Dentists Journal
Top Ten Stories of the Week
8/3/2024
All Dentists Journal · Previous Week · This Week · All Time List · Headlines

What Can You Do To Prevent Mouth Problems
Most of us tend to be too focused on our outer appearance. But, we often cease to forget our mouth problems. It is an essential part of our overall health and well-being. Maintaining oral hygiene is a key component of our health, well-being, and even our personality. However, if you’re negligent towards oral and dental hygiene, then you may get yourself in serious trouble.
Most Common Mouth Problems
Here are some of the most common mouth problems
1. Bad Breath

Bad breath is a very prevalent mouth problem and could be straightaway embarrassing. Persistent bad breath is usually caused by the smelly gases released by the bacteria that coat your teeth, gums, and tongue. Also, bits of food that get stuck between the teeth and on the tongue, may rot cause an unpleasant smell. Strong foods like coffee, garlic, and onion can contribute to bad breath.
Additionally, other habits like smoking and alcohol may lead to bad breaths. Smoking causes straining, loss of taste, and irritation of gums. If you are suffering from bad breath, then there’s high time that you establish a proper oral hygiene routine.
Basic steps like Brushing twice a day and flossing regularly can help you get rid of bad breath. Your dentist will clean all the plaque in your teeth and would also teach you the appropriate ways of cleaning your mouth and tongue.
2. Tooth Decay

Tooth decay, also known as cavities, is a very prevalent dental problem. Tooth decay occurs when plaque, the thin film that forms on the teeth, combines with the sugars and/or starches of the food you eat. This combination produces acids that attack tooth enamel. You can get cavities at any age — they aren’t just for children. As you age, you can develop cavities and your tooth enamel starts eroding.
Eating healthy foods and avoiding snacks and drinks that are high in sugar are also ways to prevent decay. Your dentist can recommend further treatments that may help reduce your risk. If you need a recommendation, you can check out dental care like dental implants in Maywood.
3. Gum Disease
Gum disease, also known as periodontal disease or gingivitis, is an infection that happens when the gums surrounding the teeth become red and swollen. It is also one of the major mouth problems.
The root of all gum disease is plaque. Plaque is a thin film of bacteria that forms on the surface of our teeth every day. That’s why everyone is at risk for gum diseases. Smoking is one of the most significant risk factors. Diabetes and dry mouth can also increase your risk. Other notable symptoms include bad breath, red, swollen, tender, or bleeding gums, sensitive teeth, and trouble chewing.
4. Oral Cancer
Oral cancer is a serious oral problem and deadly disease that affects millions of people globally. The Oral Cancer Foundation estimates that someone in the United States dies every hour from oral cancer, but it is often curable if diagnosed and treated in the early stages. It is most often seen in people over the age of 40, particularly men. The most common risk factors are cigarette smoking and alcohol use, including chewing tobacco. Oral cancer is also linked to HPV — a sexually transmitted wart virus.
Oral cancer can often be detected in the early stages by regular dental visits. You may ask your dentist whether an oral cancer exam is part of their usual checkup. Some of the most common symptoms include trouble in chewing, swallowing, or moving your tongue or jaw. If diagnosed early, there are good chances of treating and curing it.
5. Mouth Sores
A cold sore is a small, painful, raised area of small, fluid-filled blisters. There are several types of mouth sores and they can be quite painful and bothersome. Unless a mouth sore lasts more than two weeks, there is usually nothing to worry about and will disappear on its own.
Common mouth sores occur inside the mouth and not on the lips. They are most often not contagious and can be triggered by many different causes. They are only a concern if they don’t even go away after two weeks.
Mouth sores or cold sores are caused by the Herpes Simplex virus and occur as lesions on the edge of our lips. They are contagious and will come and go but are not completely treatable.
6. Dental Erosion
Dental erosion or tooth erosion is the loss of tooth structure caused by an acid attack. The acidity may be caused by acidic foods and drinks like soda, fizzy drinks, and citrus fruit. The symptoms of tooth erosion can range from sensitivity to more severe problems such as the wearing away of the tooth surface. Tooth erosion is more common than people might think, but it can also be easily treated.
With regular check-ups and follow up with your dentist, you can prevent the problem from getting any worse and the erosion from escalating any further.
7. Sensitive Teeth
Do you also feel a slight tinge when eating ice cream? There are high chances you are suffering from a sensitive tooth.
Tooth sensitivity is a common mouth problem that affects millions of people worldwide. Sensitivity may involve anything from a mild twinge to severe discomfort that can persist for a significant time. The experiencing pain or discomfort in your teeth can result from sweets, cold air, hot drinks, cold drinks, or ice cream. Some people with sensitive teeth even experience discomfort from brushing and flossing. But, the good news is that sensitivity can be easily treated.
8. Dry Mouth
You need saliva in your mouth to be able to function properly. Saliva keeps your mouth moist, breaking down your food, and helping you swallow.
There are several symptoms that indicate a dry mouth. Of which, the most noticeable one is a dry mouth. Some people say their saliva is getting thick and sticky, making it hard to talk or swallow. Quite often, dry mouth results as a side effect of some specific medications like blood pressure, heart and depression tablets
You may consult your dentist but there’s actually no foolproof treatment for dry mouth. Though, you may certainly take steps to prevent it.
(07/27/2024)by The Voice Of Woman
More Information: https://www.thevoiceofwoman.com/what-can-you-do-to-prevent-mouth-problems
Views: 386

Can Magnesium Supplements Cause Yeast Infections?
There are many different types of candida, and they can each be affected by magnesium in different ways.
For instance, Candida Albicans is the most common type of candida, and it is known to cause thrush. This type of candida can be inhibited by magnesium, as it has been shown to reduce the growth of Candida Albicans. However, another type of candida, called candida tropicalis, actually uses magnesium as a nutrient for growth. This means that increasing magnesium levels may actually cause this type of candida to grow more quickly.
So, the way Magnesium affects candida can vary depending on the type of candida that is present. In general, though, magnesium is thought to be an effective anti-fungal agent against most types of candida.
Therefore, it is important to consult with a medical professional before taking magnesium supplements if you have any form of candida.

What deficiency causes yeast infections
Candida albicans is a fungus that normally lives in the human body, usually in harmony with other organisms that make up the body’s microbiome. However, when there is an imbalance in the body’s natural flora, Candida can overgrow and cause infections. Some of the deficiencies that can trigger Candida overgrowth include:
CARD9: Studies have shown that people with deficiencies in the CARD9 gene are more susceptible to Candida infections. This gene is responsible for encoding a protein that helps regulate the immune system.
Vitamin D: Vitamin D is essential for a healthy immune system. A deficiency in vitamin D can lead to an overgrowth of Candida.

Vitamin B6: Vitamin B6 helps to maintain balance in the gut by supporting the growth of healthy bacteria. When levels are low, however, it can allow Candida to flourish, leading to yeast infections. Vitamin B6 can be found in many foods, including poultry, fish, potatoes, and bananas. Therefore, eating a balanced diet rich in this vitamin can help to prevent yeast infections.
Vitamin B12: Vitamin B12 is another vitamin that helps to keep the body’s microbiome in balance. A deficiency in this vitamin can lead to an overgrowth of Candida, which can cause yeast infections. Vitamin B12 can be found in many foods, including meat, poultry, fish, and eggs. Therefore, eating a balanced diet that includes these foods can help to prevent yeast infections.
Zinc: Zinc is a mineral that helps the body fight off infections. A deficiency in zinc can make you more susceptible to Candida infections.
Probiotics: Probiotics are live bacteria that help maintain a healthy balance of organisms in the gut. A lack of probiotics can lead to an overgrowth of Candida.
Magnesium: Magnesium is a mineral that has many functions in the body, including helping to maintain a healthy immune system. A deficiency in magnesium can make you more susceptible to Candida infections.
What is the best supplement for yeast infections
Supplements are not the only answer for candida overgrowth, as a balanced diet is also important. However, certain supplements may help to prevent or treat yeast infections. These include:
Probiotics: Probiotics are live bacteria that help maintain a healthy balance of organisms in the gut. Probiotics can be found in supplement form or in fermented foods such as yoghurt, kimchi, and sauerkraut.
Vitamin D: Vitamin D is essential for a healthy immune system. Vitamin D can be found in supplement form or in fortified foods such as milk, orange juice, and cereal.
Magnesium: Magnesium is a mineral that has many functions in the body, including helping to maintain a healthy immune system. Magnesium can be found in supplement form or in foods such as dark leafy greens, nuts, and seeds.
Hope this article has given you a clear idea of ‘Can Magnesium supplements cause yeast infections. Candida overgrowth can be triggered by a variety of factors, including deficiencies in certain vitamins and minerals. Of all, Magnesium is a mineral that has a significant role in handling yeast infections. Therefore, taking magnesium supplements may help to prevent or treat yeast infections. However, it is important to consult with a medical professional before taking magnesium supplements if you have any form of candida.
(07/27/2024)by Healthy Supplements Guide
More Information: N
Views: 1,142
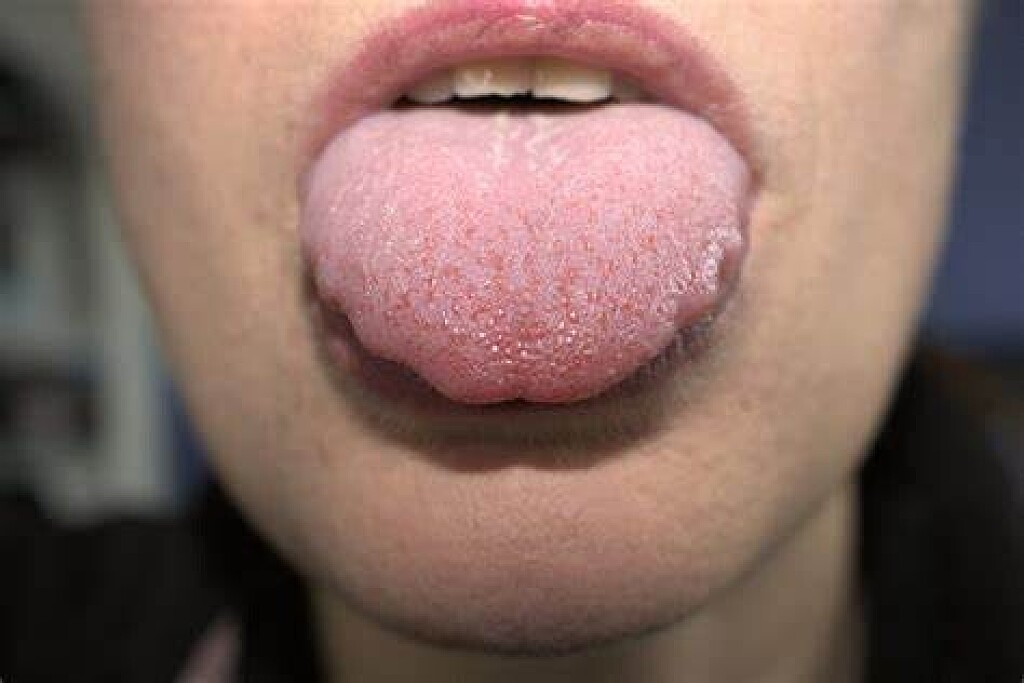
Scalloped Tongue May Be a Symptom of Bad Bite
A scalloped tongue is when your tongue has half-circle indentations around the edge. Scalloped tongue causes are usually when your tongue presses up against your teeth, either constantly or regularly, pressing the shape of your teeth into the sides of the tongue. It may also look like a rippled tongue.
There are many potential scalloped tongue causes and all should be checked out to eliminate the most serious possibilities.
What Causes a Scalloped Tongue?
Swelling of the tongue could be the reason why your tongue is pushing up against your teeth. If this is the case, it may be due to a number of different systemic conditions. Hypothyroidism is the most common cause of a swollen tongue, but there are others. Hypothyroidism condition is when your thyroid is not producing enough of its vital hormone, which controls how your body uses and stores energy. Hypothyroidism can lead to obesity, heart disease, and other serious health consequences.
Nutrient deficiencies may have links to a swollen tongue. In Chinese medicine, a swollen tongue is related to a spleen deficiency.
Scalloped Tongue Causes and Your Teeth
A scalloped tongue doesn’t have to be swollen to press against your teeth regularly. Instead, your tongue may be pressing against your teeth because your lower arch is too narrow. Your tongue might not have enough room. In some cases, it’s possible to remodel the lower jaw to increase the room for your tongue, especially if the problem is detected at a young age.
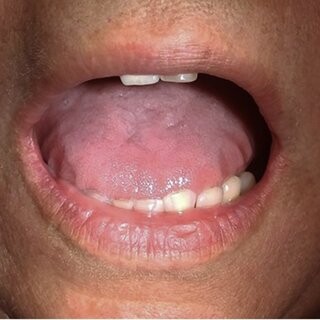
But what if there’s plenty of room for your tongue, and it’s still scalloped? In this case, it’s likely that your tongue is deliberately pressing up against your teeth on a regular basis. This may be because your bite isn’t coming together properly to stabilize your jaw for swallowing. To attempt to make up for this, your tongue pushes up against your teeth to help stabilize them. This repeated motion causes the tongue to acquire a scalloped shape. It can also lead to drifting of the teeth, causing the bite to become even less stable.
A bite that isn’t stable for swallowing is probably not stable for all the other muscular tasks your jaw muscles perform, such as chewing or assisting balance of the head. Even if you don’t have it yet, this could contribute to the development of TMJ, including jaw pain, headaches, and other symptoms.
Scalloped Tongue Treatment
The treatment for a scalloped tongue is usually determined based on what’s causing it. By treating the cause of the rippled tongue, you can treat the rippled tongue. Some common scalloped tongue treatments include:
Nasal dilators
CPAP machine
Surgery to correct the tongue shape or size
Surgery to remove abnormal or excess tissue or cells
Thyroid hormone medications
Dental devices such as mouth guards
Anti-inflammatory medications
A scalloped tongue is an important symptom that you should talk to your doctor about. If your doctor clears your health, it’s time to see a neuromuscular dentist.
(07/26/2024)by Smile Columbia
More Information: https://www.tmjtreatmentsc.com/patient-education/scalloped-tongue-may-be-a-symptom-bad-bite/
Views: 450

Mouth Problems: How to Remedy Difficulty When Eating
Many people experience mouth problems that make eating difficult. These problems can make mealtimes a pain, whether it’s due to gum disease, tooth decay, or dry mouth. Some people may even find that they’re losing weight because they’re unable to eat as much as they used to. However, there are ways to remedy the situation. This blog post will explore some of the most common mouth problems and how to fix them.
Gum Disease
Gum disease is an infection that causes swelling, redness, and bleeding. If left untreated, it can lead to tooth loss. The best way to prevent gum disease is to brush and floss regularly. If you already have gum disease, your dentist may recommend deep cleaning or surgery.
You want to avoid gum disease not just for your teeth but also for your overall health. Gum disease has been linked to heart disease, stroke, and other health problems. If you’re having trouble with your gums, see a dentist as soon as possible. Some treatment options can help improve your gum health, from deep cleanings to surgery.

Missing Teeth
Missing teeth can make eating difficult, especially if they’re in the front of your mouth. If you have missing teeth, there are a few options for replacement, including dentures, implants, and bridges. Dentures are the most affordable option and can be removed for cleaning. Dental implant surgery is more expensive but gives you a more natural-looking tooth. Bridges are usually used when you have healthy teeth on either side of the missing tooth.
Regardless of your choice, it’s essential to replace missing teeth. This will help you eat better and also improve your smile. It would help if you talked to your dentist about which option is best for you.
Tooth Decay

Tooth decay is caused by bacteria that eat away at the enamel of your teeth. It can cause pain, sensitivity, and tooth loss. To prevent tooth decay, brush your teeth twice daily and avoid sugary foods and drinks. Your dentist may recommend a filling or crown if you already have tooth decay. Some tooth decay can be repaired at home with a filling kit, but more severe cases require a dental visit.
If you have a tooth that is severely decayed, it may need to be extracted. This can be a painful process, but getting rid of the decay is essential before it spreads to other teeth. Your dentist will numb the area before extracting the tooth to minimize discomfort.
Dry Mouth
Dry mouth is a condition in which there is not enough saliva in the mouth. It can be caused by certain medications, medical conditions, or simply not drinking enough water. A dry mouth can cause difficulty eating, as well as bad breath. To treat dry mouth, drink plenty of water and chew sugarless gum or candy. You may also need to take medications or use artificial saliva products.
Your teeth and gums need saliva to stay healthy. Saliva helps wash away food and bacteria and contains minerals that help keep teeth strong. If your teeth are damaged by decay, it’s more difficult for saliva to repair the damage. This is why it’s essential to keep your mouth moist by drinking plenty of water and using artificial saliva products if needed.
Misaligned Teeth
Some people have teeth that are not aligned properly. This can make it difficult to bite and chew food. If your teeth are misaligned, you may need to see an orthodontist for treatment. Treatment options include braces and clear aligners.
If you have misaligned teeth, you may not need treatment if it doesn’t cause pain or discomfort. However, if your teeth are making eating difficult, you should talk to your dentist or orthodontist about treatment options.
Sensitive Teeth
Sensitive teeth may hurt when exposed to hot or cold temperatures. It can also be sensitive to sweet, sour, or acidic foods and drinks. Sensitive teeth can be caused by gum disease, decay, or worn tooth enamel. To treat sensitive teeth, use toothpaste for sensitive teeth and avoid foods and drinks that trigger the pain. You may also need to see your dentist for professional treatment.
You should also avoid foods and drinks that are acidic or high in sugar, as these can contribute to tooth decay. See your dentist for an evaluation and possible treatment if you have sensitive teeth.
There are ways to remedy the situation if you’re experiencing difficulty eating due to mouth problems. Gum disease, tooth decay, and dry mouth are all common issues that can make eating messy or painful. However, by brushing and flossing regularly, avoiding sugary foods and drinks, and drinking plenty of water, you can help keep your mouth healthy and free from problems. If you experience difficulties, talk to your dentist about possible treatments such as fillings or crowns.
(07/26/2024)by B2 Cafe
More Information: https://b2cafe.com/mouth-problems/
Views: 357

Abscess In The Mouth: Diagnosis, And Treatment
Abscess in the mouth can be an uncomfortable and painful oral condition that requires prompt attention. They are typically caused by bacterial infections and can develop in various areas, including the gums, teeth, and surrounding tissues. This comprehensive guide will explore the causes, symptoms, diagnosis, and treatment options for abscesses in the mouth, helping you understand this condition better and make informed decisions about your oral health.
UNDERSTANDING ABSCESSES IN THE MOUTH
Definition of an Abscess:An abscess is a localized collection of pus that forms due to the body’s natural response to infection. In the context of the mouth, it occurs when bacteria invade the tissues, leading to an inflammatory response and the formation of a pus-filled cavity.
Causes of Mouth Abscesses:Mouth abscesses are primarily caused by bacterial infections. The most common bacteria associated with oral abscess is Streptococcus species, including Streptococcus mutants and Streptococcus intermedius. Poor oral hygiene, tooth decay, gum disease (periodontitis), and dental trauma are common factors that contribute to the development of abscesses.

SYMPTOMS OF ABSCESSES IN THE MOUTH
Localized Symptoms:Severe toothache or gum painSwelling and redness in the affected areaIncreased sensitivity to hot or cold substancesPresence of a bump or swelling filled with pusFormation of a fistula (a small channel) that drains pusFoul taste or odor in the mouthDifficulty in opening the mouth or swallowing
Systemic Symptoms:FeverGeneralized malaiseSwollen lymph nodesDifficulty in breathing or swallowing (in severe cases)
DIAGNOSIS OF MOUTH ABSCESSES

Clinical Examination:During a dental examination, the dentist will visually inspect the oral cavity, looking for signs of inflammation, swelling, or pus-filled areas. They will also assess the patient’s medical history and ask about the symptoms experienced.
Imaging Techniques:To confirm the diagnosis and determine the extent of the infection, the dentist may request imaging tests such as X-rays, dental cone-beam computed tomography (CBCT), or ultrasound. These tests help identify the location and size of the abscess, as well as any associated dental or periodontal problems.
Aspiration or Culture:In some cases, the dentist may perform an aspiration procedure, in which they use a needle to withdraw a sample of pus from the abscess for laboratory analysis. This helps identify the specific bacteria causing the infection and determine the most effective antibiotic treatment.
TREATMENT OPTIONS FOR MOUTH ABSCESSES
Incision and Drainage:In many cases, the primary treatment for a mouth abscess involves incision and drainage. The dentist will numb the area with a local anesthetic, make a small incision in the abscess, and allow the pus to drain out. This procedure is usually followed by thorough cleaning of the area and may require the placement of a temporary drain.
Antibiotics:To control the infection and prevent its spread, antibiotics are often prescribed. The choice of antibiotic depends on the severity of the abscess, the patient’s medical history, and the results of the pus culture. It is crucial to complete the full course of antibiotics as prescribed by the dentist.
Root Canal Treatment or Tooth Extraction:If the abscess is caused by a severely infected tooth, the dentist may recommend either a root canal treatment or tooth extraction. A root canal treatment involves removing the infected pulp from the tooth and filling it with dental material to prevent reinfection. If the tooth is severely damaged or cannot be saved, extraction may be necessary. The dentist will discuss the options and help determine the best course of action.
Scaling and Root Planing:If the abscess is associated with gum disease, a procedure called scaling and root planing may be performed. This deep cleaning treatment removes plaque and tartar from the surfaces of the teeth and their roots, helping to eliminate the bacteria causing the infection.
Pain Management:During the treatment and recovery period, pain management is essential. The dentist may prescribe pain medications or recommend over-the-counter pain relievers to alleviate discomfort. Applying a cold compress to the affected area can also help reduce swelling and pain.
(07/28/2024)by Swiss Dent Bodrum
More Information: N
Views: 445

Home Remedies to Get Rid of Burning Mouth Syndrome
Do you wake up with a burning sensation on your tongue, even though you haven’t even taken a sip of your hot cup of coffee? Does the burning last all day long, making it difficult to eat or drink anything? If so, it is likely that you are suffering from what’s known as burning mouth syndrome (BMS).
This syndrome is characterized by constant or intermittent pain, discomfort, or burning sensation in the tongue, gums, lips, insides of cheeks, the roof of the mouth, or entire oral cavity. It commonly affects the tongue. Thus it is sometimes called burning tongue syndrome.
Many people who suffer from BMS indicate anxiety, depression, personality disorders and impaired quality of life (QoL). While BMS can affect anyone, it is more common in premenopausal and postmenopausal women.
The definitive cause is still unknown, and it can be challenging for doctors to diagnose. A number of tests may be performed, such as an MRI or CT scan, a biopsy of a sample of tissue from the mouth, an allergy test, and complete blood count. Some of the tests are used to rule out other conditions.

Causes of Burning Mouth Syndrome
BMS can be categorized as primary or secondary.
Primary burning mouth syndrome: This condition is idiopathic, meaning no obvious abnormality or cause can be identified.
Secondary burning mouth syndrome: The following underlying conditions can lead to secondary BMS, meaning it is a result or symptom of the underlying condition.

Dry mouth, also known as xerostomia.
Fungal infections.
Geographic tongue, in which map-like patches appear on the tongue.
the
Ill-fitted dentures leading to irritation in the oral cavity.
Allergies to certain foods, fragrances or substances used for oral care.
Gastroesophageal reflux disease (GERD), which involves reflux of stomach acid that can cause burning sensations.
Certain medications.
Unhealthy oral habits that can lead to irritation in the mouth.
Hypothyroidism or other endocrinal disorders.
Stress or anxiety.
Symptoms of Burning Mouth Syndrome
Constant or intermittent burning sensation, particularly on the tongue.
Dryness in the mouth, accompanied by excessive thirst.
Change or loss of taste.
Bitter or metallic taste in the mouth.
The symptoms may last throughout the day and may get worse as the day progresses. The burning sensation may also be insignificant on certain days or it may feel like a scalding burn on other days. The symptoms may come and go for days or months.
Preventing Burning Mouth Syndrome
Since the cause of BMS is not certain, little can be done to prevent it. However, if you are already suffering from the condition, home remedies and certain diet changes as described and may help you manage the symptoms.
Home Remedies to Treat Burning Mouth Syndrome
In conjunction with taking any medication prescribed by your physician, you can take certain self-help measures to control the symptoms. You may also be able to get rid of the condition completely by following the remedies religiously.
However, if treating secondary BMS, the underlying cause will play a significant role in deciding your road to recovery.
Here are the 8 home remedies to get rid of burning mouth syndrome. Give each a try and stick to the one that gives you the most relief.
Method 1: Baking Soda
Baking soda (aka sodium bicarbonate) is a readily available alkalizing agent that will regulate pH & help get rid of the acids in the mouth and relieve the burning.
Baking soda is used by health care practitioners alone or in combination with other treatments as a first line of defense against a number of health problems, including those that could be the culprit of BMS i.e., diabetes, kidney disease, cold, & flu.
You can also use baking soda occasionally to brush your teeth, instead of using regular toothpaste that may sometimes trigger burning mouth symptoms.
Add 1 teaspoon of baking soda to 1 cup of tepid water.
Mix it well and transfer the solution to a container for storage.
Use the solution as a mouth rinse 3 times daily to get rid of burning mouth syndrome in less than 1 week.
Method 2: Vitamin B12
If your body is deficient in vitamin B, especially vitamin B12, it can affect the tissues in the mouth, causing a burning sensation. Upping your intake of foods rich in vitamin B can help counter the symptoms.
You can also check with your physician about time-release vitamin B12 supplements. The time-release supplement will give your body a steady supply of the vitamin throughout the day to keep the symptoms in check.
Method 3: Sodium-Free Toothpaste
Changing your oral care habits can give you relief from the burning mouth. Many kinds of toothpaste contain sodium lauryl sulfate, the chemical that makes toothpaste foamy.
However, it can also irritate your oral cavity and lead to canker sores, bad breath as well as burning mouth syndrome.
Opt for sodium-free toothpaste to brush your teeth. You can also add in some baking soda that helps alkalinize the acids in your mouth and relieve the burning.
Mix toothpaste and baking soda in equal proportions in a bowl.
Use the blend to brush your teeth, instead of your regular toothpaste.
Use it daily whenever you brush your teeth. The symptoms should be gone within 1 week.
Continue to use sodium-free toothpaste without baking soda on a long-term basis to prevent future flare-ups. You can also use these recipes to make your own sodium-free toothpaste at home.
Method 4: Alpha-Lipoic Acid
Alpha-lipoic acid is a vitamin-like compound that works as an antioxidant, repairing nerve damage and preventing damage caused by free radicals.
In the case of burning mouth syndrome, it protects and heals the nerves in the mouth and eliminates the symptoms completely with regular consumption.
The recommended dosage is 600 mg per day to get rid of burning mouth syndrome.
Alternatively, you can divide the dose into 200 mg and take it 3 times daily.
Take alpha-lipoic acid supplements for 2 to 3 weeks to relieve the burning. You can continue to take it longer if needed to treat the condition completely.
You can also eat potatoes, spinach, liver, and broccoli, which are naturally rich in alpha-lipoic acid.
Method 5: Aloe Vera
Aloe vera is a natural coolant. It helps rehydrate as well as soothe sunburns and minor accidental burns.
In the case of burning mouth syndrome, the enzymes present in aloe vera form a protective coating on the delicate tissue in the oral cavity and speed up healing. Since it helps hydrate the tissue, it also gets rid of dry mouth and the related burning sensation.
Tips for relief
If you don’t have aloe vera gel, you can also apply glycerin or honey to keep your tongue moist.
Using salt water as a mouth rinse can also help reduce the burning.
Do not use an alcohol-based mouthwash, as it will worsen the burning.
(07/31/2024)by Fab How
More Information: https://www.fabhow.com/health-and-beauty/diseases-and-conditions/get-rid-of-burning-mouth-syndrome
Views: 390

Toothache Guide: How Serious Are They?
The treatment for a toothache may involve a somewhat invasive dental procedure such as a dental filling, root canal, dental bridge, dental crown or ultimately, a tooth extraction. But treatment today can be comfortable, and in fact, often helps you avoid tooth extraction. In addition, today’s cosmetic dentistry options, like dental veneers and dental implants, offer alternatives to traditional treatment, and provide a greater esthetic and functional benefit.
Toothache Types and What They May Mean
Evaluation and diagnosis by a dental professional can determine the type of toothache you are suffering from, and its source.
Sharp, Intermittent Tooth Sensitivity or Pain:Sensitivity to cold may denote gum recession, enamel loss from over-brushing or aging, wear and tear or a small dental cavity. Sensitivity to heat may also signify a small cavity, but it could be the result of an abscess, crack or severe decay.

Chronic Toothache: If one or more of your teeth is affected by chronic pain, nerve damage could be the cause. Nerve damage may result from teeth grinding, severe tooth decay or trauma to the teeth through injury.
Intense, Throbbing Pain: Intense, throbbing pain, sometimes accompanied by a swollen face, is often a sign of an infection or abscess.
Painful Eating: If it is painful for you to eat, the culprit could be tooth decay, or a slight fracture (crack) in a tooth.
Back-of-the-Jaw Pain: Pain in the back of the jaw may be associated with impacted wisdom teeth (back molars). But it could also be a sign of TMD or teeth grinding, both of which can cause jaw pain, and pain throughout other facial bone areas.

Toothaches range in severity, particularly in terms of tooth sensitivity and pain levels. An intermittent pain may seem little more than an occasional bother, while a chronic pain may prompt you to take immediate action.
Regardless of the type, your toothache should be evaluated by a dental professional through an oral health examination.
Causes and Solutions
Treatment for toothaches varies significantly depending on the severity of the pain and its cause. Options include:
Gum Recession: Gum recession can be reversed through a gum graft procedure whereby the gums are rejuvenated and maintained at their healthiest level. There are three approaches to the gum graft procedure:
The first approach involves removing tissue from the palate and grafting it to the root area.
The second approach involves an allograft (synthetic gum tissue) that is placed over a root.
The third approach is called a sliding graft whereby gum tissue is moved from adjacent areas over the root.
Tooth Sensitivity: Professional grade desensitizers are applied at the dental office, and require a reapplication every so often. Desensitizers can also be used during times of sensitivity at home. Finally, over-the-counter desensitizers such as those offered in select toothpastes may also provide relief.
Enamel Loss: An acidic diet, brushing too hard or natural wear and tear can result in enamel loss. When enamel is lost, the dentin (inner surface of the tooth) is exposed, causing sensitivity or pain. Desensitizers can help.
Wear and Tear: Enamel loss, uneven teeth, tiny chips and cracks can cause sensitivity or pain, and is usually indicative of tooth destruction. Uneven surfaces of the teeth may be filled with composite materials. Many cases involving wear and tear require tooth restoration with a crown or veneer.
Tooth Decay: Tooth decay is caused by an improper diet and poor dental hygiene. Depending on the amount of tooth decay you have, treatment may require a composite or amalgam filling, or, when accompanied by nerve damage or exposure of the root pulp, a root canal. When multiple tooth surfaces are affected, (making a dental filling an impractical solution) a dental crown or veneer is indicated.
Infection or Abscessed Tooth: An infection or abscess is the result of tooth decay or trauma. The treatment plan for an infection or abscess often begins with antibiotics and pain treatment, with a follow-up visit for root canal treatment. For the final restoration, the weakened tooth can be strengthened with a crown or veneer.
Crack or Fracture in Tooth: Cracks or fractures in teeth can occur from teeth grinding, trauma to the tooth or simply years of wear and tear. Usually, a cracked tooth is treated with a protective covering such as a dental crown or veneer.
Teeth Grinding: Teeth grinding can result in tooth fractures, unevenness and even a shift in the bite. Mouth guards used during sleep can help protect teeth from self-imposed injury caused by teeth grinding.
Impacted Wisdom Teeth: Impacted wisdom teeth are back molars that fail to surface. Impacted wisdom teeth can crowd and shift other teeth. Oftentimes, oral surgery is required to remove impacted wisdom teeth and relieve pain.
Is Your Toothache Indicative of a More Serious Problem?
Because some toothaches signify more serious health issues, you should not ignore them. For instance, studies have demonstrated that heart attacks may be signaled by the sensation of pain on the left side of the jaw. Soreness in the jaw and cheekbones or difficulty in chewing may also be the first sign of temporomandibular joint disorder (TMJ), a serious maxillofacial condition. In addition, sinus infections may produce pain in the upper molar teeth, wrongly leading you to believe that your pain is the result of a dental problem. It is for these reasons that you should consult your dentist if you have a chronic or extremely painful toothache.
The good news is that dentists now have more advanced methods for identifying the sources of toothache pain, and have developed more comforting and effective solutions to preserve teeth.
First Aid Relief for Toothache
Until you are able to reach the dental office, there are a few ways to find relief from dental pain.
Your dentist may advise you to take ibuprofen, acetaminophen or aspirin to dull the pain. Over-the-counter medications containing benzocaine may reduce pain in the affected tooth, or surrounding gum area. However, aspirin applied directly to the tooth is not recommended, because it can burn the gums or cheek.
To reduce discomfort from swelling, you may be advised to swish warm saltwater in your mouth periodically throughout the day, and apply an ice pack to the swollen area.
(07/29/2024)
by Consumer Guide To Dentistry
More Information: https://www.yourdentistryguide.com/toothaches/
Views: 458

Recognizing The Signs Of Infection After Root Canal Treatment
By being able to recognize these signs of infection after root canal, patients can prevent the infection from spreading further or causing complications.
What are root canal infections?
A root canal infection is a dental condition that occurs when bacteria invade the soft tissue inside a tooth known as the pulp. The pulp contains blood vessels, nerves, and connective tissues that help the tooth grow during development.
When the pulp becomes infected or inflamed, it can cause severe pain and discomfort and may lead to the development of an abscess, a pocket of pus that forms around the tooth. A root canal procedure is typically necessary to treat a root canal infection.

During this procedure, the dentist or endodontist removes the infected pulp from the tooth and fills the space with a rubber-like material called gutta-percha. A dental crown may also be placed over the tooth to protect it from further damage. This article highlights the importance of being able to identify the signs of an infection after undergoing root canal treatment, to help prevent complications.
What causes root canal infections?
Root canal infections can occur due to a variety of reasons. There are many reasons why a tooth can have an infection after a root canal. These include:
Complex root canal anatomy: The shape of your root canals can be very complicated and areas of infection may go undetected in the first procedure.

Incomplete cleaning and disinfection: Your tooth could have narrow or curved canals that weren’t fully cleaned and disinfected during the root canal.
Accessory canals: Your tooth may also have extra, accessory canals that could be housing bacteria which may reinfect a tooth.
Delayed placement of restoration: If the placement of the crown or permanent restoration is delayed following treatment, it could allow harmful bacteria back into your tooth.
New cavity or damage: Your tooth may get a new cavity after treatment, or become cracked or damaged, leading to a new root canal infection.
It’s important to address these issues promptly to avoid the need for additional root canal procedures or even tooth extraction.
Signs You May Have An Infection After A Root Canal
Some of the signs that you may have an infection after a root canal procedure include persistent or reoccurring pimples on the gums, persistent feeling of lethargy, the area of the tooth and gums feeling hot, and fever, constant pain. If you experience any of these symptoms, it’s essential to contact your dentist or endodontist right away.
Persistent or Reoccurring Pimples on the Gums
If you notice a pimple or bump on your gums that persists or continues to reappear, it may be a sign of an infection. This can occur when pus from the infected area is trying to drain out.
Persistent Feelings of Lethargy
An infection can cause you to feel tired or run down, even if you haven’t been exerting yourself. This is because your body is using energy to fight off the infection.
The area around the Tooth and Gums Feels Hot
In some cases, you may notice that the area around the affected tooth and gums feels warm or hot to the touch. This can be a sign that the infection is spreading and causing inflammation.
Fever
Fever after root canal can indicate that an infection has spread beyond the affected tooth and gums and into other parts of your body. A fever is usually defined as a temperature of 100.4°F (38°C) or higher.
Persistent Pain
If you continue to experience pain or discomfort in the affected area, even after the root canal procedure, it may be a sign that the infection has not been fully treated. This can be a sign that the infection is spreading and causing inflammation in the surrounding tissues.
Can an infection spread to the gums or to other teeth?
An infection after a root canal can spread to the gums and other teeth. When an infection is not properly treated, bacteria can spread to the surrounding gums and tissues, causing inflammation and infection. This can lead to symptoms such as redness, swelling, and tenderness in the gums. In severe cases, the infection can even spread to other teeth, causing new infections.
Additionally, an untreated infection can also spread to other parts of the body, including the jawbone, sinuses, and bloodstream. This can cause serious health complications, such as abscesses, bone loss, and even sepsis. Therefore, it’s important to seek prompt treatment for any signs of infection after a root canal.
How are root canal infections treated?
When it comes to root canal infection treatment, a root canal retreatment may be recommended by a dentist or endodontist to give the affected tooth a second chance. This procedure is similar to the first root canal therapy and involves several steps to effectively remove the infection.
The dentist or root canal specialist will examine the tooth and surrounding area using X-rays to locate any infected or necrotic tissue. A protective barrier will be placed around the tooth to protect the gums and mouth. The dentist will use a dental drill to access the pulp and root canal area and clean out the infected or dead tissue.
After cleaning the area, the dentist will dry it out and fill it with a safe, latex-based polymer filler called gutta-percha. To protect the tooth and allow it to heal from infection, filling material such as amalgam or composite will be used to seal the tooth. A permanent crown may be necessary to protect the tooth from future infections.
Overall, root canal retreatment effectively treats a root canal infection and saves the affected tooth. Your dentist or endodontist can discuss the best treatment options for your situation.
Make Your Appointment With Dentist For Life Today!
Making an appointment with a trusted and experienced dentist is important for maintaining good oral health, preventing and treating an infection after a root canal, and addressing any concerns you may have about your teeth and gums. At a dentist in Marysville Ohio, we are committed to providing high-quality dental care to our patients.
Our team of skilled dentists and staff use the latest technology and techniques to ensure your comfort and satisfaction. Contact Dentist for Life today to schedule an appointment and start your journey to a healthier, happier smile.
(07/29/2024)by Dentist For Life
More Information: https://dentistforlife.net/blog/signs-of-infection-after-root-canal
Views: 459

Tooth Abscesses vs Tooth Infections: What is the Difference?
When teeth are healthy, strong and free from infection, they feel so comfortable that you are not aware of them. It is a very different story when a tooth becomes infected, and the pain of a tooth infection can be considerable. A dental abscess can feel even worse, but we find patients are frequently confused by the differences between these conditions.
What is a Tooth Infection?
Your mouth is home to hundreds of species of bacteria, many of which are benign, but some are harmful and can cause infection. Usually, your teeth have a hard outer coating of enamel that protects them and prevents bacteria from entering the tooth. You can have an infected tooth if you have a very deep cavity that isn’t treated, have gum disease (periodontal disease) or if a tooth is cracked. When a tooth is cracked, it lets in harmful bacteria. Even a small crack in a tooth can open up every time you bite down.
If tooth enamel is damaged through trauma or decay, these harmful bacteria can penetrate the tooth, soon reaching the tooth pulp. Your tooth pulp is right in the centre and contains the tooth nerve, connective tissues and blood vessels and extends into the tooth roots via root canals. When it becomes infected, it is extremely painful. The tooth nerve can also become damaged and inflamed if you take a blow to the mouth.
What are the Signs and Symptoms of a Tooth Infection?
Tooth infection symptoms usually include:
Throbbing pain in the affected tooth
Pain when you try to bite or chew on the tooth
Increased sensitivity to hot and cold foods and drinks

Sometimes a tooth will initially feel painful, but the discomfort might disappear. This doesn’t mean the infection is gone. It could mean the tooth nerve has died, so the tooth no longer feels painful, but the infection is still present. A tooth infection will not clear up on its own; your immune system cannot fight the infection as it can’t send antibodies to the inner part of the tooth. Instead, the infection will continue to spread beyond the tooth and the tooth root. It can start to affect the area between the tooth and your jawbone and turn into a tooth abscess.
What is a Tooth Abscess?
You have a tooth abscess if an untreated tooth infection spreads beyond your tooth root, and there are two main types of dental abscesses. Periapical abscesses are formed right at the tip of a tooth root. Periodontal abscesses form in the bone right next to the affected tooth and may be present if you have gum disease. If you have advanced gum disease, your gums can pull away from your teeth, creating deep pockets, called periodontal pockets, where bacteria can thrive, eventually causing an abscess.
What are the Signs and Symptoms of a Tooth Abscess?
An abscessed tooth can cause pain, but this isn’t always the case. Other symptoms include:
Swollen gums around the affected tooth
Pain when chewing
A persistent bad taste
Bad breath
Jaw pain
A severely abscessed tooth can cause a pimple to form on the gum, that if you press it will ooze pus. A dental abscess can affect overall health, as the bacteria can spread to other parts of the body. Signs to be aware of include swollen lymph nodes, facial swelling, fever and a general sense of feeling unwell. A tooth abscess may also cause trouble breathing or swallowing and a headache.
If you are concerned you have a dental abscess and think the infection has spread, you must seek emergency medical care. In rare cases, a severe tooth infection can spread to the brain and may become life-threatening.
Although similar conditions cause tooth infections and dental abscesses, treatment isn’t always the same. If you do have a painful tooth, contact Tandara Dental Centre as soon as possible. Dental pain isn’t normal and indicates a problem with a tooth that needs professional care. The sooner we can see you, the greater the chance we can successfully treat a tooth infection and save the tooth. It is much harder to save abscessed teeth.
What About Using Home Remedies for a Tooth Infection?
We know it is easy to look online and discover all sorts of remedies for tooth infections. However, home remedies for a tooth infection will not eliminate the bacteria causing this problem. You will need professional dental care. The sooner you see a dentist, the more quickly we can get rid of discomfort and pain and prevent the infection from spreading.
Diagnosing a Tooth Infection
When you visit Tandara Dental Centre, we can gently examine the tooth and quickly diagnose the reason for tooth pain. Our dentist will most likely take a dental x-ray of the tooth, showing the extent of the infection. Once we have this information, we can decide the best way to treat the infection and hopefully save the tooth.
Treating a Tooth Infection
If the infection has not spread into the surrounding tissue and is confined to the central part of the tooth, our dentist may recommend root canal treatment.
What is Root Canal Treatment?
Also called endodontic treatment, root canal treatment removes the infected dental pulp and the tissues extending into the root canals in the tooth roots. It is an intricate process that takes several visits to complete. Your tooth will feel much more comfortable after your initial visit to get rid of the infected tissues in the tooth, but it could still feel a bit sensitive for a while until it settles down.
Once all the infected tissue is removed, the tooth is disinfected, and medication is placed in the tooth to eliminate any remaining bacteria. We will insert a temporary filling to allow the medication to work. After several weeks, our dentist will remove the temporary filling, clean the tooth again and insert more medication and another temporary filling. The tooth is left to settle down for another few weeks to make sure it is infection-free. The next stage is to seal the tooth permanently with a material called gutta-percha. Sometimes a post is inserted into the tooth for additional strength.
Because a severely infected tooth has almost certainly lost a substantial part of its structure, it is restored with a dental crown. The crown fits over the entire tooth, sealing and protecting it from further infection. The crown restores appearance and strength, so you will be able to eat and talk comfortably and confidently. Your root treated tooth is now ‘non-vital’ as the nerve is removed and, consequently, more brittle but could last for years or life.
Sometimes a tooth that has received root canal treatment can become re-infected. At this stage, we would need to assess the tooth very carefully. It might be possible to perform a second root canal treatment to remove the infection, but we will need to discuss the possible risks and benefits of this approach. Treatment could be quite involved and costly and may have a limited chance of success. If this is the case, we might suggest removing the tooth and looking at suitable ways to replace it, such as placing a dental implant that can provide a long-term solution.
Diagnosing a Tooth Abscess
If we discover your tooth infection has spread beyond the tooth and that you have a tooth abscess, we will still try very hard to save the tooth. When we take the x-ray of your tooth, we can see if the abscess is treatable and any chance of saving the tooth. It depends on how far the infection has spread beyond the tooth.
Treating a Tooth Abscess
You will almost certainly need antibiotics, and the abscess or pocket of pus on the gums might need to be lanced so it can be drained. When we can catch a tooth abscess soon enough, root canal treatment could save it. Unfortunately, if the infection is severe, the only solution may be to remove the tooth to help the infection drain adequately. Leaving the tooth in place could cause additional oral health problems, especially as the infection will have killed the tooth nerve, and there will be no blood flow to the tooth root to help fight the infection.
What About Wisdom Tooth Infections?
Your wisdom teeth usually come through during the late teens and early twenties and can cause problems if they cannot erupt properly and become impacted or stuck underneath the adjacent teeth. Often there is inadequate room for wisdom teeth, so they can cause problems with overcrowding, affecting the adjacent teeth. Some wisdom teeth will partially erupt, so they are tricky to keep clean and become decayed and infected more easily. An impacted and infected wisdom tooth can cause toothache and jaw pain and must be removed.
If your wisdom teeth have yet to make an appearance, we will monitor them closely, checking their position in your jaw using digital dental x-rays. We prefer to take a wait and see approach, but if it is obvious these teeth cannot erupt without causing problems, we will suggest removing them before you get a wisdom tooth infection due to an impacted tooth.
What to Expect if You Need a Tooth Removed?
Tooth extraction is usually a routine procedure, and if you do need this treatment, we will do everything we can to ensure you feel comfortable. If you need a straightforward tooth extraction, local anaesthetic is usually enough to numb the tooth so we can quickly remove it. You should not feel any pain as the tooth is taken out.
If tooth removal is more complicated, it may require a surgical extraction, for example, if a wisdom tooth is partially or completely hidden in the gum. In this case, we can provide additional sedation if needed, so you feel deeply relaxed or will fall asleep during treatment. The tooth is then removed by making a small opening in the gum and jawbone to expose it. The tooth might be sectioned or cut into smaller pieces before we remove it, so we only need to make a small incision that will heal more quickly and comfortably.
What to Expect After Tooth Extraction?
Healing after tooth extraction should be uneventful and comfortable, and we will provide lots of information on how to care for the surgery site. An infection after tooth extraction only occurs in a tiny percentage of cases. When it does happen, it is very treatable. It could be a condition called dry socket, where the blood clot protecting an empty tooth socket becomes dislodged, allowing the socket to become infected and increasingly painful. In this case, we can clean out the socket so it can heal more easily.
Can I Prevent a Tooth Infection and Tooth Abscess?
Practising good oral hygiene can reduce the risk of developing a tooth infection and gum disease. We much prefer this preventive approach rather than seeing patients in pain or discomfort that could have been avoided.
Preventive Dentistry
Preventive dentistry is not complicated or time-consuming and could save you from pain and avoid spending hours in our dental chair. It is also much more cost-effective.
Regular Professional Dental Care
When you visit a dentist for regular checkups and cleanings, any signs of problems, such as gum disease or small lesions in teeth, are detected and easily treated before they can develop into larger and more troublesome issues. When we can catch dental problems in their early stages, the risk of developing tooth infections and tooth abscesses declines.
Professionally cleaning your teeth removes all the plaque and tartar buildup from teeth, reducing tooth decay and gum disease risks. Dental education is another important factor. When we clean your teeth, we can easily identify areas that need a bit more attention when you brush and floss. Our dental team can discuss how to clean your teeth more effectively and, if needed, can demonstrate different techniques and tools to use.
Taking Care of Your Oral Health at Home
A good oral hygiene routine takes less than ten minutes each day and will help you enjoy optimal oral health between checkups. The routine is extremely straightforward, simply involving brushing your teeth twice a day for two minutes each time. You need the full two minutes to clean all tooth surfaces thoroughly. If you use an electric toothbrush, it will have a built-in timer, but if you prefer a manual brush, be sure to set the timer on your phone or keep a small timer in the bathroom for this purpose. It is very easy to underestimate two minutes! You must floss your teeth once a day because plaque bacteria and food debris can easily become trapped between your teeth, greatly increasing the risk of a tooth infection or gum disease. Flossing is easy once you know how to do it correctly, so be sure to ask us for help if you struggle with this task. We can show you some techniques or other tools to try.
Tooth infections and tooth abscesses are unpleasant and can cause tooth loss but are often preventable with the proper dental care. By working together, we can help you achieve and maintain your best level of oral health.
(07/30/2024)by Tandara Dental Centre
More Information: https://www.tandaradental.com.au/tooth-abscesses-vs-tooth-infections-what-is-the-difference/
Views: 444

Common Problems In The Mouth That Adults Experience
Throughout your adult life, you will most likely suffer from at least one of the common problems in the mouth that we’re about to list. We’re not saying that it’s inevitable these will happen, but rather reporting on what has already happened to many adults – all of which require the expertise of your dentist to correct.
Chipped Teeth
You would believe that chipped teeth would be something akin to children who love to roughhouse and get into things they shouldn’t, but surprisingly chipping a tooth is a phenomenon that occurs most often in adults. Our chances of chipped teeth become greater with age. With age, we chew on more ice, more hard candies, etc. Also, our enamel isn’t as strong with age – despite being the strongest mineral in our bodies. If you chip a tooth, salvage the missing piece if you can, and bring it with you to an emergency dentistry appointment.
Stained Teeth

Over time, we expose ourselves more and more to common foods and drinks that are known to cause stains on our teeth such as wine, coffee, tea, soda, dark berries, spaghetti sauces, etc. No matter how many store bought teeth whitening trays your purchase, or whitening strips, the result will not be as fast and effective as teeth whitening performed by a professional dentist.
Amalgam Tattoo
While the American Dental Association has deemed amalgam as a safe solution for dental fillings, there are potential problems associated with them such as “amalgam tattoos”.You’ll notice these on the inside of your cheeks appearing as blue-grayish spots. They occur when a small piece of amalgam finds its way into the soft tissue of your mouth. They’re harmless, but you should consult your dentist on removing your amalgam fillings and replacing them with more advanced options.

Gum Disease – Experienced by Many Adults
Gum disease is the one of the main reasons dentists constantly nag you to brush and floss your teeth. When you don’t – you begin to enter the world of gum disease, which can be reversed in it’s early stages (known as gingivitis), but is non-reversible if it gets out of control. Many young adults are recommended to undergo deep cleaning procedures because they were not staying consistent with their routine. Listen to your dentist: brush and floss!
Many other common problems exist within our mouths as adults, but these seem to bear the most weight. Always make sure to visit your dentist every six months, not just for a routine cleaning, but for a chance to have a professional examine your mouth for any abnormalities. Dental exams are more important than you may realize.
(07/31/2024)by Sohrab Rahbar, DDS
More Information: https://www.dentistinirvine.com/blog/problems-in-the-mouth/
Views: 483

