons.
Normal Gum Reactions Post-Procedure
Post-procedure discomfort is a common experience for many dental patients after the placement of a temporary crown. Here, we explore what constitutes normal gum reactions and the reasons behind these sensations:
Mild Gum Pain and Discomfort: After the placement of a temporary crown, it's typical to experience mild soreness or discomfort around the gumline. This can manifest as a dull ache, sensitivity to hot or cold foods, or a slight throbbing sensation.
Reasons for Discomfort:
Manipulation of Gum Tissue: During the crown preparation process, the gums are often manipulated or retracted, which can lead to temporary irritation and inflammation.
Adjustment Period: The gums and oral tissues may need time to adjust to the presence of the temporary crown, especially since it might not fit as precisely as a permanent crown.
Sensitivity Post-Preparation: The process of reshaping the tooth for the crown can also temporarily increase sensitivity in the surrounding gum tissues.
Understanding that this level of discomfort is a normal part of the recovery process can help patients manage their expectations and better handle the interim period before the placement of the permanent crown.
Temporary Crowns & Gum Health
While temporary crowns serve a vital role in the dental restoration process, their impact on gum health is an important consideration.
The fit of a temporary crown is less precise compared to a permanent crown. This can sometimes result in minor movement or rubbing against the gums, potentially causing irritation or even sores if the irritation is prolonged.
Maintaining Gum Health with a Temporary Crown:
Gentle Cleaning: It's essential to maintain good oral hygiene to prevent infection and promote healing. Brush gently around the temporary crown and use a soft-bristled toothbrush to avoid aggravating the gums.
Rinsing with Salt Water: A saltwater rinse can be soothing and help reduce inflammation and bacteria in the mouth.
Avoiding Hard or Sticky Foods: To prevent additional irritation or dislodging the temporary crown, avoid hard, sticky, or chewy foods.
Using Dental Floss Carefully: Be cautious when flossing around the temporary crown to prevent dislodging it. Slide the floss out rather than lifting it out to avoid pulling on the crown.
Signs of Concern: When to Contact Your Dentist
While some discomfort is expected after receiving a temporary crown, certain symptoms can indicate complications requiring professional attention:
Severe Pain: If the pain intensifies or becomes sharp and unbearable, it's a sign that something may be wrong. Severe pain can indicate nerve damage, an infection, or an ill-fitting crown.
Significant Swelling: Some swelling is normal, but if it becomes pronounced or spreads beyond the immediate area of the tooth, this could signify an infection or an allergic reaction.
Persistent Bleeding: A small amount of bleeding immediately after the procedure is normal. However, ongoing or heavy bleeding is a cause for concern and warrants immediate dental consultation.
Other Symptoms: Pus discharge, a noticeable odor, or an allergic reaction to the crown material are all reasons to contact your dentist.
Promptly consulting your dentist when these symptoms arise is crucial. They can diagnose the issue and provide the necessary treatment, such as adjusting the crown or prescribing medication, to resolve the problem and ensure your comfort and safety.
Managing Normal Discomfort
While waiting for your permanent crown, here are some effective strategies to manage normal levels of discomfort associated with a temporary crown:
Saltwater Rinses: Gargling with warm salt water can help soothe irritated gum tissue, reduce swelling, and flush out bacteria.
Avoid Extreme Temperatures: Steer clear of excessively hot or cold foods and beverages, as temporary crowns can make your teeth more sensitive to temperature changes.
Soft Foods: Stick to soft foods that require minimal chewing to reduce the pressure on your temporary crown and surrounding gums.
Over-the-Counter Pain Relievers: Medications like ibuprofen or acetaminophen can be effective in managing pain. However, always follow the recommended dosage and consult your dentist or doctor if you have any concerns about these medications.
Good Oral Hygiene: Continue brushing and flossing regularly, but be gentle around the temporary crown to avoid dislodging it.
Rest: Sometimes, simply giving your mouth a break and avoiding unnecessary stress on your teeth can help alleviate discomfort.
By implementing these simple self-care measures, you can effectively manage normal levels of discomfort associated with a temporary crown and maintain your oral health until the permanent crown is placed.
Transitioning to a Permanent Crown
The transition from a temporary to a permanent crown marks the final step in your dental restoration process. Here's what to expect:
Transition Process: Your dentist will carefully remove the temporary crown and replace it with the permanent one. This final crown is crafted to fit your tooth precisely, ensuring optimal comfort and functionality.
Decreased Discomfort: You'll likely notice a significant reduction in discomfort once the permanent crown is in place. A well-fitted permanent crown protects the tooth, fits seamlessly with your bite, and alleviates the irritation caused by the temporary crown.
Final Adjustments: Your dentist may make small adjustments to ensure the crown fits perfectly and doesn't interfere with your bite or adjacent teeth.
Long-Term Comfort: Permanent crowns are designed to feel like your natural teeth, offering a comfortable and lasting solution to dental issues.
Final Thoughts
Understanding the difference between normal post-procedure discomfort and signs of complications is crucial after receiving a temporary crown. While mild pain and sensitivity are typical, severe pain, significant swelling, or persistent bleeding are warning signs that require immediate attention from your dentist.
Maintaining good oral hygiene, like gentle brushing and flossing, is vital for the health of your temporary crown and overall oral health. Additionally, managing minor discomfort with simple home remedies can make the period with your temporary crown more bearable.
Finally, remember that transitioning to a permanent crown usually brings relief and improved oral function. Ensuring you follow up with your dental appointments for the placement of the permanent crown is key to completing your dental restoration journey successfully. By staying informed and proactive about your dental health, you can navigate the temporary crown experience with confidence and comfort.
(09/03/2024)
by Burlington Dental Center
More Information: https://burlingtondentalcenterks.com/gum-pain-after-temporary
Views: 331

Oral Issues That Can Damage Oral Health
Infections in the mouth happen more often than you may realize. Improper hygiene, vices and physical contact are just some of the causes. Being aware of what’s going on within your mouth can save major health problems down the road from common oral issues.
Some of the simplest causes of problems are also the easiest to take care of.
Tooth decay:
Also called dental caries or cavities. Your teeth break down due to acids that are caused by bacteria. If you have pain while eating, pits in the tooth surface, or dark marks in the tooth; chances are you already have cavities.

See your dentist in Airdrie right away to have it be a minor fix.
Regular flossing and brushing along with dental cleanings and checkups can help prevent this from occurring in the first place.
Gingivitis:

Gingivitis is caused by plaque that becomes attached to your tooth surfaces. It causes your gums to get red and irritated. Left long enough it will cause them to bleed. Regularly going to your dentist for a cleaning is important as they will remove the plaque for you.
Better yet, practice good oral hygiene, especially flossing to make sure the areas your brush can’t reach get properly cleaned. Don’t ignore gingivitis as it will progress to a more virulent strain of gum disease. Isn’t five minutes a day worth the investment to avoid the pain this could cause?
Gum Disease:
a.k.a. periodontal disease, this one makes your gums more inflamed than gingivitis and affects the tissue around your teeth. The tissue pulls away from the tooth leaving pockets where particles can get trapped, causing an infection. If you have ignored your gingivitis before, do not let this one pass. If you are having trouble with your gums, you should visit your dentist immediately.
Once again, good oral hygiene, brushing and flossing, can help prevent this from becoming a problem.
Cold Sores:
a.k.a. oral herpes is a viral infection caused by the herpes simplex virus. There are names for every herpes infection that occur in your body. Oral herpes is a very visible infection that occurs on your face or in your mouth. If your lip starts itching or maybe you already have fever blisters, chances are good this is a cold sore. Cold sores may take two to four weeks to disappear. While the cold sore is present, you’ll probably feel pinching-like pain in the affected area. Herpes will usually let itself show for a period of time with some active cases, but it will also decrease depending on severity. There are medicated creams that can help speed the process of healing the outbreak. Herpes is not limited to cold sores so watch out for unexplained fever, swollen lymph nodes, muscle pain and headaches as the first symptoms to be concerned about.
Keeping your lips from drying out by using a lip balm daily can help prevent these from breaking out, but discuss options to control them with your doctor or dentist if you get them frequently.
Taking care of your oral health is simple and easy. Brush after meals and before bed and floss once or twice a day. There are many electric toothbrushes that can help make this a light task. There are also many aids to make flossing less of a bother as well. Regular dental checkups and cleanings should also be a necessary part of your routine.
(09/03/2024)by Airdrie Springs Dental
More Information: https://www.airdriespringsdental.ca/common-oral-issues/
Views: 325

How can psoriasis affect the mouth and tongue?
Psoriasis can affect any area of the body, including the mouth and tongue. The condition can cause cracks on the tongue or smooth patches, a complication called geographic tongue.
Psoriasis is a chronic autoimmune condition that causes a person’s skin to grow faster than average, resulting in changes in skin color and, often, scaly patches.
These patches can form anywhere on the body. Less frequently, psoriasis affects the mouth. Oral psoriasis can cause discolored patches with yellow or white edges to form on the tongue.
Psoriasis can cause noticeable changes in the tongue’s color, texture, and feeling.

For example, people with psoriasis are more likely to develop an inflammatory condition called geographic tongue.
Although psoriasis on the tongue is rare, symptoms include:
discolored patches with yellow or white borders
swelling and discoloration on the tongue

smooth patches
fissures or cracks in the surface of the tongue
Psoriasis on the tongue can be tricky to diagnose because signs may be mild or even unnoticeable. However, for some people, these symptoms can lead to pain or swelling so severe that it makes eating or drinking difficult.
A thorough examination and testing can help a doctor determine if a person with a geographic tongue has oral psoriasis.
How does psoriasis affect the mouth, gums, and lips?
Psoriasis typically does not affect the mouth. When it does, people may experienceTrusted Source the following symptoms:
peeling skin on the gums
sores or pustules in or around the mouth
pain or a burning sensation when eating hot or spicy foods
a noticeable change in taste
In most cases, the patches or sores will appear inside the cheeks.
Risk factors for psoriasis on the tongue
To develop psoriasis, a person must have at least one relevant gene and experience exposure to triggers.
Several factors can triggerTrusted Source psoriasis, including:
stress
medications
infection
injury to the skin
Psoriasis may affect only one area of the body or several, and it may arise in new places. No matter where it occurs, psoriasis is not contagious, so a person cannot pass on the condition to others.
Treatment
Many treatments can helpTrusted Source people manage their psoriasis symptoms.
Oral psoriasis sometimes requires no treatment. However, consult a doctor if the symptoms interfere with daily activities.
For people with oral psoriasis, the doctor may prescribe anti-inflammatories or topical anesthetics such as lidocaine. These medications can help reduce inflammation and pain, making it easier to eat and drink.
A person may notice improvements in oral psoriasis if they treat body-wide symptoms. Typically, when treating psoriasis, a doctor will prescribe medications such as:
non-biological medications, such as methotrexate
biological treatments, such as guselkumab
acitretin
cyclosporine
phototherapy
topical treatments such as steroid creams, emollients, or ointments
Prevention
To prevent psoriasis symptoms from flaring up, it can help to avoid triggers. For psoriasis on the tongue, a person can:
avoid spicy or very hot foods
quit smoking
use mouth rinses
practice good oral hygiene
It can also help to reduce stress, which can worsen symptoms.
(09/04/2024)by Medical News Today
More Information: N
Views: 397

