My BEST Dentists Journal
Articles tagged #American Dental Association
Today's Dentists Journal

Possible Causes of Tooth Pain After Brushing
Have you noticed discomfort or pain after brushing your teeth? Picking up on warning signs of oral health issues and quickly acting on them is a great way to keep your teeth and gums in excellent condition. Read on for the top three causes of tooth pain and what to do about them.
Tooth Sensitivity
Cleaning your teeth is essential for keeping your smile healthy. If your teeth hurt after brushing or eating hot or cold foods, you may have tooth sensitivity. According to the American Dental Association, tooth decay and gum disease can cause tooth sensitivity, and you will need professional treatment. Your dental professionals can check for signs of oral health problems and recommend a treatment for tooth sensitivity, such as a special toothpaste, a crown, or an in-office application of fluoride gel.
Tooth sensitivity may be temporary. Some people report tooth pain shortly after a visit to their dental hygienist, if the dental hygienist has done any scaling or tartar removal. Your teeth could also be sensitive if you have gum recession, as the exposed root surface may cause discomfort. In this case, tooth sensitivity is likely only temporary, so you can simply brush your teeth with sensitive toothpaste. Usually, your teeth will return to normal within a few weeks. If they do not, call your dentist and ask them to check your teeth.

If a recent dental treatment is not to blame, food sensitivity can often be a side effect of damaged enamel, which you can't get back once worn away. Damaged enamel occurs when the hard mineral that protects your teeth's surface erodes over time, as explained by the United States National Institute of Dental and Craniofacial Research (NIDCR). Enamel erosion is usually the result of exposure to acid or excess sugar. Enamel that wears away can result in cavities and pain after brushing or flossing. If you suspect this is the reason for your teeth hurting after flossing or brushing, talk to your dentist.
If the enamel wears away to the point of exposing the sensitive nerves in your teeth, you have a cavity. These cavities often manifest as sharp pain when you bite down on something hard, and it doesn't have to be hot or cold to set you off. Cavities are small fissures in your teeth, but they can lead to more complicated problems if left unfilled. You should see your dentist as soon as you suspect you have one; he or she can fill it to prevent the condition from worsening.
Gum Problems and Cavities
Gum problems precede gum disease. Plaque build-up irritates gum tissue, making gums swollen and tender. Maintain proper oral hygiene and see your dentist if you notice these symptoms. As gum problems progress, they can become more challenging to treat.

The Wrong Toothbrush
If you notice pain and discomfort after brushing with a hard-bristled brush, it may be time to get a new toothbrush. Most dentists recommend a soft-bristled toothbrush to keep teeth clean. Good brushing technique with a soft brush can help remove plaque and help fight tooth cavities and gum problems without irritating your gums and teeth. Brush for two minutes using short, gentle strokes. Clean all the surfaces of your teeth, including the outside, inside, and chewing surface of those hard-to-reach back teeth.
As you can see, tooth pain after brushing may be a temporary inconvenience after a professional dental treatment, or it may be a sign of a more serious oral health condition. Maintain good oral hygiene habits with a soft-bristled toothbrush. Be sure to see your dentist if you notice pain, discomfort, or sensitive gums.
(12/30/2024)by Colgate
More Information: N
Views: 602
Should You Use Mouthwash Before or After Brushing?
Brushing and flossing are the foundations of a good oral hygiene routine‚ but mouthwash can also be a useful addition, thanks to the many oral health benefits it has to offer. If you've recently started using mouthwash, you may be wondering how you should incorporate it into your routine. Is it better to use mouthwash before or after brushing? And what else can you do to boost your oral health?
Benefits of Mouthwash
Mouthwash is probably best known for freshening your breath, but adding it to your daily oral care routine can provide many other benefits, too.
The South African Dental Association (SADA) recommends that you protect your mouth while on the go and after meals and snacks by rinsing with a fluoride mouthwash; this will freshen your breath and help guard against cavities. As the American Academy of Periodontology notes, untreated gum disease can lead to complications such as gum recession and tooth loss, but using mouthwash can help boost your prevention efforts.

Mouthwash achieves these oral health benefits by helping to control plaque, which is a thin film of germs that builds up on your teeth. When plaque isn't removed, it eventually hardens into tartar. The American Dental Association (ADA) reports that mouthwash can actually slow down the formation of tartar, too.
When to Use Mouthwash
When you first add mouthwash to your oral care routine, you may wonder: Should you use mouthwash before or after brushing? This is a good question, and it doesn't have a simple answer. The scientific research is limited, and reputable organisations offer different recommendations.
The US-based Mayo Clinic recommends using mouthwash after brushing and flossing your teeth. However, the National Health Service (NHS) in the United Kingdom recommends avoiding mouthwash right after brushing, since this may wash away the fluoride from your toothpaste. Instead, the NHS recommends using mouthwash at a different time of day.

The ADA states that you can use mouthwash either before or after brushing, depending on your personal preference. That said, mouthwash manufacturers may recommend an order based on their product's ingredients, so check the label on your product to ensure that you maximise its effects.
Other Ways to Boost Your Oral Care Routine
Mouthwash may enhance your oral care routine, but remember: it's not a substitute for regular brushing and flossing. Brush your teeth twice a day for at least two minutes to remove food particles and plaque from your teeth, and floss once a day to clean between your teeth and along your gumline.
If you want to make further improvements to your daily oral care routine, consider these tips from the South African Dental Association (SADA):
Eat a well-balanced, tooth-healthy diet
Limit high-sugar foods and drinks, such as sweets and fizzy drinks
Avoid frequent snacking
Apply toothpaste to the full length of your toothbrush head
See your dentist regularly for check-ups.
While it's not a replacement for brushing and flossing, mouthwash can play an important role in your oral hygiene routine. It can help to freshen your breath, remove plaque and reduce your risk of cavities and gum problems. For help deciding whether to use mouthwash before or after brushing, talk to your dentist.
(12/28/2024)by Colgate
More Information: https://www.colgate.com/en-za/oral-health/brushing-and-flossing/should-you-use-mouthwash-before-or-after-brushing
Views: 627
How Long Should I Brush My Teeth?
The importance of brushing for the full two minutes is an oft-repeated piece of advice that dentists give to patients, and parents give to children. But is there science to back this up? Why two minutes and not one or four? How long should you brush your teeth to maintain good oral health? The fact is, brushing your teeth correctly and thoroughly is essential for healthy teeth and gums, but it takes time ― at least two minutes.
What the Experts Say
Experts who advise on how long you should brush your teeth usually recommend a minimum of two minutes, twice daily. A study published in the British Dental Journal examined 66 sources of dental information from around the world and found that a significant portion of them (26) advised brushing for two minutes. The remaining sources offered a number of different recommendations, all longer than two minutes, with some recommending brushing for more than three minutes. The American Dental Association backs the two-minute rule, and runs a campaign called 2min2x to help parents get the message across to children.
What the Science Says

Research supports the recommendation to brush for at least two minutes. It seems obvious that the longer you brush your teeth, the more plaque you remove, and now a study published in The Journal of Dental Hygiene backs this up. The study analyzed the effect of brushing time on plaque removal across a range of time periods, from 30 seconds to three minutes. The researchers found that patients who brushed for 45 seconds removed 26 percent less plaque than patients who brushed for two minutes. The difference in plaque removal when comparing shorter and longer brushing times was even wider: according to the study, brushing for 30 seconds removes 55 percent less plaque than brushing for three minutes.
Why Brushing Your Teeth Takes Two Minutes
Two minutes may feel like an awfully long time when brushing your teeth, but only if you are not doing it thoroughly. Removing food debris, plaque and bacteria from the surface of your teeth is only one step in an effective, twice-daily oral-care routine.

As well as setting up home on your teeth, bacteria also coat your mouth's interior, including the inside of your cheeks, your gums and your tongue. To reduce your risk of bad breath and cavities, you should brush these areas too. Once per day, you'll need to spend just a little longer cleaning your teeth via flossing, because that's also a critical step toward good oral health.
How long should you brush your teeth? As long as it takes to do a good job. For some people, two minutes is long enough, for others, it may take longer. For that clean mouth feeling and the confidence that you are helping prevent tooth decay, the time spent is worth it.
(12/19/2024)by Colgate
More Information: https://www.unitedconcordia.com/business-services/employers/blog/long-brush-teeth
Views: 619
Is UV Teeth Whitening Safe?
Everyone deserves to have a beautiful, confident, and healthy smile, so it’s no wonder that there are so many at-home products on the market that help you combat yellow or stained teeth to achieve a brilliant sparkle. But there’s one teeth whitening product that’s gained attention in the past decade among celebrities and social media influencers that’s a bit more high-tech and a bit more expensive: an at-home UV teeth whitening kit. Here, we’ve laid out a few facts on the safety and effectiveness of these types of products, so you can understand how it works before considering it as an option for a whiter smile.
How It Works
These kits are similar to a common in-office teeth whitening treatment, which involves a dental professional applying a peroxide-based whitening gel to your teeth, and placing a blue UV light over the teeth. Together, the gel and light create a system that can expedite the teeth whitening process. And these in-office treatments are effective—according to a study published in the Journal of Conservative Dentistry, light-activated bleaching showed an increase in lightness compared to bleaching done without light. Further, the light-activated process lasted longer.
An at-home kit functions similarly and typically instructs you to apply a whitening gel to your teeth with a pen and then use a portable LED light over your teeth for a few minutes over a period of days. These kits often come with a higher price tag than other at-home whitening solutions, like whitening toothpaste or strips.

Safety of UV Teeth Whitening Kits
You might be wondering: is UV teeth whitening safe? While the American Dental Association does mention that in-office light-activated treatments are an option you could consider for teeth whitening, they do not mention at-home UV light kits as a recommended option. The ADA also notes that tooth sensitivity may be associated with this process when done at the dentist’s office.
Another critical safety consideration: there are no regulations associated with at-home UV light teeth whitening kits. A 2019 article in the Journal of the American Dental Association states that the Centers for Disease Control and Prevention Guidelines for Infection Control “do not include safety recommendations or regulations that are directly related to blue light exposure.”The article also concludes that evidence suggests you should take precautions when using dental curing kits. Further, according to the Oral Health Foundation, regulations on these kits vary from country to country. For instance, kits in Europe cannot legally contain more than 0.1% peroxide, whereas other countries allow for stronger amounts. Plus, some kits sold over the internet may contain extra ingredients that could be potentially harmful.
Another potential issue in using UV teeth whitening is that there can be extreme user error, resulting in damage and even burns. The ratio of gel to UV exposure varies from kit to kit, and without the consultation of a dentist, you may not know your threshold for sensitivity. What's more, applying too much gel at one time can result in the gel conducting too much of the heat from the UV light, causing gum burns.

So, to answer the question initially stated about safety, it’s unclear. Therefore you should avoid using UV light kits at home, as the research isn’t definitive enough to say that it’s safe. Plus, the ADA has not approved this kind of therapy.
What if I injured myself with an at-home UV whitening kit?
If you’ve experienced any injury from a UV whitening kit, don’t panic—your oral health care provider will know what to do. If you’re injured, contact your oral health care provider immediately, and have the kit on hand to provide any information. From there, they will be able to help determine the best treatment. Luckily, there are plenty of other safe and effective home whitening methods available—and they don’t break the bank either!
Teeth Whitening Alternatives
If you want to whiten at home, you’ve got options. One is to choose a toothpaste that contains a whitening ingredient, like hydrogen peroxide. You can use a whitening toothpaste every day for continuous whitening that becomes part of your oral care routine—no extra steps required. Whitening strips and pens are other options, though you should consult with your oral care professional to ensure that this is the safest method for your needs. While these methods won’t be as quick as an in-office treatment, you can take comfort in knowing that they’re safe. But before you go ahead and choose an at-home whitening option, talk to your oral care provider first, and together you can determine the best (and safest) method.
The next time you notice an advertisement or celebrity endorsement for a teeth whitening UV light kit, remember to take it with a grain of salt. With the right at-home treatment or even a treatment via your oral care provider, you can get the star power smile without the risk.
(12/12/2024)by Colgate
More Information: https://www.colgate.com/en-in/oral-health/teeth-whitening/is-uv-teeth-whitening-safe
Views: 567
Six Ways to Keep Your Gums Healthy
Having cavity-free teeth doesn’t mean you have healthy gums. Since it’s usually painless, you may not know if something is wrong with your gums. A few strategies can help you keep your whole mouth healthy.
When it comes to your mouth’s health, it’s not all about how straight your teeth are or how bright your smile is. You can’t forget about your gums!
What is gum disease?
Gum disease starts when plaque builds up under and along the gum line. Plaque is a sticky film-like substance that’s filled with bacteria. It can cause infections that hurt the gum and bone, leading to gum disease and tooth decay. Plaque also can cause gingivitis, the earliest stage of gum disease. Gingivitis causes your gums to become:
inflamed
tender
red
swollen
prone to bleeding
Fortunately, since the bone and tissue holding the teeth in place aren’t impacted, this damage is reversibleTrusted Source.

You can also develop periodontitis, an advanced form of gum disease. Periodontitis impacts the bones that hold your teeth in place. Left untreated, it can ruin the gums, bones, and tissues connected to your teeth.
The final stage of gum disease is advanced periodontitis. This is when the fibers and bone supporting your teeth are destroyed. It can impact your bite, and teeth may need to be removed.
According to the American Dental Association (ADA), signs that you might have gum disease include:
consistently bad taste or breath
separating or loose permanent teeth
gums that easily bleed
gums that are swollen, red, or tender
gums that have pulled away from your teeth
Gum disease is preventable. Here are a few ways you can help keep your gums healthy.
1. Floss
Floss at least once a day. This helps remove the plaque and food that’s beyond your toothbrush’s reach, according to the ADA. It doesn’t matter when you floss. Do it at night, do it in the morning, or do it after lunch… just do it!
2. Get regular dental cleanings
Your dentist can detect early gum disease symptoms if you see them on a regular basis. That way symptoms can be treated before they become more serious. A professional cleaning is the only way to remove tartar. It can also get rid of any plaque you missed when brushing or flossing. If you have gingivitis, brushing, flossing, and regular dental cleanings can help reverse it.
3. Quit smoking
Yet another reason for smokers to quit: Smoking is strongly associated with the onset of gum disease. Since smoking weakens your immune system, it also makes it harder to fight off a gum infection, say the Centers for Disease Control and Prevention (CDC)Trusted Source. Plus, smoking makes it more difficult for your gums to heal once they’ve been damaged.
4. Brush twice a day
Brush your teeth after every meal. This helps remove the food and plaque trapped between your teeth and gums. Scrub your tongue too, since it can harbor bacteria. Your toothbrush should have soft bristles and fit in your mouth comfortably, says the Mayo Clinic.
Consider a battery-powered or electric toothbrush. These can help reduce gingivitis and plaque more than manual brushing. Swap toothbrushes or toothbrush heads every three to four months, or sooner if the bristles start to fray.
Try an electric toothbrush today.
5. Use fluoride toothpaste
As for toothpaste, store shelves are lined with brands that claim to reduce gingivitis, freshen breath, and whiten teeth. How do you know which one is best for healthy gums? Make sure to choose toothpaste that contains fluoride and has the ADA seal of acceptance. After that, the flavor and color is up to you!
You can purchase toothpaste that contains fluoride online.
6. Use a therapeutic mouthwash
Usually available over the counter, therapeutic mouthwashes can help reduce plaque, prevent or reduce gingivitis, reduce the speed that tarter develops, or a combination of these benefits, according to the ADA. Plus: A rinse helps remove food particles and debris from your mouth, though it’s not a substitute for flossing or brushing. Look for the ADA seal, which means it’s been deemed effective and safe.
It doesn’t matter whether your brush, floss, or rinse first. Just do a good job and use the right products.
(12/11/2024)by Healthline
More Information: https://www.healthline.com/health/dental-and-oral-health/ways-to-keep-gums-healthy?utm_source=ReadNext
Views: 535
Do Cavities Cause Bad Breath?
Most people wake up in the morning with less than kissable breath. But when bad breath, also known as halitosis, interferes with your confidence and social life, it's time to figure out what's causing it. Do cavities cause bad breath? And is your oral care routine strong enough to keep bad breath away? Here's what may be causing your bad breath and how you can remedy it.
What Causes Bad Breath?
Bad breath results from an accumulation of germs in the mouth. According to a review in the Journal of Pharmacy and BioAllied Sciences (JPBS, the official publication of the Organization of Pharmaceutical Unity with BioAllied Sciences registered in India), when certain germs in the mouth interact with proteins in the saliva, this creates volatile sulfur compounds. The sulfur compounds are what we smell when we realise it's time to grab a mint. According to the JPBS review, bad breath can be caused by:
Poor oral hygiene that allows food debris to get trapped in the mouth

Gum problems and periodontitis
Germs on the tongue
Ear, nose and throat problems, including tonsillitis and sinusitis
Dry mouth

Personal habits, such as smoking and drinking alcohol.
Do Cavities Cause Bad Breath?
Cavities are small holes in the teeth where germs collect and eat away at the enamel. While cavities do not directly cause bad breath, they can contribute to it. Germs can get stuck and accumulate in the decay pockets, making it more difficult to keep your mouth clean and your breath fresh, explains the American Dental Association (ADA).
Bad breath does not necessarily signal a cavity, but it could indicate that you have one. That's why it's important to maintain regular dental appointments and see your dentist right away if you suspect that you have a cavity or if you are experiencing tooth sensitivity or pain.
Manage Bad Breath and Cavities Like a Pro
One of the easiest ways to manage and prevent both bad breath and cavities is to practise good oral hygiene. Start with brushing twice a day. Brushing your teeth physically removes decay-causing germs and food particles. You should also floss daily to remove lingering germs and food particles hiding in between your teeth.
Keeping your mouth moist is important for fresh breath, too. A healthy saliva flow is one of the best defenses against bad breath, as it washes out the mouth, notes the ADA. Be sure to drink plenty of water and talk to your doctor about any possible contributing factors for dry mouth, such as taking certain medications.
Smoking is another contributor to bad breath, and it can also increase your risk for gum problems, explains the ADA. Ask your doctor for strategies to help you quit.
If you wear dentures or another oral appliance, the US-based Mayo Clinic suggests cleaning them daily to prevent bad breath. Follow your dentist's specific directions for cleaning your appliance.
Finally, seeing your dentist regularly ensures that your mouth stays healthy. A professional teeth cleaning can remove germs and food that your toothbrush at home may miss. Your dental professional will also check for cavities that could harbour bad germs. If they do detect any cavities, they can fill them to stop the condition from worsening.
Bad breath can be a real bummer. While cavities do not directly cause bad breath, you can prevent both bad breath and cavities by practising good oral hygiene and seeing your dentist regularly.
(12/10/2024)by Colgate
More Information: https://www.colgate.com/en-za/oral-health/bad-breath/do-cavities-cause-bad-breath
Views: 544
Who Knew Brushing Your Teeth Could Be Life Saving?
Our parents, our dentists and popular culture have always touted the benefits of great oral health care — brushing your teeth, flossing regularly, and visiting your dentist at least twice a year.
What a lot of people don’t realize is that good oral care extends beyond your teeth, gums and mouth. Here are some studies that suggest that good oral health can also help reduce heart disease, osteoporosis, rheumatoid arthritis, and diabetes.
Heart Disease and Gum Disease
People who have gum disease are two to three times more likely to have heart disease, according to Harvard Health Publishing, although there may not be a direct link. Harvard suggests that people who don’t follow good oral health likely don’t follow other overall good health practices, which is why there is a link between people who have gum disease (periodontitis) and people who have heart disease.

With that said, how, then, does good oral health contribute to good cardiac health? Oral health extends beyond merely brushing and flossing your teeth. It also involves decreasing your sugar intake, quitting smoking, and losing weight. There are some studies that suggest that inflammation in the mouth can cause or worsen inflammation of blood vessels. Also, an increase in plaque in the mouth has a link to plaque in blood vessels.
Osteoporosis and Oral Care
Osteoporosis is a condition that causes bones to become less dense and more brittle. It is more common among older people, and more common among women than men. One of the risks with osteoporosis is fractures.
According to the NIH’s Osteoporosis and Related Bone Diseases National Resource Center, there is a strong connection between bone loss (osteoporosis) and tooth loss. In fact, women who have osteoporosis are three times more likely to lose their teeth as well.

Does one cause the other? The NIH says that isn’t clear. There’s a link but not necessarily a cause and effect. People who do not eat good diets are more likely to experience osteoporosis and periodontitis.
Bottom line: Visit your dentist at least twice a year for regular checkups, cleanings, and X-rays. Board certified dentists are trained to identify signs of bone decay, which can be a signal of bone loss throughout the skeletal system.
Rheumatoid Arthritis and Dental Care
Rheumatoid arthritis is an autoimmune disease that causes inflammation, pain and swelling in the body’s tissues and joints.
The research here is less about whether there is a direct link or cause-and-effect relationship between RA and oral health. It’s more about how practicing good oral health is even more important for people who suffer from autoimmune diseases.
An article published on Johns Hopkins Arthritis Center explains that some medications that RA patients take can also cause some mouth ulcers and other oral problems. That is why it is very important to brush and floss your teeth, as well as use a high quality mouthwash that not only protects against plaque buildup but also contains fluoride to promote remineralization.
Bottom line: Everyone should practice good oral health, but it is especially important for people who suffer from rheumatoid arthritis (RA) and other autoimmune diseases in order to prevent the spread of infections and tooth decay.
Diabetes and Oral Health
While poor oral hygiene does not cause diabetes, it is important for people who have diabetes or are at risk for it to step up their dental care. Why? Diabetes sufferers are at higher risk for periodontal disease. Also, diabetes slows healing, so healthy gums and teeth lessen the risk for infection or diseases that originate in your mouth.
Bottom line: If you have diabetes or are at risk for it, step up your brushing, flossing and preventive dental care. Good oral health care could be the difference between living well with diabetes and struggling with it.
Healthy Mouth, Healthy You
The American Dental Association recommends the following for your oral health:
● Brush your teeth twice a day.
● Floss or use an interdental cleaner (like a dental pick) once a day.
● Add an alcohol-free mouthwash if needed, as per your dentist.
● See your dentist twice a year for regular checkups, cleanings and X-rays.
● Don’t smoke.
● See your dentist if you note signs of gum disease (bleeding, swelling, tenderness, odor).
(11/30/2024)by Pittsburgh Healthcare Report
More Information: https://www.pittsburghhealthcarereport.com/who-knew-brushing-your-teeth-could-be-life-saving-how-good-oral-health-care-can-reduce-other-health-risks/
Views: 289
Four Ways To Keep Up Good Dental Hygiene As You Get Older
Good dental hygiene and oral care habits are important at any age. But as you get older, you might find yourself wondering if your dental routine needs some tweaking, or if certain life changes have also caused changes in your mouth. Whether you have all of your original teeth, some of them or a full set of dentures, diligently caring for your mouth is just as important when you get older as it was when you were a kid.
1.- Fluoride Is Still Important
Fluoride isn't just for children. Even if you're over 50, it's still important to protect the surface of your teeth and ward off decay. The Mayo Clinic notes that older individuals have an increased risk for cavities, making it doubly important for you to make sure fluoride is a part of your daily routine. When brushing – twice a day – use a fluoride toothpaste. Drinking fluoridated tap water can also help you defend against tooth decay as you get older. If you are particularly concerned about cavities or have had a few as you've aged, your dentist might even give you an in-office fluoride treatment for an added level of protection.
2.- Watch Out for Dry Mouth

Although getting older doesn't necessarily make dry mouth more likely, certain features of aging, such as more regular medications or a chronic condition, can increase your risk for dry mouth – along with cavities or decay. Dry mouth can also affect the fit of your dentures, according to the National Institute of Dental and Craniofacial Research, often causing chafing between the dentures and your gums.
If you suffer from dry mouth, there are a few improvements you can make to your dental hygiene to reduce your symptoms. You can use a moisturizing mouthwash or spray, or chew sugar-free gum, which encourages the production of saliva. Another option is to use an artificial saliva product, often available from the pharmacy without a prescription. According to the American Dental Association, it contains ingredients that allow it to closely mimic real saliva.
You can also consult your doctor or dentist if your dry mouth is caused by medication. Adjusting your dose or trying a new medicine can help alleviate certain symptoms.
3.- Caring for Your Dentures

According to the American College of Prosthodontists, more than 178 million people in the United States are missing at least one tooth, and tooth loss is more likely to occur in older people. If you're among that group, it's still important to take care of those dentures just as you would care for real teeth. Use a toothpaste that is specially made for dentures, and make sure you clean them on a daily basis. You'll also want to brush your gums and tongue with a soft toothbrush to remove any bacteria and food particles from your mouth. If you have partial dentures, be sure to floss between the implants before you put the dentures back in. Your dentist can give you specific instructions on taking care of your dentures, so that they last as long as possible.
4.- Don't Forget about Gum Disease
Whether or not you have all of your real teeth, gum disease remains a big concern among older individuals. A study published in the Journal of Dental Research found that nearly 64 percent of adults over age 65 had severe or moderate periodontitis in 2009 and 2010. Albeit common, gum disease doesn't have to be a cost of getting older. Maintaining good dental hygiene and seeing your dentist regularly will help you prevent it or treat it quickly.
A healthy smile looks great at any age. Keeping up with good hygiene habits, visiting your dentist regularly and making changes to your routine as your body changes will help you keep a great-looking smile for life.
(11/29/2024)by Colgate
More Information: https://www.colgate.com/en-za/oral-health/oral-care-age-55-up/four-ways-to-keep-up-good-dental-hygiene-as-you-get-older-1014
Views: 274
What To Look For In An Endodontist
If you find yourself needing a root canal, your dentist will likely refer you to an endodontist. Many of us have little to no experience with dental care outside of regular cleanings. If you fall into this category, the term endodontist may be new to you.
You may even ask yourself, how is an endodontist different than a dentist. Learning more about this dental specialty and what to look for will give you peace of mind knowing that you’re selecting the best endodontist in Ellicott City.
If you’re in need of an endodontist, reach out to Dr. Lina Jarboe and Dr. Burton Waxman at Access Endodontics today. You can reach our team at 410.936.4478 or connect with us online to learn more.
What Are Endodontics?

This particular field of dentistry focuses on the study and treatment of the inner tooth, including the dental pulp. An endodontist’s job generally revolves around saving and preserving teeth that are damaged, decayed, or that have suffered an injury. While your dentist covers the regular checkups, fillings, and cosmetic procedures, your endodontist will diagnose and resolve tooth pain. They use specialized technology to perform procedures that are beyond a general dentist’s capabilities.
Typically, endodontics will perform root canals and other procedures based on referrals. If you’re experiencing tooth pain, reach out to your dentist right away.
Qualities of a Great Endodontist
When you need a serious dental procedure done, you want to know you’re in the hands of a professional you can trust. To ensure that your endodontist is that sort of professional, be sure that they have the following four qualities.

Proper Qualifications
Endodontics is a specialized field of dentistry that requires two extra years of postdoctoral education at an accredited dental school. The person providing your endodontics services should have received this education at an accredited institution by the American Dental Association (ADA). This signifies that your endodontist has displayed a high level of expertise and knowledge in their field of study and has passed rigorous testing from certified professionals.
Specialization in Your Area of Need
Endodontics is a specialized area of dentistry. Finding an endodontist with experience, chairside manner and knowledge, will ensure that you have a positive visit. Some endodontists are highly specialized, focusing on a specific procedure. For example, certain endodontists have built their reputation off of root canal procedures. They may be great at what they do, but they also may not be the dental professional you’re looking for if you need anything other than a root canal. Your dentist should refer you to an endodontist that skillset matches the services you require.
Use of Cutting-Edge Technology
Endodontics, just like all other fields of dentistry, relies heavily on technological advances that allow practitioners to perform their procedures with greater ease, greater precision, and with less pain and recovery time for the patient. The use of cutting-edge technology requires dental professionals continually enhance their skillset and obtain additional training. When your endodontist uses the latest technologies and treatment techniques, it shows a willingness for continued learning and a desire to invest their time in providing patients with the best experience possible.
Good Chairside Manner
Qualifications, expertise, and cutting-edge technology are certainly important qualities of a great endodontist. But if your doctor is unfriendly, or unaccommodating, it can make your endodontic procedure more complicated than necessary. To find out if your endodontist has a good chairside manner, you can look up “endodontics Ellicott City” and read some reviews for the top results. Otherwise, you can stop in and have a preliminary meeting with one before your procedure is performed.
(11/28/2024)by Access Endodontics
More Information: N
Views: 263
Signs Of A Cavity In Between Teeth
You know the importance of brushing your teeth and having good oral hygiene to avoid cavities. But did you know that cavities aren't just in your teeth?
Yes, even when you take care of your enamel, you can still end up with a cavity between your teeth. This has a technical term called an interproximal cavity. It forms like other cavities: when the enamel is worn away and bacteria are able to get into the tooth.
When this happens with your permanent teeth, it can cause tooth pain that you don't want to have to deal with, as well as other problems when the cavity penetrates into the bloodstream.
The Goal is to Keep Your Healthy Teeth Free From Decay

Preventive dentistry is the best way to make sure you don't end up with interproximal cavities and tooth decay. These tips will teach you how to recognize if you have the signs of a cavity in your teeth and how to prevent cavities in general.
Keep in mind that if you're concerned that you may have a cavity, you should contact your dentist early. The sooner the problem is taken care of, the less likely you'll need more serious fixes like a dental crown or root canal treatment.
Understand What a Cavity Is
You've been taught to brush your teeth since childhood to avoid cavities. But what exactly is this dental concern, anyway? And do you really need to floss?

A cavity is an easily preventable dental condition in which the hard surface of your teeth (the enamel) ends up with a tiny hole in it. This permanent damage is caused when the bacteria stick to the tooth.
Cavities Can Be Avoided With Regular Care
As you engage in frequent snacking, eat sugary foods or drink sugary drinks, and don't effectively clean right after, the food particles form dental plaque.
As plaque, bacteria sticks to the enamel and decays the tooth. If you don't remove decay fast, it turns into a hole that requires a large filling to fix it. However, if it's caught early, the enamel could be recalcified with fluoride gel.
Preventing a Cavity
The best way to prevent interproximal cavities and other cavity types, according to the American Dental Association, is to brush at least twice a day.
Use toothpaste with fluoride to get rid of the bacteria, and follow with flossing and a mouth rinse. Fluoride is a commonly added ingredient to most over-the-counter tooth products.
Tooth Sensitivity? Stop What You're Doing and Check Your Technique
If you notice tooth sensitivity, you could be using the wrong brush. Always use a soft-bristled toothbrush unless your dentist recommends otherwise. Brush your teeth in a circular pattern, and include your gums to prevent gum disease.
Habits Are Important, Too
Flossing is important since interproximal cavities form between the teeth, and the floss and mouthwash get up in those hard-to-reach places.
Avoid sugary snacks and drinks, quit habits like using tobacco, and head to your dentist during office hours for preventative cleanings. If you need professional help quitting bad habits, your primary doctor can provide medical advice.
Recognize the Symptoms of Interproximal Cavities
If you're concerned that something isn't quite right, but you're not sure what's going on with your teeth, look for these symptoms to guide you:
Sensitivity to heat or cold- This is usually one of the first side effects you'll notice as the cavity erodes your enamel and gets into the second layer of tissue, the dentin. Once temperatures reach this layer, discomfort is the natural side effect.
Pain in the teeth - Sensitivity is annoying but it goes away. Pain, on the other hand, is different. It's constant, mild to moderate, and often throbbing. It can be hard to narrow down where the pain is coming from because it feels like it's in your other teeth, too. The dentist can take x rays to figure out where the interproximal cavity is.
Bad breath - Officially called halitosis, bad breath is a warning that there's tooth decay going on somewhere. Halitosis is harder to diagnose yourself, but if you know you have it, you want it gone quickly.
Browning or yellowing teeth - When you see dark spots on your teeth, it's not normal. This is a sign that a hole is beginning to form inside the tooth. It can be recalcified with fluoride gel if you catch it before tooth decay becomes a hole. At that point, the dentist can use tooth colored filling material to cover the hole, but it can't be reversed.
Abscesses or pus forming - If you have a weird spot on your gums that is beginning to show pus, it's a sign your cavities have progressed. This means you have to schedule an ASAP visit with your dentist before your interproximal cavity requires a root canal, bridge or dental implant.
Chips - Sometimes, a chip or broken tooth occurs without us realizing it. If you ate something hard or sticky, it could have cracked the top layer. To prevent cavities from destroying the tooth, the dentist can place a natural looking cover over the tooth or add a filling treatment. This keeps plaque from getting into the dentin and causing discomfort. But a chip or crack that isn't treated becomes a serious dental issue, often requiring a root canal to correct.
Head to the Dentist Before You Think You Have a Cavity
So how can you avoid interproximal cavities between two teeth or cavities in general? The best thing to do is to seek out preventative care at least every six months, according to the American Dental Association.
Professional cleanings and dental exams help catch problems early, before cavities can form. And if you do need a filling, the dentist can use a variety of metal alloys to solve minor issues.
Prevention or Early Care, Either Way is a Good Reason to Visit the Dentist
Interproximal cavities form when bacteria is ignored and allowed to run rampant. Head to your dentist for routine visits, and call for an urgent appointment if you think you may have an interproximal cavity or any other dental issues.
(11/23/2024)by Charlotte Emergency Dental
More Information: https://www.charlotteemergencydental.com/blog/signs-of-a-cavity-in-between-teeth/
Views: 337
How anger issues could be wrecking your teeth
Grinding your teeth (bruxism) is widely thought of as a sleep-related disorder. Many bruxers who clench or grind their teeth during the night have other sleep disorders, such as snoring and pauses in breathing (sleep apnea).
But there could be another reason for your teeth grinding — be it during the day or night. Doctors still don’t completely understand the causes, says Mayo Clinic, but intense emotions such as anxiety, stress, anger, frustration or tension could be at the root of the problem. Meaning the more stressed you are, the more likely you are to start bruxing.
“Nervous tension, anger and frustration can cause people to start showing the signs of bruxism without even knowing it,” says California clinic Delta Dental.
Last week, writer Hale Goetz revealed how her own anger management issues were “destroying” her teeth. During a visit to her dentist, he revealed her canines were flat and told her she would need a mouth guard if she wanted to prevent nerve damage.

As a lifelong bruxer, the impact of extreme habitual grinding was “inevitable” to Goetz. When it was pointed out to her by her dentist, using a pair of false teeth to show just how out of line her jaw had been moving to flatten her teeth, she began to notice just how much of a grinder she was and how it was more extreme when she was in a state of emotional conflict.
A mouth guard is typically the first step a dentist will recommend toward preventing or correcting damage to the teeth, as it keeps the teeth separated to soften the impact of any clenching or grinding. Goetz says her mouth guard has two roles: It does its job by protecting her teeth, but also (and perhaps more importantly) it serves as a useful self-care gauge. The deeper the notches in her mouth guard, the more attention she needs to pay to her emotional well-being.
“Bruxism is often associated with anxiety and stress as are some anger management issues,” says Fredrick Wade from Addiction Medicine. “When one is treating anger management, learning stress management techniques is essential as it can be for those who suffer with bruxism.”

“If stress is the cause [of bruxism], you need to find a way to relax,” says the American Dental Association. “Meditation, counseling and exercise can all help reduce stress and anxiety.”
Other self-care tips for bruxism are listening to music, taking a warm bath and exercising. Stay away from stimulating substances (including alcohol, caffeine and nicotine) in the evening, and try to say goodnight to technology at least 30 minutes before you go to bed.
(11/14/2024)by Sheknows
More Information: N
Views: 319
The Truth About Your Toothbrush And Germs
Your toothbrush is home to more than 100 million bacteria including E. coli and staphylococci (Staph) bacteria, according to researchers at the University of Manchester in England. And the University of Alabama at Birmingham found that fecal germs were on your toothbrushes too.
All that sounds gross, but you needn't panic. Your mouth is also full of bacteria and your toothbrush probably won't make you sick, but there are ways to keep it clean so you stay healthy.
Mouthful of Bacteria
"There (are) hundreds of microorganisms in our mouths every day," says Gayle McCombs, RDH, MS, associate professor and director of the Dental Hygiene Research Center at Old Dominion University.
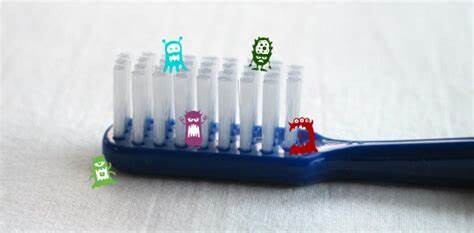
Even plaque – the stuff you are trying to brush off your teeth – is composed mainly by a type of bacteria.
None of this is cause for concern unless there is an unhealthy balance of bacteria in the mouth.
How Brushing Your Teeth Hurts
Brushing your teeth, particularly with an electric toothbrush, can actually push germs under your gums, says R. Thomas Glass, DDS, PhD, professor of dentistry and pathology at Oklahoma State University Center for Health Sciences.

Most of these germs already exist in your mouth so you probably won't get sick from them. However, if others use your toothbrush (or you use someone else's) germs can be spread.
The thing to worry about is recurring illness. "When your resistance is low, that's when this becomes clinically important," he says. "In essence, you are re-infecting yourself," says Glass.
Could Your Toothbrush Be Making You Sick?
You probably won't get an infection from your own toothbrush. Even if your brush is covered in bacteria, your immune system can usually take care of any bacterial invaders. However, you should still care for your toothbrush properly and keep it clean. The following slides discuss some ways to care for and store your toothbrush properly to minimize the chance of illness.
Don't Brush Where You Flush
Where you store your toothbrush in your bathroom is important. In most bathrooms, the toilet is very close to the sink, where most people keep their toothbrushes. Every time you flush, bacteria are released into the air – and you don't want that bacteria to get on your toothbrush.
"It's just common sense to store your toothbrush as far away from the toilet as possible," says McCombs. Keep it in a medicine cabinet if possible, and always close the toilet lid before flushing to minimize the spread of bacteria onto your toothbrush.
Toothbrush Holders
Toothbrush holders as well can pick up bacteria that are spread by toilet flushing. A study by the National Sanitation Foundation (NSF) found that toothbrush holders are the third-most germy household items (behind dish sponges and kitchen sinks). Remember to clean your toothbrush holder regularly to remove germs.
Toothbrush Storage Tips
After you've moved your toothbrush as far from the toilet as possible, and cleaned your toothbrush holder, here are some storage tips to keep your toothbrush as germ-free as possible:
Rinse your toothbrush thoroughly with tap water every time you use it.
Let your toothbrush dry thoroughly between brushings. Don't use toothbrush covers, which can create a moist enclosed breeding ground for bacteria.
Keep your toothbrush upright in a holder, rather than lying it down.
Don't ever use anyone else's toothbrush, or let someone use yours.
Keep toothbrushes separate. If toothbrushes touch, they can swap germs.
Do Toothbrush Sanitizers Really Work?
There are products available that claim to sanitize your toothbrush. Some use ultraviolet light; others are sprays or rinses. There are even brushes with built-in antibacterial bristles. While some of these products do kill some germs, there is no evidence using them will reduce your risk of illness.
The American Dental Association (ADA) states soaking your toothbrush in an antibacterial mouth rinse after use may reduce the number of bacteria on your toothbrush.
Just make sure you do not try to sterilize your toothbrush in a microwave or dishwasher. According to the ADA, most toothbrushes are not made to withstand these conditions and doing so might damage the brush and reduce its effectiveness.
When to Toss Your Toothbrush
The ADA recommends replacing your toothbrush every three to four months, or more often if bristles become frayed, if you are sick, or if you have a weakened immune system. For an electric toothbrush, replace the head as frequently as you would a regular disposable brush. Children's toothbrushes may need to be replaced more often than adult brushes.
Remember, "Bacteria cause gum disease, and decay, and bad breath," says dentist Kimberly Harms, DDS, consumer advisor for the ADA. Harms recommends brushing and flossing as often as possible, and rinsing your mouth with an antibacterial mouthwash before you brush to eliminate bacteria before they get onto your toothbrush.
(11/13/2024)by Medicinenet
More Information: https://www.medicinenet.com/truth_about_your_toothbrush_pictures_slideshow/article.htm
Views: 577
Do You Have Enamel Erosion?
While your tooth enamel is the hardest substance in your body, certain lifestyle habits, medical conditions, and food choices can cause it to erode and become sensitive.
We put our teeth through a lot in our lifetime, including the hours we spend eating and drinking. The tooth surfaces must deal with a constantly changing environment. One area that sometimes gets overlooked when choosing our diet is the acidity in maybe causing to our teeth.
Enamel is the hardest substance found in the body but even this amazingly tough outer tooth layer can be damaged by a pH environment lower than 5.5. The pH 0 being the most acidic. If these harsh conditions occur frequently then the top layer can be eroded away over time.
The appearance of acid erosion differs from other types of tooth substance loss as it is smoother in appearance making it less obvious to spot. Here’s what to look out for:

Saucer shaped depressions, wearing away of biting surfaces and edges that have a smooth shiny appearance.
Thinner enamel or dentine which sometimes has a darker yellow/brown coloring.
These visual symptoms are often accompanied by sensitivity to hot, cold, and sweet stimulates
The surface of the tooth can also feel different to the tongue and touch usually feeling rougher.

Causes include internal factors such as:
Gastroesophageal reflux or acid reflux. This can be caused by food/drink, smoking, pregnancy, and medical conditions such as hiatus hernia.
Bulimia is eating disorder which causes frequent vomiting to control a person’s food intake. This causes the enamel to be in contact with strong acids in the stomach.
Binge drinking and alcoholism can also induce regular vomiting. The acid in the stomach has a pH around 1.
External factors:
Foods include acidic fruit such as citrus fruits, apples, and tomatoes.
Anything that has been pickled or preserved in vinegar is also a high risk.
Drinks such as sodas, alcohol and fruit juices are obvious dangers but there are some hidden risks with people not realizing the acidic dangers. These might take you by surprise.
Lemon slice in hot water. Often taken for its health benefits but the pH of lemon juice is around 2 so adding this to hot water almost creates hot acid. As a comparison the pH of soda usually sits around 2.5.
Carbonated water has a pH of 3-4 which is often overlooked.
Sport drinks and flavored waters.
Here what to do to help reduce and prevent loss of tooth surface:
Avoid regular intake of food and drink that is acidic. If you’re drinking something that is acidic then drinking through a straw can reduce the amount of contact, do not hold carbonated drinks in your mouth before swallowing. Eating the most acidic item first follow but something less acidic can help.
Brush your teeth with fluoride toothpaste twice a day for 2 minutes with a soft manual brush or good quality electric toothbrush, preferably one that has a pressure feature.
The American Dental Association recommends waiting 60 minutes after eating or drinking to brush your teeth as this can cause the softened enamel to be brushed away. The saliva will help return the pH levels but chewing sugar-free gum can also help this process.
Visit your dentist and dental hygienist regularly to ensure a healthy mouth and get tips and guidance for your home care. Also seek medical guidance for any of the internal issues that could be causing erosion.
(11/12/2024)by Dr. Michael's dental clinic
More Information: https://www.drmichaels.com/blog/do-you-have-enamel-erosion
Views: 512
Are Dental X-rays Safe During Pregnancy?
Are you do a dental checkup, which involves taking a dental X-ray? Dental X-rays are an important tool for dentists as they allow them to assess your oral health beneath the surface of your teeth and gums. Dental X-rays are considered safe for most people.
However, are dental X-rays safe during pregnancy? If you are pregnant and due for a dental X-ray is safe to go ahead with it or should you postpone until you have given birth?
Continue reading the article as we answer these and other questions about dental care during pregnancy.
Why Do Dentists Use X-Rays?

Dental X-rays, which are also known as radiographs, are a non-invasive procedure. They allow dentists to diagnose various oral health issues that cannot be detected with the naked eye.
By analyzing X-rays, dentists can identify dental problems early before they become serious issues and start causing patients discomfort or pain. They can help prevent infections and other serious oral health problems and address them before they require more expensive and extensive treatment.
Types of Dental X-Rays
There is a range of X-rays dentists can use depending on the situation. For example, they can use them to identify cavities below the surface of a tooth, evaluate orthodontic issues, monitor how previous work such as root canals is progressing, and monitor a child’s dental development.

X-rays commonly used in dentistry include:
bitewings for detecting tooth decay and periodontal, which are gum health problems
full mouth series help establish a baseline of your overall dental health and include approximately twenty X-rays usually taken on your first visit to a new dentist
panoramic X-rays are used to evaluate not just your tooth and gum health but the health of the whole mouth and the surrounding area
periapical X-rays focus on a single area of your mouth. For example, if you have pain in a certain area or the dentist is doing a root canal.
All the above radiographs use electromagnetic radiation in short bursts to capture an image. In the X-ray images, issues such as cavities and infections look darker than healthy teeth and gums. The amount of radiation emitted during the image capturing is small and safe.
It is natural to be concerned about the health of your baby and worry about radiation exposure if you have to have dental X-rays. However, having dental X-rays while you are expecting is perfectly safe.
The American Dental Association (ADA) has stated that dental X-rays are safe for all, including pregnant women and children. When you have a dental X-ray, the exposure is focused on your mouth, away from the fetus and it will not harm it at all.
X-Ray Safety Standards
Both dentists and dental hygienists and their assistants have trained to deliver dental X-rays safely. They are required to follow strict safety standards published by the Food and Drug Administration (FDA).
All X-ray equipment must be licensed and inspected every year. The X-ray technologies are regulated by the local authorities as well as the state who also ensure the safety guidelines are followed by all dental practices.
Your and Your Baby’s Safety During a Dental X-Ray
Your dentist will ensure the safety of you and your unborn child by adhering to the safety guidelines, which include:
only using equipment that has been licensed and inspected by the authorities
placing a protective leaded apron on your abdomen, which will block radiation from the X-ray
short exposure time
lower level of radiation exposure than is used in most other imaging technologies used in the medical field
Dental diagnostic X-ray imaging does not use high levels of radiation that could harm a developing fetus. In addition, the focus is on the mouth, so it is not near the baby, who also has additional protection from the apron.
In addition, the potential to diagnose problems that could compromise the mother’s health is considered to outweigh the risks, which are minimal.
New Technologies Have Improved Safety of Dental X-Rays
Modern technologies have greatly improved the safety of X-ray imaging. Instead of photographic film that was used in conventional X-rays, today dentists can use digital images. This has greatly reduced the amount of exposure since digital images need approximately 80% less radiation exposure than film.
An additional advance has been technology known as Cone Beam Computerized Tomography, CBCT for short. It is used to create a 3D panoramic image of the whole dental anatomy of a patient. The images created using CBCT minimize radiation exposure and are more accurate than 2D X-rays.
Should You Delay Having a Dental X-Ray if You Are Pregnant?
Dental X-rays are part of a comprehensive dental examination and an important diagnostic tool for dentists. The ADA recommends that all adults have a dental X-ray once every one or two years, depending on the overall oral health of the patient.
If you choose to delay your X-rays, it could mean that dental diseases, tooth decay, gum disease, or other dental issues go undiagnosed. If not noticed and addressed in time, the problems could get worse and cause pain and lead to more serious dental health complications.
Because the risks are minimal, it is best not to delay your dental X-rays. However, some patients choose to delay them slightly, just until they are through the first trimester. They do this because the first trimester is the most active time in the development of the fetus.
If you are pregnant or think you could be pregnant, make sure to disclose this to your dentist. You can also discuss any concerns you have about dental X-rays or other dental procedures with your dentist. They will be able to advise you further on these issues.
Oral Health Problems During Pregnancy
When you are pregnant, you may experience increased acidity in your mouth because of sugary cravings and morning sickness, For some pregnant women, hormonal changes can cause gingivitis. This is a gum disease where the gums bleed easily, become inflamed, and develop an exaggerated response to plaque.
If gingivitis is left untreated, it can become periodontitis, which is a more serious condition. Periodontitis causes the gums to recede and the teeth can become loose and fall out.
In the worst cases, dental issues such as periodontitis could lead to complications in pregnancy. For example, inflammation and periodontitis could result in pre-term delivery, low birth weight, and pre-eclampsia.
Is It Safe to Have Dental Surgery When Pregnant?
If you need dental surgery while you are pregnant, there are no reasons not to go ahead with it. Once your dentist knows you are pregnant, they will pick an anesthetic that is safe to use when you are expecting.
It is best not to delay your dental surgery because of your pregnancy. If the issue is not treated, it will have time to grow and you may end up needing more complicated and expensive surgery as a result. Dental issues could also lead to loss of teeth and even issues with your pregnancy.
Plan Ahead
If you are planning to get pregnant, it is a good idea to include your oral health in your plans. Get an appointment booked with your dentist to get your teeth and gums checked in advance and then you will not have to worry about dental appointments, X-rays, or other procedures during the pregnancy.
During your appointment, you can also talk to your dentist about looking after your teeth when you are pregnant. They can advise you about potential changes that pregnancy can cause in your mouth and how to address them.
Looking After Your Teeth While Pregnant
It is just as important to look after your teeth while you are pregnant as it is at other times. It is the best way to prevent dental issues before, during, and after pregnancy. Keep up your dental hygiene by brushing twice a day and flossing once a day and do not skip scheduled dental checkups.
(10/09/2024)by CDHP Dental Health Project
More Information: N
Views: 281
Things You Should Never Do Before Going To The Dentist
Ah, the dentist. The haven of good dental hygiene, and for many, one of those places you really don't want to go. Despite a visit to the dentist being essential for maintaining good oral health, and most dentists doing everything in their power to make your visit as stress-free as possible, a huge amount of people are scared of the chair. One 2014 study published by Medical Principles and Practice found that 36 percent of people experience dental anxiety when in the dentist's office or before a visit, and 12 percent of those experience extreme fear.
Yet despite this trepidation, Americans seem to understand the importance of getting their teeth checked. As Delta Dental reported, approximately 93 percent of Americans plan on visiting the dentist in 2021. But in your fear of opening wide and saying ahh, you might be tempted to do some things before your check-up which could prove less than useful. If you're due for an appointment soon, sink your teeth into the following things you should never do before going to the dentist.
Avoid putting on too much makeup before seeing the dentist
Shutterstock

You might not think twice before putting on a face full of makeup before heading to the dentist, but it's a surprisingly annoying factor for your dentist. According to Savannah Dental Solutions, a dental practice in Savannah, Georgia, run by Chad and Alexandra Schnabel, "Dental procedures involve placing hands, tools, and water inside your mouth. Depending on exactly what you are having done, your mouth may also be numbed. Since the area around your mouth will likely get messy, it's best to skip the lipstick, foundation, and full face powder." That said, the dentists noted that blush and mascara are fine.
Try your best to arrive with a mostly bare face to avoid any unwelcome mess for the professionals perfecting your smile, and consider packing your makeup bag if you have to head somewhere else after your appointment. As Savannah Dental Solutions explained, "If you're heading to work or a social engagement after your appointment, you can always freshen up and apply makeup in the restroom on your way out."
Don't bring a picture of your dream teeth to a cosmetic dental consultation
Shutterstock

The Hollywood smile is a much-coveted look for some people, which is why it's not surprising that dentists are routinely asked how they can get an A-lister's stunning grin when stopping in for a cosmetic dental consultation. According to doctor of dental surgery Jay Grossman, however, bringing in a picture of your "dream teeth" isn't exactly a feasible way to approach dental work.
In an article for The Healthy, he explained, "Patients come in with pictures of celebrities and say, 'I want to look just like her.' I'm sitting there thinking, You can't have a smile that looks like Angelina Jolie's, because you don't have a face that fits those teeth. It's like when you get your hair color done — you can't just put the same highlights or lowlights in everybody's hair." Of course, having an idea of what you're hoping to achieve is wise, but don't get too set on a specific look.
Never keep your medical history a secret from your dentist
Shutterstock
A dentist appointment is a medical appointment, and should be treated as such. Unfortunately, though, when it comes to oral procedures, patients can forget that they need to be as open and upfront about any medical history as they would be with their primary doctor. Not doing so can be downright dangerous.
According to Martin Hogan, dentist and division director of the Oral Health Center at Loyola University Medical Center in Illinois, it's vital to share information beforehand so your dentist knows how best to treat you. In an interview with Medical Xpress, he explained, "If you have experienced a serious health condition such as a surgery or been diagnosed with a chronic condition, you need to tell your dentist before you come for your appointment. Depending on the illness, you may need to be premedicated with antibiotics to prevent infection."
This premedication, according to Hogan, is important. "Pretreatment one hour before the appointment with an antibiotic is recommended for patients with certain health conditions," the dentist revealed. Without it, your appointment "must be rescheduled ... resulting in a wasted trip."
If you're going to need medication, don't drink alcohol before your dentist appointment
This may seem like a no-brainer, but considering the anxiety that can surround a trip to the dentist, it's easy to see why people would be tempted to indulge in a drink or two before an appointment. However, doing so could mean trouble when you arrive at the practice, particularly if you're visiting to undergo treatment that requires medication.
Dr. David Potts, dentist for County Family Dental Care in Libertyville, Illinois, explained, "Of course, you could drink wine before going to the dentist, but it will affect [your] treatment. There will be some counter-indications between the wine and some dental medication." This could leave you at risk of having to reschedule your appointment or worse, you could put your health in danger.
If you're feeling a little nervous around your treatment, Potts advised, "You might consider doing some form of sedation dentistry instead. That won't keep you from any form of treatment, but will give you the same relaxed feeling you can get from wine."
If you're going in for a root canal, don't take painkillers
It seems pretty logical, right? For a procedure considered to be as frightening and painful as a root canal (although interestingly, only 17 percent of people actually consider it their "most painful dental experience," according to the American Association of Endodontists), taking some pain medication beforehand feels like the smart thing to do.
However, taking painkillers before arriving at the dentist may be an unwise move, and for more than one reason. As Downtown Dental, a dental practice in Greenville, South Carolina revealed, anesthesia is typically administered before a root canal begins, meaning there's no need for any over-the-counter medications. Also by taking painkillers, you're, well, killing the pain. This is a problem because your dentist may actually need for you to identify exactly where the pain is located before they can get to work. Even if you're nervous about the potential for pain, leave the medicating to the dentist.
If you're having dental surgery, don't wear contact lenses
It might seem like forgoing glasses and opting for contacts would be the more comfortable choice in the dentist's chair, what with the amount of stuff going on in and around your mouth during a procedure. The less on your face, the better, right? Well, this isn't quite the case, particularly if you're undergoing oral surgery.
According to Verywell Health, wearing contacts during surgery can be problematic if you're having to undergo a general anesthetic. This is because your eyes may need to remain closed for an extended period of time. While a short period of your eyes being closed isn't too risky, longer periods of wearing contact lenses with your eyes shut can raise your risk of eye infection, as well as being generally uncomfortable to remove afterward (via Healthline).
Also, if you're going to need oral surgery, make sure to wear practical, comfortable clothing, remove any jewelry beforehand, and if you have longer hair, tie it back so it's away from your face. The more you can help your dentist do what they need to do, the easier the procedure will be.
Don't step up your dental hygiene suddenly before seeing the dentist
Look, we get it. Going to the dentist strikes fear into the heart of even the most diligent flosser. And if it's been a while since you've had an exam, you might feel like putting in the hours on your dental hygiene just before your appointment. However, doing this is futile. After all, dental hygiene is a lifelong endeavor, and trying to make up for lost time may cause you a fair amount of discomfort.
More to the point, your dentist can tell. Martin Hogan, doctor of dental surgery and division director of the Oral Health Center at Loyola University Medical Center, told Medical Xpress, "Sometimes we will see the gum tissue slightly irritated and when asking patients about this, they mention that they have been flossing 'extra hard' the past few days in anticipation of their dental visit. Other times we may see the gum tissue slightly dried out, which often is caused by excessive use of alcohol-containing mouth rinses." So while we get why you'd do this, it isn't helping you and it certainly isn't fooling your dentist. Instead, focus on practicing good oral hygiene consistently. That's the way to save face with your dentist.
Don't smoke before coming to the dentist
Although smoking rates are on the decline in the U.S. — from 20.9 percent of adults in 2005 to 14 percent in 2019, per the CDC – it's far from rare. And with the myriad health complications that smoking can cause, it's little surprise that your dentist also isn't a huge fan of the harmful habit. As Ada Cooper, a New York City-based dentist and spokesperson for the American Dental Association, told The Healthy, "Smoking is something patients shouldn't do period, but definitely not before the dentist."
Smoking can lead to tooth staining, bad breath, inflammation of your salivary gland openings, and heightened plaque and tartar build-up on your teeth, all of which can cause headaches for your dentist when trying to administer treatment (via WebMD). And that's all before the fact that smoking can also lead to a higher risk of gum disease, longer healing times after dental surgery and procedures, and a higher prevalence of developing oral cancer. If it wasn't time to quit before, it could be now.
(09/12/2024)by Health Digest
More Information: N
Views: 393
The Ugly Truth About Your Toothbrush & Germs
Your toothbrush is home to more than 100 million bacteria including E. coli and staphylococci (Staph) bacteria, according to researchers at the University of Manchester in England. And the University of Alabama at Birmingham found that fecal germs were on your toothbrushes too.
All that sounds gross, but you needn't panic. Your mouth is also full of bacteria and your toothbrush probably won't make you sick, but there are ways to keep it clean so you stay healthy.
"There (are) hundreds of microorganisms in our mouths every day," says Gayle McCombs, RDH, MS, associate professor and director of the Dental Hygiene Research Center at Old Dominion University.
Even plaque – the stuff you are trying to brush off your teeth – is composed mainly by a type of bacteria.

None of this is cause for concern unless there is an unhealthy balance of bacteria in the mouth.
Brushing your teeth, particularly with an electric toothbrush, can actually push germs under your gums, says R. Thomas Glass, DDS, PhD, professor of dentistry and pathology at Oklahoma State University Center for Health Sciences.
Most of these germs already exist in your mouth so you probably won't get sick from them. However, if others use your toothbrush (or you use someone else's) germs can be spread.
The thing to worry about is recurring illness. "When your resistance is low, that's when this becomes clinically important," he says. "In essence, you are re-infecting yourself," says Glass.

You probably won't get an infection from your own toothbrush. Even if your brush is covered in bacteria, your immune system can usually take care of any bacterial invaders. However, you should still care for your toothbrush properly and keep it clean. The following slides discuss some ways to care for and store your toothbrush properly to minimize the chance of illness.
Where you store your toothbrush in your bathroom is important. In most bathrooms, the toilet is very close to the sink, where most people keep their toothbrushes. Every time you flush, bacteria are released into the air – and you don't want that bacteria to get on your toothbrush.
"It's just common sense to store your toothbrush as far away from the toilet as possible," says McCombs. Keep it in a medicine cabinet if possible, and always close the toilet lid before flushing to minimize the spread of bacteria onto your toothbrush.
Toothbrush holders as well can pick up bacteria that are spread by toilet flushing. A study by the National Sanitation Foundation (NSF) found that toothbrush holders are the third-most germy household items (behind dish sponges and kitchen sinks). Remember to clean your toothbrush holder regularly to remove germs.
After you've moved your toothbrush as far from the toilet as possible, and cleaned your toothbrush holder, here are some storage tips to keep your toothbrush as germ-free as possible:
Rinse your toothbrush thoroughly with tap water every time you use it.
Let your toothbrush dry thoroughly between brushings. Don't use toothbrush covers, which can create a moist enclosed breeding ground for bacteria.
Keep your toothbrush upright in a holder, rather than lying it down.
Don't ever use anyone else's toothbrush, or let someone use yours.
Keep toothbrushes separate. If toothbrushes touch, they can swap germs.
There are products available that claim to sanitize your toothbrush. Some use ultraviolet light; others are sprays or rinses. There are even brushes with built-in antibacterial bristles. While some of these products do kill some germs, there is no evidence using them will reduce your risk of illness.
The American Dental Association (ADA) states soaking your toothbrush in an antibacterial mouth rinse after use may reduce the number of bacteria on your toothbrush.
Just make sure you do not try to sterilize your toothbrush in a microwave or dishwasher. According to the ADA, most toothbrushes are not made to withstand these conditions and doing so might damage the brush and reduce its effectiveness.
The ADA recommends replacing your toothbrush every three to four months, or more often if bristles become frayed, if you are sick, or if you have a weakened immune system. For an electric toothbrush, replace the head as frequently as you would a regular disposable brush. Children's toothbrushes may need to be replaced more often than adult brushes.
Remember, "Bacteria cause gum disease, and decay, and bad breath," says dentist Kimberly Harms, DDS, consumer advisor for the ADA. Harms recommends brushing and flossing as often as possible, and rinsing your mouth with an antibacterial mouthwash before you brush to eliminate bacteria before they get onto your toothbrush.
(08/11/2024)by Medicinet
More Information: N
Views: 347
Sneaky Dental Issues That Might Mean Big Trouble
You know all about the importance of brushing your teeth, as well as your kids' teeth. But the benefits aren't limited to your pearly whites. "Many physicians and dentists consider the mouth to be a window into the general health of the patient," says Scott Froum, D.D.S., a board-certified periodontist based in New York City. Our experts Dr. Froum and Sally Cram, D.D.S., a dentist and spokesperson for the American Dental Association, broke down five tooth-, gum- and tongue-related issues that could mean you've got a much bigger problem on your hands:
1. Consistent bad breath
Aside from scaring away friends and family, your not-so-minty-fresh breath could be an early sign of gum disease, says Dr. Cram. Gum disease is particularly sneaky because it doesn't cause pain in its early stages, so most people who have it may not realize it until lots o' damage has already been done. Luckily, it doesn't involve some torturous procedure to reverse. Just put a little more time and effort into brushing and flossing daily.
2. Red, swollen or bleeding gums

If your gums continue to swell or bleed despite your best brushing and flossing efforts, our experts say there's a possibility you could be dealing with diabetes. So, if your pesky gum problems persist and you're noticing other diabetes symptoms like extreme thirst or hunger, fatigue or blurry vision, go see your doc ASAP.
3. Stubborn tongue pain
Obviously if you down hot soup too fast or bite your tongue it's going to be a little sore, but prolonged pain in the tongue or throat (more than two weeks) is one of the most common early signs of oral cancer, says Dr. Cram. Next steps: Monitor those symptoms and look out for any sores, lumps or lesions that won't disappear. Pass that two week mark and to the doctor you go.
4. Spots or sores out of the blue

If clusters of tiny white spots have started popping up around your lower molars — womp, womp — you might have a viral infection in your near future, Dr. Froum says. Called "Koplik spots," these little sores have developed a reputation as a highly predictive sign of measles. Tack on other symptoms like a fever, cough or runny nose, and you may be a few days away from that itchy measles rash. (Alas, you guessed it, a doctor's visit is required.)
5. Hefty tooth discoloration
As tempted as you might be to blame yellow teeth on your coffee addiction, you might be looking at the wrong culprit: If your teeth have turned a shade of black or brown, it could mean you're dealing with some deep-rooted tooth decay, Dr. Froum says. The solve: You might need to get a cavity filled — or (shudder) undergo a root canal treatment.
(08/03/2024)by Good Housekeeping
More Information: https://www.goodhousekeeping.com/health/wellness/a40559/common-dental-problems/
Views: 377
Common Problems In The Mouth That Adults Experience
Throughout your adult life, you will most likely suffer from at least one of the common problems in the mouth that we’re about to list. We’re not saying that it’s inevitable these will happen, but rather reporting on what has already happened to many adults – all of which require the expertise of your dentist to correct.
Chipped Teeth
You would believe that chipped teeth would be something akin to children who love to roughhouse and get into things they shouldn’t, but surprisingly chipping a tooth is a phenomenon that occurs most often in adults. Our chances of chipped teeth become greater with age. With age, we chew on more ice, more hard candies, etc. Also, our enamel isn’t as strong with age – despite being the strongest mineral in our bodies. If you chip a tooth, salvage the missing piece if you can, and bring it with you to an emergency dentistry appointment.
Stained Teeth

Over time, we expose ourselves more and more to common foods and drinks that are known to cause stains on our teeth such as wine, coffee, tea, soda, dark berries, spaghetti sauces, etc. No matter how many store bought teeth whitening trays your purchase, or whitening strips, the result will not be as fast and effective as teeth whitening performed by a professional dentist.
Amalgam Tattoo
While the American Dental Association has deemed amalgam as a safe solution for dental fillings, there are potential problems associated with them such as “amalgam tattoos”.You’ll notice these on the inside of your cheeks appearing as blue-grayish spots. They occur when a small piece of amalgam finds its way into the soft tissue of your mouth. They’re harmless, but you should consult your dentist on removing your amalgam fillings and replacing them with more advanced options.

Gum Disease – Experienced by Many Adults
Gum disease is the one of the main reasons dentists constantly nag you to brush and floss your teeth. When you don’t – you begin to enter the world of gum disease, which can be reversed in it’s early stages (known as gingivitis), but is non-reversible if it gets out of control. Many young adults are recommended to undergo deep cleaning procedures because they were not staying consistent with their routine. Listen to your dentist: brush and floss!
Many other common problems exist within our mouths as adults, but these seem to bear the most weight. Always make sure to visit your dentist every six months, not just for a routine cleaning, but for a chance to have a professional examine your mouth for any abnormalities. Dental exams are more important than you may realize.
(07/31/2024)by Sohrab Rahbar, DDS
More Information: https://www.dentistinirvine.com/blog/problems-in-the-mouth/
Views: 432
Top Four Embarrassing Oral Health Problems…Solved!
Stinky breath, unsightly mouth sores, and tooth decay: We’ve got a solution for all of your dental-health dilemmas.
The best way to keep your mouth, teeth, and gums looking and feeling great? Your daily brushing and flossing routine, combined with a balanced diet and regular dental visits.
But following these oral hygiene commandments isn’t always enough. Many common oral-health problems, such as bad breath, tooth decay, erosion, receding gums, and mouth sores, can leave people feeling both physically uncomfortable and reluctant to smile. Fortunately, with the right treatments these embarrassing oral-health problems can be solved! Check out these remedies from the American Dental Association (ADA):

1.- Bad Breath
Treatment for bad breath, or halitosis, varies depending on the cause. Brushing and flossing is crucial since it helps keep food particles from collecting bacteria and rotting in your mouth. If your dentist gives you a clean bill of health, though, you’ll need to investigate further.
Your bad breath could be the result of a medical disorder, such as a respiratory infection; chronic sinusitis or bronchitis; diabetes; a gastrointestinal disturbance, such as GERD; or a liver or kidney ailment. The use of particular medications can cause dry mouth, which can contribute to bad breath. And sometimes, the solution may be as simple as changing your diet: If you’re a garlic or onion lover, cutting down on these foods will help. So will cutting out tobacco if you’re a smoker.
2.- Tooth Decay and Erosion

Brushing twice a day with fluoride toothpaste, flossing once a day, and visiting your dentist regularly for exams and cleanings will help fight tooth decay and erosion. Your dentist may also recommend protective plastic sealants to reduce your risk of decay. Eating a balanced diet and keeping your snacking to a minimum will also help head off plaque and erosion. If you’re particularly concerned about erosion, avoid acidic food and drinks, such as citrus fruits and juices, tomatoes, pickles, soda, and sports drinks, since studies suggest that they can strip enamel from the teeth. Gastric acid can also contribute to erosion, so if you have a medical condition like acid-reflux disease or bulimia, getting treatment is imperative.
3.- Receding Gums
Gum recession and periodontal disease can have serious repercussions. Early stage gingivitis causes the gums to become red and swollen, and to bleed easily, while the more advanced periodontitis damages the gums and bones that support the teeth, causing them to loosen and fall out. The ADA recommends brushing, flossing, and keeping up with regular dental checkups and periodontal exams. Everyday Health’s dental expert, Dr. James E. Jacobs, adds that since gum recession can also result from aggressive tooth brushing with medium or hard bristles, malpositioned teeth, or bad habits such as clenching, grinding, or scratching your gums with foreign objects, you can also help protect your gums by using an ultrasoft toothbrush and wearing a nightguard to reduce stress on your teeth if you tend to clench or grind at night. Additionally, Dr. Jacobs recommends seeking professional dental, orthodontic, or periodontic help to get your bite comfortable, your teeth properly aligned, and if necessary, your gums grafted.
4.- Mouth Sores
Canker sores and cold sores are two of the most common sores that show up around the mouth. They can be painful, annoying, and unsightly. Cankers develop inside the mouth, while cold sores appear externally, usually on the edge of the lips. Fortunately, both of these types of sores tend to heal on their own within a week or so, and canker sores can be treated with over-the-counter topical anesthetics or antimicrobial mouth rinses to reduce discomfort. Topical anesthetics may also provide temporary relief for cold sores. If you’re embarrassed by frequent cold-sore outbreaks, talk to your doctor about getting a prescription for antiviral drugs that could help reduce infections from the herpes virus.
(07/13/2024)by Biermann Orthodontics
More Information: https://www.mcbiermann.com/top-5-embarrassing-oral-health-problems-solved/
Views: 305
Can You Dissolve Tartar?
Routine visits with your dental hygienist help keep your gums and teeth healthy. During cleaning appointments, one of the things your hygienist might do is remove tartar buildup from your teeth.
As you read on, we'll look into what tartar is, what role dental hygienists play, and what tools dental professionals use to handle tartar. We'll also answer the question: can you dissolve tartar?
What is Tartar?

Tartar (aka dental calculus) is plaque that builds up over time and hardens. But first, what is plaque?
Plaque is a sticky, colorless film that forms on your teeth. Plaque houses bacteria and secretes acids, which can cause tooth decay and irritate gum tissue.
If plaque is not removed regularly, the minerals in your saliva cause it to calcify and harden into a substance called tartar. The most prevalent areas where tartar builds are where the major salivary glands are located in the mouth: near the lower front teeth and in the cheeks next to the upper molars.
Brushing Your Teeth

Brushing your teeth won’t dissolve tartar, but it’s a great way to prevent it from happening in the first place. It helps to dislodge and remove plaque, preventing it from building up and hardening into tartar. But which is best: a classic toothbrush or an electric one?
Classic Toothbrushes or Powered Toothbrushes?
There is evidence that some powered toothbrushes can remove plaque more effectively than a classic manual toothbrush. However, when used properly, both types of toothbrush are successful at removing plaque and preventing tartar. The most important thing is to brush twice a day, for two minutes at a time, using a fluoride toothpaste.
Natural Ingredients to Dissolve Tartar
You may have come across natural solutions for dissolving tartar, but how do they work and are they effective? Let’s look at three of the most popular natural methods…
Aloe Vera
Aloe vera is packed with antioxidants and has lots of established wellbeing benefits, like anti-inflammatory and anti-bacterial properties. While studies do suggest that this can have a positive effect on your oral health, including plaque and tartar prevention, there is currently no evidence to suggest that aloe vera can dissolve tartar.
Orange Peels
Fans of orange peel suggest that rubbing the white inner part on your teeth can help to dissolve tartar. Like aloe vera, the antioxidants and other nutrients in orange peel may have an antibacterial effect in the mouth, which can theoretically help to prevent tartar build-up. However, orange peels will not help to dissolve tartar that has already built up on your teeth.
Coconut Oil
Coconut oil has been having a big moment in health and wellbeing lately! You may have heard of coconut oil pulling, a method of swilling and swishing coconut oil around the gums and teeth for around 20 minutes. And while it doesn’t dissolve tartar that has actually built up on the teeth, there is some evidence to show that coconut oil can reduce harmful plaque bacteria. However, it’s worth noting that the American Dental Association (ADA) is not yet convinced of its effectiveness.
It’s tempting to look for natural solutions to oral healthcare problems such as tartar, and there certainly may be preventative benefits to some of these options. However, nothing can replace the expert intervention of a qualified dental professional, especially if tartar has already built up on your teeth. So if you’re concerned about tartar, the best thing to do is check in with your dental hygienist.
Hygienists: Your Tartar Experts
A dental hygienist's role in dentistry is diverse and can vary from state to state. However, one universal part of that role is removing hard and soft deposits on the teeth.
The detection and removal of tartar is critical for maintaining optimum periodontal (gum) health and preventing gum disease. And so, a hygienist's role is essential in your overall oral health care.
Tools of the Trade
Tartar is challenging to remove. So how do the professionals do it? Great question. Here are some tools of the trade that help them keep your teeth healthy and tartar-free:
Hand instruments: You've probably seen your dental hygienist scrape off tartar with fine-tipped metal tools using a technique known as scaling. These tools are classic and effective.
Ultrasonic instruments: This technology uses a high-powered oscillating tip to remove buildup with micro-vibrations.
Perioscopy: This extremely tiny scope can probe into small areas between gums and teeth to examine calculus build-up on the roots of the teeth.
A friendly heads-up! Your dental hygienist has spent years training to remove tartar and perform other procedures. Attempting to use sharp tools in your own mouth can result in injuries to your teeth and gums, so always look to a professional for this type of care.
It's a Wash for Anti-Tartar Rinses
It would be nice to be able to wash tartar away, wouldn't it? The truth is the jury is still out on the effectiveness of tartar removal rinses. One study compared chlorhexidine — an antimicrobial mouth rinse widely used in dentistry — and a commercial anti-calculus mouth rinse. The study found that there was 47 % more new calculus and 10% more new plaque formed when using the antimicrobial mouth rinse versus the anti-calculus rinse.
Another study tested the effectiveness of an anti-tartar rinse by soaking calculus samples “in vitro”, or in a laboratory setting. Some of the mineral content of the tartar was dissolved in the rinse, but only after it had been soaking for 4.5 and 16 hours. This study was not conducted on a human mouth, and of course, no one wants to swish mouthwash for that long!
So, what would your hygienist say about dissolving your tartar? Well, as dental professionals do, they'll go with the research. If a mouthwash arises that research shows as a great option for dissolving tartar, they'll be all for it.
Until then, if you're wondering how to reduce the amount of tartar that forms on your teeth, the best thing you can do is to reduce or prevent plaque and calculus build-up in the first place. You can do this with proper home oral care and regular dental check-ups and professional cleanings. Brushing at least twice a day and flossing daily will go far in reducing the need to look for ways to remove tartar.
Plaque control directly relates to tartar prevention and is known to prevent cavities, gingivitis, and gum disease. That's why one of the things every hygienist does is to help you remove it. Remember that your dental hygienist is trained to use tools to help you remove your tartar and that trying to use sharp instruments in your mouth is dangerous.
Good oral hygiene and regular dental visits are, and will continue to be, the best treatment. If tartar is something on your radar, see your hygienist and get proactive in taking care of it right away.
(06/06/2024)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/plaque-and-tartar/can-you-dissolve-tartar--what-would-your-dental-hygienist-think
Views: 301
Signs You Have the Best Dentist
Getting into a dental school is not necessarily that hard, however, only the choicest ones have what it takes to be a great dentist. It takes a little more than having great knowledge or expertise on treatments such as removing stubborn wisdom teeth in Blacktown or having amazing manual dexterity. There are a few other traits that are important for a competent dentist to have.
Some of the patients find bedside manner, a clean and welcoming ambiance, and a sorted appointment system important while considering the medical doctors we choose to go to. With so many dentists to choose from, there is no possibly easy way to know if we have chosen the right one. Therefore, we are trying to make it easier for you with extensive guidelines about what makes a quality dentist while opting for your current care provider or deciding if you need a new one. If you’re wondering whether or not yours is top of the line, we believe these are ten qualities that make a good dentist:
#1. Actively Listens to You
A good dentist intends to help you, but the best ones utilize their skills as much as use their technical knowledge and wisdom. A great doctor lends his ears to listen to all your concerns, never rushes with the treatment, and will pay heed to solve any concern that might lead you to make uncomfortable, like if you have dental anxiety or fear for any procedure and so on.
#2. Educates You

Let’s get this right, you didn’t go to a dental school, they did. so, you are dependent on them to educate you on your oral health conditions, good dental care habits, and the available options to treat your issues. An ideal dentist is usually interested in taking some time out to explain these to you to be able to work on what is convenient for toy and enhance your confidence. This could range from teaching you how to brush your teeth properly to explaining and discussing the step by step of the potential procedure you might require.
#3. Respects Your Time and Resources
Ideal and thoughtful dentists are usually punctual and respect your time as well as their own when suggesting treatment or while scheduling an appointment. They have staff members who are responsible for calling and leaving you a message reminding you of an upcoming appointment and also helping you schedule your other future appointments with enough time for you to plan.
#4. Keeps a Clean Office

The American Dental Association (ADA) recommends checking to ensure that your dentist’s office is “clean, neat, and orderly”, and that all dental instruments are thoroughly sterilized. If you happen to notice things like old gloves and dirty or rusty instruments in the dental operatory, your dentist could be contaminating the examination room, which might lead to the spreading of germs and can make you and other patients sick.
#5. Only Promotes What Is Necessary
The ideal dentist won’t try to upsell you on products and treatments that you might not necessarily need or didn’t ask for before signing up for the examination. A competent dentist will also have a team that is meant to help you figure out what your dental insurance could partially or fully cover for procedures, products, or devices that you might want to have or you might need.
#6. Gets to Know You
When a dentist invests some additional time in getting to know you and your routine better, it becomes easier for them to provide you with better and more convenient care options that will be appropriate to your regimen and medical history. They will also be able to assist with the underlying issues that could go undiagnosed in a hurried impersonal visit. However, it is not be confused with flirting. When your dentist greets you warmly and asks about your family or work, you may be thinking these are signs your dentist likes you. They’re also just indications that you have a quality dentist who cares about you and cares about your comfort during your dental appointment.
#7. Values a Long-Term Relationship
A good dentist invests in keeping you for the long term. This means following up when it is time for the next appointment, scheduling regular screenings or X-rays, and making you and your family members when you are in their office. If your dentist treats you like a one-time thing or a job, it might your cue to look for another dentist.
#8. Cares About Their Staff
If you happen to work in an office, it might be a slightly funny concept for you to think of your dentist as a boss, managing his staff. It is worth observing the existing hierarchy among the staff and how your dentist interacts with his colleagues. It is going to give you an idea of their management style, the mood of the team who would be working with you, and the kind of manners your dentist has as a person. It is a good sign to see a dentist treating their staff with kindness and passion because it speaks a lot about their nature and their professional ethics as a whole.
#9. Follows Up with You
Some dental procedures can be complicated and can tend to be long and arduous, leaving you feeling restless and uncomfortable for a few hours afterward. The best ones will always find it necessary to follow up with you after a long or strenuous procedure to ensure you are improving or feeling better as expected and that no complication or issue comes in the way of your process of recovery.
#10. Values You as a Patient
Most professional dentists have a special language for their patients to know that they care for them. Whether it is the time and space that they give you to clarify your doubts, their thorough assessment at the routine check-ups, or explaining to you the different options for a procedure that you might require, your dental health expert can express their care and concern for their patients and their job in many professional ways.
Your relationship with your dentist is very personal and choosing the correct professional can be very overwhelming. They are meant to see you as a patient for life and not once or twice. The best ones always give you the care and compassion that you and your family needs and deserve. If your dentist missing some of the qualities that we have enlisted below it might be your cue to look for a new and better dentist.
(05/31/2024)by Smilecraft Dental Group
More Information: https://www.smilecraftdental.com/10-signs-you-have-the-best-dentist/
Views: 346
How Snacking Can Affect Your Teeth
Have you ever wondered what general dentistry professionals think about how snacking affects your dental health? Snacking in between meals is a great way to refuel your body and keep you going until your next meal.
However, many people substitute snacks for meals, which can be bad for your teeth. In general dentistry, there is a belief that frequent snacking does as much damage to your teeth as eating candy or drinking sodas.
Why is snacking so bad for your teeth?
For general dentistry practitioners, snacking is considered to be bad for your teeth because anytime you snack on sugary or starchy foods, the sugar and starch combined with the bacteria in your mouth to form acids that wear down your enamel.

When your enamel is weakened, the structure of your teeth becomes compromised, leading to tiny holes known as cavities, a form of tooth decay. If the cavities in your teeth are left unchecked, they can lead to further tooth decay and, eventually, tooth loss.
What should I do if I cannot snack?
Even though snacking can be bad for your health, you can still enjoy some of your favorite snacks as long as you do so in moderation. If you want to protect your teeth, you will also have to practice good oral hygiene.

The American Dental Association recommends brushing your teeth at least twice a day and flossing regularly. Ideally, general dentistry practitioners would prefer it if you brushed your teeth after every meal but that is not very practical, especially if you snack a lot.
The best way to protect your teeth after snacking is to rinse with either fluoride mouthwash or tap water because most of the tap water in the country has fluoride in it.
Limiting your snacking
There are plenty of ways to reduce the amount of snacking you do each day, helping to protect your teeth. Some of the most popular techniques used to reduce snacking in general dentistry include:
Eating breakfast: It is said that breakfast is the most important meal of the day, but a lot of people skip breakfast, opting for alternatives to snack on. If you eat a big meal for breakfast every day, your body gets fueled and your appetite is curbed, meaning you are likely to eat fewer snacks
Drink water: Drinking water helps to hydrate your body and helps you feel less fatigued. Water is also a better alternative to any soda or sugary drink because it does not damage your teeth as sugary drinks do
Eat less sugar: If you want to eat a snack, try avoiding sugary snacks and processed foods
Have a healthy diet: A balanced diet is very important to your general and oral health, which is why you should eat a lot of healthy food, fruits and vegetables to help you maintain a balance
Conclusion
Snacking is bad for your teeth because many snacks have plenty of sugar and carbohydrates. If you want to learn more about the negative effects of snacking on your teeth, talk to your dentist to understand how snacking affects your teeth.
(05/16/2024)by Rowley Family Dental Center
More Information: https://coastalsmiles.com.au/how-snacking-can-affect-your-teeth/
Views: 398
Does A Sensitive Tooth Mean A Cavity?
A small amount of dental sensitivity should not sound the alarms. In fact, it is considered normal. But, if tooth pain keeps you from eating ice cream or enjoying your morning coffee, then it’s time to speak with your dentist. This pain could be attributed to severe sensitivity or a number of other dental issues (that can all be treated).
Causes of Tooth Sensitivity
Tooth sensitivity, according to the American Dental Association, is caused by tooth decay, a cracked tooth, worn tooth enamel, worn fillings, and tooth roots that are exposed as a result of aggressive tooth brushing, gum recession, or periodontal (gum) disease. In a report published by the U.S. National Library of Medicine, “One in eight participants from general practices had dentin hypersensitivity, which was a chronic condition causing intermittent, low-level pain. Patients with hypersensitivity were more likely to be younger, to be female, and to have a high prevalence of gingival recession and at-home tooth whitening.”
But what is the difference between cavity pain and sensitivity?

Dentin is one of the four major components of teeth. It is a tissue within the tooth that is protected by hard enamel (the strongest substance in the body) at the top of the tooth and cementum on the root. A major characteristic of dentin is that it can be sensitive because of the microscopic tubules that connect it to the pulp of the tooth. The pulp houses a tooth’s nerves.
Therefore, if dentin loses its protective armor (enamel and cementum), sensitivity to hot, cold, acidic, and sweet foods could develop because the nerves connected to the dentin are exposed and triggered. Causes of dentin exposure are teeth grinding, gum recession, brushing too hard, and even heartburn.
Cavities are different in that they occur when there is a hole in your enamel, allowing bacteria to enter. Cavities must be professionally treated by a dentist to prevent further decay. Sign and symptoms of a cavity include:

Holes or pits in the tooth
White, black, or brown stains on the tooth surface
Pain when eating or drinking hot, cold, or sugary foods
Pain when biting
Pain occurring spontaneously
The biggest difference between pain associated with sensitivity and that of a cavity is the latter is often classified as a dull ache rather than sharp pain with sensitivity. Moreover, pain from a cavity won’t necessarily stop after eating or drinking.
In short, sensitivity does not necessarily mean that you have a cavity. And, luckily, sensitivity can be treated with at-home products or in-office treatment. It’s important to speak to your dentist if you have regular sensitivity or dull, aching pain in your mouth. There are ways to treat the discomfort if either is the case!
(05/16/2024)by Ideal Dental
More Information: https://www.myidealdental.com/blog/does-a-sensitive-tooth-mean-a-cavity/
Views: 341
Is It Necessary To Sanitise Your Toothbrush?
Since our mouths contain bacteria and the bathroom does as well, it's common to wonder if your toothbrush stays clean enough with just a rinse after brushing, especially since some products now claim to sanitise. Toothbrush sanitising, however, is not the same as sterilising. Sanitation means 99.9 percent of bacteria are reduced. With sterilisation, all living organisms are destroyed. But is a sanitising of your toothbrush a necessity or a preference?
What the American Dental Association Recommends
According to the American Dental Association, no commercial products can sterilise a toothbrush and it's not necessary. The ADA notes, "There is insufficient clinical evidence to support that bacterial growth on toothbrushes will lead to specific adverse oral or systemic health effects."
Bacteria tends to grow in dark, warm and moist places. Keeping your toothbrush covered or stored in a closed container might lead to problems. Let your toothbrush air dry in a holder that allows it to stand up without touching the bristles or other toothbrushes. Replacing your toothbrush every three-to-four months is also important. Avoid sharing toothbrushes as well.

Keeping it Clean
Most of us simply rinse the toothbrush head once we're done brushing. But a more thorough rinse in warm water ensures that food debris and leftover toothpaste won't remain in the bristles.
The Maryland Children's Oral Health Institute suggests that you may disinfect your toothbrush by allowing it to soak in an antibacterial mouthwash. If you want to sanitise, toothbrush heads should be immersed for about 15 minutes in mouthwash. Any longer could damage the bristles. And don't share or reuse that mouthwash, it defeats the purpose.
According to the ADA a study indicates that soaking a toothbrush in 3 percent hydrogen peroxide or Listerine mouthwash greatly reduces (i.e., 85 percent) bacterial load, while microwaving or putting toothbrushes in the dishwasher is not recommended as such high heat may damage the brush.

Some Exceptions
If someone in your family is sick or is at a higher risk of infection, taking some preventive steps may help guard against a problem. Replacing toothbrushes more often, buying disposable toothbrushes and using antibacterial mouthwash to rinse and soak could offer some benefit. If you choose to try a UV toothbrush sanitiser, the product should be approved by the Food and Drug Administration. Keep in mind that a UV sanitiser will not remove all germs. Because the ultraviolet light may deteriorate the bristles, you should inspect and replace your toothbrush more often.
(05/14/2024)by Colgate
More Information: https://www.colgate.com/en-in/oral-health/brushing-and-flossing/is-it-necessary-to-sanitize-your-toothbrush-0513
Views: 401
Chronic Bad Breath? You May Need to Visit the Dentist
Embarrassed by chronic bad breath? Breath fresheners can be an effective short-term fix.
But if bad breath persists despite a regular brushing and flossing regimen, it’s best to see your dentist for an exam.
What Causes Bad Breath?
Bad breath, or halitosis, is an embarrassing problem that could signify a more serious medical issue, especially if you’re already practicing good oral hygiene.

The tongue harbors many bacteria, which are normally kept in check by saliva. However, an excess of bacteria can form plaque on your teeth and gums—producing plaque and volatile sulfur compounds that cause bad breath.
Risk factors for bad breath include:
Smoking or chewing tobacco
Poor oral hygiene

Dry mouth due to medications
Gingivitis or periodontal disease
Medications that interfere with saliva production (antidepressants and antihistamines are common offenders)
High-protein diet
Good Oral Health is Essential for Overall Health
Maintaining good oral health is essential for overall wellness.
Teeth and gums are vulnerable to decay, periodontal (gum) disease, tooth loss, and oral cancers. You can prevent many problems with regular visits to your dentist for exams, cleaning, and x-rays.
The American Dental Association recommends these steps for good oral health:
Brush your teeth twice a day with fluoride toothpaste. Use an ADA-approved soft-bristled brush. Floss once a day unless your dentist tells you otherwise.
If you have gingivitis or periodontal disease, floss at least once a day and brush after meals whenever possible.
Visit your dentist regularly—at least twice a year—for checkups and professional cleanings. You may need professional cleanings more often If you have problems with your gums or periodontal disease.
If you use tobacco products, stop. Smoking increases the risk of developing oral cancer and causes bad breath, stained teeth, and mouth sores.
If you drink alcohol, do so in moderation (no more than one drink per day). Excessive alcohol consumption can damage the tissues of the mouth.
Common Signs of Dental Problems
Many people don't realize that their oral health is an important factor in maintaining overall health. A healthy mouth can help prevent severe conditions such as heart disease, stroke, and cancer—not to mention periodontal disease that can lead to tooth loss.
Some signs of dental problems are obvious, such as bad breath or pain when chewing.
These are common signs of dental problems:
Bleeding gums. Bleeding may be a sign of gum disease caused by plaque. Left untreated, gum disease will worsen and may eventually lead to tooth loss and other problems.
Swollen or discolored gums. If you notice any changes in your gums, see your dentist. Changes in gum tissue may indicate a more serious problem.
Bad breath (halitosis). Bad breath can occur when your teeth decay or become infected. Halitosis can be eliminated with proper treatment for any dental problems.
Tooth pain or sensitivity. See your dentist if you’re experiencing persistent tooth sensitivity or toothaches.
Embarrassed By Bad Breath? Schedule an Appointment Today
Good oral hygiene can help prevent embarrassing bad breath, but you should see your dentist if the problem persists.
A dental cleaning removes plaque and reduces your chances of developing cavities and gum disease that can lead to bad breath. Routine dental exams are the best way to protect your smile.
(05/06/2024)by Dr Todd Paczewski
More Information: https://www.drtoddsmileon.com/chronic-bad-breath-you-may-need-to-visit-the-dentist/
Views: 357
Wisdom Teeth Are Usually Problematic
Wisdom teeth, are the third set of molars that emerge between the ages of 17 and 25 and usually become problematic – even for those who have the best oral health. These teeth are supposed to grow in just behind the other molars, but that doesn’t always happen. Often, the wisdom teeth don’t erupt through the gums at all and become impacted. This usually happens because the jaw is too small to fit four extra teeth.
Dr. Shane S. Porter of Premier Dental of Eagle cites four problems related to wisdom teeth:
Decay and Wisdom Teeth
Wisdom teeth that only partially erupt through the gums are difficult to clean and are more at risk for decay. It’s important to practice good dental hygiene at home and keep regular cleaning appointments to prevent decay. Impacted wisdom teeth often become decayed or infected because they’re hard to reach with your toothbrush. Fluid-filled cysts or tumors occasionally form around the bottom of an impacted wisdom tooth, causing damage to the jawbone, in the nerves in the area and nearby teeth.

Damage to Nearby Teeth
Wisdom teeth often grow at odd angles, pushing into adjacent molars and causing crowding and misalignment. It’s not unusual for wisdom teeth to be positioned crooked or sideways in the jaw, keeping them from erupting into the mouth properly. Infection can be the result. Healthy teeth can be damaged as impacted wisdom teeth push against the neighboring second molars.
Risk of Gum Disease
Any part of the mouth that is hard to keep clean is a breeding ground for bacteria that causes gum disease. With wisdom teeth sitting at the very back of the mouth, they are difficult to reach. Bacteria around the impacted tooth can lead to gum disease and enter your bloodstream, adversely affecting your heart and other organs of your body.

Symptoms of Infection
Impacted wisdom teeth can become infected. Signs of such an infection include red or swollen gums, jaw pain, swelling around the jaw and difficulty opening the mouth. Dr. Porter should be consulted promptly if these symptoms are present.
How Will I Know if I Should Have My Wisdom Teeth Removed?
Dr. Porter has performed over ten thousand successful wisdom teeth removal procedures during his dental career, and he considers it his best skill. Dental x-rays will reveal whether wisdom teeth will be a problem as you enter adulthood. If you are concerned about your wisdom teeth, consult with Dr. Porter about the advisability of having them removed.
The Best Time to Remove My Wisdom Teeth
When Dr. Porter detects problems or feels that your wisdom teeth have the potential to create complications in your mouth, he will most likely suggest that you have one or all of your wisdom teeth removed – even if they aren’t causing you problems at the moment. When wisdom teeth cause problems, removing them is the “wisest” thing to do. According to the American Dental Association (ADA) wisdom teeth are also easier to remove when you’re younger, because the roots are not completely developed and the bones around the teeth aren’t as dense. This means there is a slimmer chance of damaging surrounding nerves, teeth or bone during removal.
What Does the Procedure Entail?
At Premier Dentistry of Eagle, we provide an environment of safety and comfort for all our services with Dr. Porter at the helm. We utilize state-of-the-art technology and have a highly trained team to monitor the administration of anesthesia. Most wisdom teeth removal can be performed using a local anesthesia, oral sedation, nitrous oxide (laughing gas), IV sedation, or general anesthesia. Dr. Porter will discuss your sedation options with you prior to your procedure. After your wisdom teeth are removed, you will rest in our office for a short time until you are fully awake and steady. When you are discharged, you will need to have someone drive you home and we will send you with a postoperative kit to care for your mouth; consisting of care instructions; antibiotics, gauze and a prescription for any necessary pain medication.
What is the Recovery Process Like After Surgery?
After surgery, bruising, swelling and tenderness in the face and neck are common. Ice packs and pain medications should help ease the pain. A certain amount of bleeding can be expected following surgery and you will need to restrict your activities the day of surgery. In most cases, you can resume normal activity the next day, or when you feel comfortable.
You will be required to eat soft foods for up to a week following your oral surgery. What to Eat After Wisdom Teeth Removal Foods such as yogurt, scrambled eggs, mashed potatoes, pudding, ice cream, cottage cheese, applesauce and fruit smoothies are a sampling of the foods to plan on. Five to six glasses of milk, water or juice will prevent dehydration, and you will be restricted from drinking through a straw for at least 24 hours. The sucking action required for using a straw has the potential to unseat the blood clot that forms in the tooth socket and it will make you more susceptible to a dry socket. The socket is the hole in the bone where the tooth has been removed. After a tooth is pulled, a blood clot forms in the socket to protect the bone and nerves underneath. If that clot is dislodged too soon, it can leave the bone and nerve exposed to air, food, fluid, and anything else that enters the mouth, and it can lead to infection and severe pain that lasts for several days.
(04/25/2024)by Premier Dentistry Of Eagle
More Information: https://www.premierdentistryofeagle.com/wisdom-teeth-are-usually-problematic/
Views: 243
Why Can I See My Teeth Through My Gums?
If you have recently asked why can I see my teeth through my gums, you should book yourself an appointment with a dentist. Changes or abnormalities in your gums can be a sign of periodontal disease, which needs to be treated as soon as possible. Ignoring it could be an incredibly risky option.
In this article, you will find information on what can cause gum health to deteriorate and reveal your tooth root together with symptoms of gum disease. Ensure you see your dentist if you have gum issues or it may lead to tooth loss, affect the bone in your jaw, or cause other health complications.
The Appearance of Healthy Gums Versus Unhealthy Gums
When your teeth and gums are healthy, there will be about three mm between your gums and teeth. In people who have gum disease, the gums have often pulled away from the teeth and exposed the roots of the teeth.
When the gum has receded, you will notice a wider gap between the gum and the tooth. As well as the periodontal pocket between the tooth and gum, you are also likely to see more of the tooth than before, making your teeth look bigger.
Symptoms of Exposed Roots

Gum recession is usually very gradual and by the time you notice it, the gum disease may already have caused significant damage. Therefore, it is important to know the symptoms that may indicate you have an exposed tooth root.
Bleeding Gums
Often the first and most noticeable sign of trouble is bleeding during brushing or flossing. If you discover blood when you spit out the toothpaste or after flossing, it may be a sign of a serious inflammation of the gingival tissues.
Swelling

If you have exposed roots, you may notice that your gum tissue is swollen in a particular area of the mouth. This can be caused by the inflammation of the tissue in the gums. They may also look red rather than pink. Swollen gums are also likely to cause irritation or pain, especially during brushing and flossing or when you bite into food.
Tooth Sensitivity
Another early sign of issues with your gums is sensitive teeth. Your teeth may be sensitive when you brush them or you might notice it when you are eating or drinking hot and cold food and beverages.
Bad-Smelling Breath
If you have a bacterial infection or inflamed tissue in your gums, you may notice a bad smell when you are cleaning your teeth. The bacteria can also travel from the gums to elsewhere in your body and cause bad-smelling breath.
Periodontal Disease
If receding gums expose the roots, it may lead to chronic periodontitis, which is the most common form of periodontitis where the periodontal membrane of the teeth is inflamed. It can also affect the periodontal ligaments, which are a group of tissue fibers helping to attach the teeth to the bone.
Severe cases may cause lesions on the face caused by the necrosis of gingival tissues, alveolar bone, and periodontal ligaments. It may also cause a periapical cyst to form, which is a pathological cavity that often contains soft matter or fluid and has epithelium in the lining.
Why Do Gums Pull Away From Your Teeth?
Not taking proper care of their teeth can lead to exposed roots. Without regular brushing and flossing, plaque will build up on the teeth. Over time, it will harden and become tartar and push gums away from the teeth.
Gingivitis
Gum Recession caused by gingivitis is the most common reason for root exposure. Gingivitis is caused by tartar buildup. If the condition is not addressed, it may develop into periodontal disease, more commonly called gum disease.
Do not delay contacting your dentist when you have gum recession. Your dentist will ensure you get proper treatment for the infection before you lose any teeth. They will also be able to advise how to look after your gums properly to avoid further gum recession.
Oral Injury
The recession can also be caused by an outside force. If you have hurt your mouth, for example, as a result of a fall, this type of dental trauma can lead to exposed roots. Your dentist will know how to treat the result of that injury and prevent further damage.
Sometimes your gum might recede on one side of your mouth only. This can be the result of abnormal wear patterns or if the gum has a severe abrasion like a scratch from your nail. For the majority of people, the latter is likely to heal on its own but when it does not, visit your dentist.
Misalignment
If your teeth are not in the correct alignment, it may expose the roots and place additional strain on your teeth. Misalignment can be a result of, for example, an adult tooth growing in before a baby tooth has fallen out or teeth shifting into a potential area of space if you have lost a tooth.
A Medical Condition
Some medical conditions, such as sickle cell anemia, diabetes, and lupus will increase the risk of gum disease and gum recession. These conditions can weaken the immune system, meaning you can get diseases more easily. Oral cancer can also cause your gums to recede and requires immediate care.
Medications
There are some medications, such as antibiotic treatment or chemotherapy that can make you more susceptible to gum problems and tooth decay. If the problems are not treated, they may progress to periodontal disease or gingivitis.
Oral Surgery
If you have had surgery on your mouth, it can increase the likelihood of gum disease. Looking after your oral health following periodontal surgery can aid recovery and prevent gum disease. Your dental surgeon will be able to advise you on how to best look after your teeth and gums.
Aging
While patients of all ages can get receding gums, aging can also cause gum recession. With age, the muscle structure in your gums changes, which can lead to receding gums and teeth becoming looser. If not addressed, it is likely to lead to tooth loss.
Dental Cleaning
If the gum recession is caught early, a deep cleaning procedure may be enough to treat it. Dental cleaning involves the removal of dental plaque from areas you may not be able to reach home. Your dentist may also apply fluoride to your teeth to protect them. A professional cleaning will also give you a fresh clean feel.
Root Canal Treatment
If the condition has progressed too far to be treated by dental cleaning, your dentist may suggest root canal therapy. This non-surgical therapy is used to relieve pain caused by dental infections. During the process, the dentist will remove the inflamed pulp from your tooth and clean and disinfect the surfaces of the tooth.
Gum Graft
Sometimes gum recession can be treated by gum graft, which is a surgery where gum tissue that has been lost is replaced. This will add more volume to the gum line and improve your oral health.
Gum graft restorations have an excellent success rate and can help save your natural teeth. It can also be a protective measure for people who are more at risk of gum disease. Sometimes, laser procedures can be used as an alternative to gum grafts to stimulate gum growth.
Tooth Extraction
The treatment of extreme levels of periodontal disease may require tooth extraction. You will have dental surgery to remove the tooth. Following tooth extraction, you may choose to get a dental implant, which goes into the jawbone and holds a false tooth firmly in place.
Your best chance of preventing exposed roots is to establish an oral hygiene routine as part of a healthy lifestyle that includes brushing your teeth twice a day. You should also floss your teeth once a day.
For brushing, use a medium or soft toothbrush rather than a hard toothbrush because too hard brushing can also cause gum recession over time. Using an electronic toothbrush can help you apply the correct pressure when brushing.
Visit your dentist regularly. The American Dental Association (ADA) recommends that everyone should see a dentist at least once a year. For some people, it may be twice a year, depending on the health of your teeth.
Do not skip appointments as they help catch issues early. Early diagnosis means less invasive methods are required to address the issue.
(04/23/2024)by CDHP Dental Health
More Information: N
Views: 359
Top Four Embarrassing Oral Health Problems…Solved!
Stinky breath, unsightly mouth sores, and tooth decay: We’ve got a solution for all of your dental-health dilemmas.
The best way to keep your mouth, teeth, and gums looking and feeling great? Your daily brushing and flossing routine, combined with a balanced diet and regular dental visits.
But following these oral hygiene commandments isn’t always enough. Many common oral-health problems, such as bad breath, tooth decay, erosion, receding gums, and mouth sores, can leave people feeling both physically uncomfortable and reluctant to smile. Fortunately, with the right treatments these embarrassing oral-health problems can be solved! Check out these remedies from the American Dental Association (ADA):

1.- Bad Breath
Treatment for bad breath, or halitosis, varies depending on the cause. Brushing and flossing is crucial since it helps keep food particles from collecting bacteria and rotting in your mouth. If your dentist gives you a clean bill of health, though, you’ll need to investigate further.
Your bad breath could be the result of a medical disorder, such as a respiratory infection; chronic sinusitis or bronchitis; diabetes; a gastrointestinal disturbance, such as GERD; or a liver or kidney ailment. The use of particular medications can cause dry mouth, which can contribute to bad breath. And sometimes, the solution may be as simple as changing your diet: If you’re a garlic or onion lover, cutting down on these foods will help. So will cutting out tobacco if you’re a smoker.
2.-Tooth Decay and Erosion

Brushing twice a day with fluoride toothpaste, flossing once a day, and visiting your dentist regularly for exams and cleanings will help fight tooth decay and erosion. Your dentist may also recommend protective plastic sealants to reduce your risk of decay. Eating a balanced diet and keeping your snacking to a minimum will also help head off plaque and erosion. If you’re particularly concerned about erosion, avoid acidic food and drinks, such as citrus fruits and juices, tomatoes, pickles, soda, and sports drinks, since studies suggest that they can strip enamel from the teeth. Gastric acid can also contribute to erosion, so if you have a medical condition like acid-reflux disease or bulimia, getting treatment is imperative.
3.- Receding Gums
Gum recession and periodontal disease can have serious repercussions. Early stage gingivitis causes the gums to become red and swollen, and to bleed easily, while the more advanced periodontitis damages the gums and bones that support the teeth, causing them to loosen and fall out. The ADA recommends brushing, flossing, and keeping up with regular dental checkups and periodontal exams. Everyday Health’s dental expert, Dr. James E. Jacobs, adds that since gum recession can also result from aggressive tooth brushing with medium or hard bristles, malpositioned teeth, or bad habits such as clenching, grinding, or scratching your gums with foreign objects, you can also help protect your gums by using an ultrasoft toothbrush and wearing a nightguard to reduce stress on your teeth if you tend to clench or grind at night. Additionally, Dr. Jacobs recommends seeking professional dental, orthodontic, or periodontic help to get your bite comfortable, your teeth properly aligned, and if necessary, your gums grafted.
4.- Mouth Sores
Canker sores and cold sores are two of the most common sores that show up around the mouth. They can be painful, annoying, and unsightly. Cankers develop inside the mouth, while cold sores appear externally, usually on the edge of the lips. Fortunately, both of these types of sores tend to heal on their own within a week or so, and canker sores can be treated with over-the-counter topical anesthetics or antimicrobial mouth rinses to reduce discomfort. Topical anesthetics may also provide temporary relief for cold sores. If you’re embarrassed by frequent cold-sore outbreaks, talk to your doctor about getting a prescription for antiviral drugs that could help reduce infections from the herpes virus.
(04/20/2024)by Biermann Orthodontics
More Information: https://www.mcbiermann.com/top-5-embarrassing-oral-health-problems-solved/
Views: 341
Is Sparkling Water Bad For Your Teeth?
We all have our favorite brands and flavors. It's crisp, refreshing, and zero calories. And that makes us feel good about our beverage choice. We're talking about sparkling water, of course! It's popularity right now is massively escalating, according to USA Today. But how does it affect your pearly whites? Is sparkling water bad for your teeth? We've got all the sparling water answers you need.
How Does Soda Affect Your Teeth?
If you asked your dentist for their thoughts on soda, they'd recommend avoiding it. Why? Two big reasons:
Sugar — soda has an abundance of it, leading to tooth decay and cavities

Acid — most sodas are highly acidic, contributing to tooth erosion
So now you know what not to drink. Some healthier alternatives to drink include water, milk, and you guessed it — unsweetened sparkling water.
What Are Sparkling Water's Effects on Your Teeth?
That fizzy refreshment in your sparkling water, it's caused by carbonation. And it's the carbonation that has some concerned. So is carbonated water bad for your teeth? A Journal of the American Dental Association study found that many popular sports drinks were "extremely erosive," while most sparkling carbonated waters ranked as "minimally erosive." So does minimally erosive equate to "bad"?

Sparkling water is much less erosive than other beverages. Which is good — so it's not bad for you. "For an average, healthy person, carbonated, sugar-free beverages are not going to be a main cavity-causing factor," according to the U.S. News & World Report article. However, it's not necessarily good for you. It's great to replace soda with sparkling water, but don't replace water with fluoride over its sparkling counterpart.
What Are Some Other Ways to Protect Your Teeth?
To battles against cavities and enamel erosion, there are a few things you can do.
Brush with specially formulated toothpaste to help strengthen tooth enamel, replenish natural calcium, and protect against tooth sensitivity
See your dentist regularly to detect signs of tooth decay early when it is easy to correct or reverse
Now you know the truth about sparkling water — it isn't bad for your teeth. You also understand what's needed to keep your teeth healthy while you enjoy something fizzy.
(04/16/2024)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/tooth-sensitivity/is-sparkling-water-bad-for-your-teeth
Views: 486
Five Ways To Improve Your Dental Hygiene Routine
According to the Centers for Disease Control and Prevention, approximately 31% of US adults aged 20-44 have untreated dental cavities. The prevalence of tooth decay and gum disease is largely due to poor oral hygiene practices.
Oral hygiene, which includes daily brushing and flossing, is absolutely essential for preserving your smile and minimizing your risk for dental problems. Neglecting either of these aspects, even for a short period of time, can have serious consequences to dental health and the appearance of your smile.
In celebration of National Dental Hygiene Month, we’d like to encourage our Kingston patients to take a critical look at their oral hygiene routine and consider different ways they can improve dental care.
IS YOUR ORAL HYGIENE ROUTINE UP TO PAR?

Improving your dental hygiene should be specific to your smile and individual concerns. However, generally speaking, many patients can benefit from the following tips:
Switch Out Your Toothbrush: When was the last time you switched out your toothbrush? According to the American Dental Association, it’s best to switch out your toothbrush or toothbrush head every 3-4 months. As the toothbrush begins to wear, the bristles can become frayed and less effective at removing plaque from your teeth. As a rule of thumb, we recommend switching your toothbrush at the start of each season to make sure you’re properly cleaning your teeth.
Use Mouthwash: Using mouthwash won’t replace brushing or flossing, but it’s an excellent additional tool to boost your dental health. Using a mouthwash can help wash away harmful plaque or food debris lingering in the mouth. As a bonus, mouthwash is also great for freshening your breath.
Upgrade Your Tools: Of course, if you find that a manual toothbrush and traditional string floss work well for you, there’s no need to upgrade your dental tools. But for patients that want to improve their oral hygiene routine, it may be a good idea to look into other tools. Investing in an electric toothbrush or a water flosser may help bring your dental hygiene routine to a new level.

Use Products Tailored for Your Smile: With a vast array of oral health products on the market, it can be difficult to choose what will work best for your smile. We recommend choosing products tailored to your own concerns. For example, patients worried about discoloration should opt for whitening toothpaste or patients with tooth sensitivity should opt for desensitizing toothpaste.
Schedule Routine Dental Cleanings: While there are plenty of at-home tools out there, you should never skip out on professional dental cleanings. Your dental hygienist will thoroughly clean your teeth and remove tartar that is nearly impossible to remove yourself. Be sure to maintain great oral hygiene with the help of routine cleanings.
(04/16/2024)by Dr. Ian Smith
More Information: https://www.iansmithdental.com/dental-health/5-ways-improve-dental-hygiene-routine/
Views: 367
If You Need Tooth Decay Treatment, Don't Wait
Even after trying your best to prevent tooth decay, sometimes the dentist finds a little cavity or two. It may be tempting to put off tooth decay treatment when you're not feeling any pain, but procrastination comes with a price: Tooth decay doesn't repair itself, and what starts out as a minor problem can quickly become serious, changing your treatment options dramatically.
The Start of Tooth Decay
Tooth decay is actually a very sneaky disease that typically begins before a patient even notices, says the American Dental Association (ADA). Sticky bacterial plaque forms on your teeth and uses sugars in the foods you eat to create acids. These strong acids slowly soften and dissolve the hard enamel covering your teeth. Left untreated, decay will work its way through all the layers of your tooth.
Signs and Severity of Tooth Decay

You won't notice pain and sensitivity until decay goes through the enamel into the dentin layer, the Academy of General Dentistry notes. Dentin is made up of tiny nerve endings that become irritated and cause sensitivity when exposed to hot, cold, sweet, sticky and sour foods. You may also feel discomfort when biting down and find that food frequently gets trapped between your teeth.
Decay spreads rapidly through dentin because it is much softer than enamel. Root decay also spreads quickly, since the cementum covering on the root is not as hard and thick as enamel. Be warned that as tooth decay continues, your pain may be more frequent and intense.
It is important to remember that infection develops when decay and bacteria reach the pulp portion of your tooth, which contains the nerves and blood vessels. The ADA notes that pain from an abscessed tooth is persistent, serious and will likely keep you up at night. Other symptoms include fever, facial swelling and a bad taste in your mouth. You may notice pus draining from a red swelling on your gum near the root tip. Consequences can be serious if the infection spreads into your jawbone or throughout your body.
Tooth Decay Treatment

If your dentist detects a small area of erosion on your enamel before it reaches the dentin, he may suggest an approach that would help repair the spot. This process might include using mouthrinses, toothpastes or filling materials that contain fluoride, calcium and phosphates. Ask your dentist about using a fluoride varnish for treatment of early decay and cavity prevention.
When decay reaches the dentin, there is no turning back. A small cavity can be repaired with either an amalgam filling (composed of silver and other metals) or a tooth-colored resin material. If the tooth has lost a lot of its structure, however, your dentist may need to do a crown. Crowns strengthen and restore shape and function to your teeth, but they cost quite a bit more than a simple filling.
An abscessed tooth is the worst-case scenario, and your treatment options are slim: You can either opt for a root canal treatment or an extraction, though dentists will typically only do extractions when there are no other means of saving the tooth. Should you require a root canal, your dentist or an endodontist will remove the diseased pulp and clean and seal the pulp chamber; the ADA website contains more details about this process. After root canal treatment, teeth can become more brittle and break easily. If you lost a lot of tooth structure due to decay, your dentist may also recommend a crown for your tooth.
Do you see a pattern here? The longer you put off dental treatment, the more involved and expensive it becomes — and the more pain you may have to endure. The moral of this story is to go to the dentist at the first sign of trouble. Better yet, prevent decay from occurring by brushing and flossing daily, and visiting your dentist regularly for a more thorough cleaning and checkup.
(04/05/2024)by Colgate
More Information: https://www.colgate.com/en-ph/oral-health/fillings/if-you-need-tooth-decay-treatment-dont-wait
Views: 380
How To Keep Your Tooth Enamel Strong For A Long Time
The surface of your teeth is called enamel. It helps protect them from decay. Some wear and tear is normal, but there’s plenty you can do to keep that barrier strong. Take these simple steps for a healthy mouth and a winning smile.
1. Limit Sugary Foods and Drinks
Bacteria in your mouth feed on sugar from foods and drinks. Then they make acids, which soften and wear away your enamel. Chewy candies that stick on your teeth are can also cause damage. Soft drinks may have extra acids.
Soft drinks with artificial sweeteners are a smarter choice than ones with sugar, but they’re also acidic and will wear down enamel over time.

The best choice when you’re thirsty? A glass of plain water. Many flavored waters are acidic.
2. Eat Foods That Protect Enamel
Calcium in food counters acids in your mouth that cause decay. It also helps keep your bones and teeth strong.
Milk, cheese, and other dairy products help protect and strengthen enamel. Choose low-fat or fat-free items to help keep calories down. If you don’t eat dairy, look for foods with calcium added.

3. Avoid Over-Brushing
You can wear down your enamel if you brush too fast and hard. Hold a brush with a soft bristle at about a 45-degree angle to your gums. Then move it back and forth in short, gentle strokes, about the distance of one tooth.
Wait for up to an hour after eating sweets or citrus fruits before you brush your teeth. Acidic foods can soften enamel and may make it easier for you to damage it.
4. Use Fluoride
The American Dental Association (ADA) calls fluoride “nature’s cavity fighter” because it strengthens your enamel and helps repair the early stages of tooth decay. Fluoride also makes your teeth more resistant to acids that come from foods and from bacteria in your mouth.The ADA recommends fluoride toothpaste as soon as the first tooth appears and throughout your life. Rinsing with a mouthwash that has fluoride can also help prevent cavities and keep your enamel strong.
(04/04/2024)by Dean Dentistry
More Information: https://deancosmeticdentistry.com/how-to-keep-your-tooth-enamel-strong-for-a-long-time/
Views: 488
Ways To Prevent Getting A Cavity
From the time you’re old enough to know what “going to the dentist” is, you’ve probably heard about what you need to do to prevent cavities. Cavities are small holes in the enamel of your teeth, and they allow bacteria to enter and reach the soft dentin of your teeth.Eventually, those bacteria can cause infection, and that can lead to a host of health issues. Your best bet is to avoid allowing the cavities to form at all. At Goodman Dental Group, Dr. Brian Goodman and Dr. Tanner Goodman are happy to provide white fillings should you need them. However, we’d rather you not have cavities to begin with! Here are our best tips to help you prevent cavities.
Pay attention to how you brush
How often do you mindlessly brush your teeth, quickly, without paying much attention to what you’re doing? The American Dental Association (ADA) suggests you should brush for at least two minutes, at least twice per day, in addition to flossing once. Using a good technique to brush and using the right kind of brush are crucial in order for it to be effective in protecting your teeth.Scrubbing hard isn’t the way to go. Instead, hold your brush at a 45 degree angle to your gum line. Gently, brush back and forth. Focus on one tooth at a time, and try not to make sweeping strokes.When you brush the inside surfaces of your teeth, turn your brush vertical, and use a gentle up and down motion.Choose a brush that has soft bristles and that fits the size of your mouth. Replace your brush every three to four months or when you begin to notice signs of wear, like fraying.You may think brushing right after you eat could help protect your teeth, but the ADA recommends waiting at least an hour. If you do need to brush right after you eat, rinse your mouth with water first.
Avoid the harmful foods

Sugary foods are bad for your teeth because the bacteria that lead to cavities thrive on sugar. Limit the amount of sugary foods and beverages you consume to protect your teeth.Sticky candy that clings to your teeth for a long time after you eat it can be particularly damaging. Fruit juices, sodas, and other drinks high in sugar can also leave a film of sugar on your teeth.Bread, pasta, chips, and other processed, refined carbohydrates may also be harmful to your dental health. As those foods break down they become simple sugars and that, too, can raise your risk of developing cavities.
Eat more of the good stuff
Some foods naturally help prevent cavities. Eat more of these to improve your dental health.
Fruits and vegetables

Carrots, apples, celery, and other crunchy fruits and vegetables cause more saliva production. When you have more saliva, it washes away the food debris that can lead to cavities.
Calcium, vitamin D, and phosphates
Cheese, milk, and other dairy products may help fortify your teeth and help protect them. Aim for foods that contain calcium, vitamin D, and phosphates.
Phosphorus
Foods that are rich in protein, like meat, nuts, legumes, and eggs contain phosphorus. Phosphorus makes it easier for your body to use calcium, an essential nutrient for healthy teeth.
Enjoy chewing sugarless gum
Gum helps rinse away the harmful substances on your teeth, and can help you maintain good dental health. The xylitol in sugarless gum may also delay the growth of a specific bacteria that contributes to plaque formation.
Get professional cleanings regularly
Excellent dental hygiene at home is a key to good oral health; however, it can only take you so far. You also need regular professional cleanings to remove the plaque that builds up, no matter how often or thoroughly you brush.
In addition to keeping your teeth healthy, during regular cleanings, the providers at Goodman Dental Center check for any signs of problems and recommend any necessary preventive treatments. Schedule your next dental cleaning today, by phone or online.
(03/26/2024)by Goodman Dental Center
More Information: https://www.goodmandentalcenter.com/blog/ways-to-prevent-getting-a-cavity
Views: 385
Helpful Tips For keeping Your Gums Healthy
When most people think about oral hygiene, brushing their teeth is the first thing that comes to mind. And while taking care of your teeth certainly is important, ensuring that your gums are healthy is just as essential! That said, you might not be sure how to properly clean and care for your gums. Keep reading to learn more about the significance of healthy gums, along with some ways for preventing gum disease and keeping your gums pink and pristine.
Why Gum Health Matters
Even if you have the cleanest and whitest teeth in the world, it’s all for naught if your gums aren’t healthy! Your gums are very important and keeping them healthy will stave off many different oral health problems such as gingivitis, the earliest stage of gum disease. Gingivitis can cause your gums to become swollen and prone to bleeding—and if left untreated, it can develop into periodontitis and pose a threat to your teeth.
Luckily, gum disease is both preventable and treatable, although catching it before it can progress further is crucial. According to the American Dental Association, these signs might indicate gum disease:

Swollen, red, or tender gums.
Gums that have pulled away from your teeth.
Gums that easily bleed.
Separating or loose permanent teeth.

Consistently bad taste or breath.
How To Keep Your Gums Healthy
Since gum disease can pose a serious threat to your oral health and even your whole body, it’s important to take preventive measures to keep your gums in tiptop shape. Consider the following:
Brush and floss daily – You should brush your teeth twice a day or after every meal; this removes food and plaque that’s trapped between your teeth and gums. Flossing is also instrumental in the removal of this debris—your floss can reach where your toothbrush can’t!
Use a fluoride toothpaste – Certain toothpastes contain fluoride, which is a naturally occurring mineral with many positive health benefits that help your teeth and gums.
Consider a therapeutic mouthwash – These are usually available over the counter, and can help reduce plaque, prevent gingivitis, and reduce the speed that tarter develops.
Quit smoking – Smoking is terrible for your oral health, period. It’s strongly associated with gum disease since it weakens your immune system. It also reduces your gum’s ability to heal once they’re damaged.
Visit your dentist regularly – Your dentist can detect early gum disease symptoms, but only if you visit them! Biannual checkups and cleanings can work wonders for your oral health and prevent gum disease and other problems from developing.
The next time you’re in the bathroom brushing your teeth, don’t forget about your gums! Their health matters too and keeping them vital will ensure that your mouth is pain and problem-free for the foreseeable future.
(03/21/2024)by Peaks View Dental
More Information: N
Views: 286
What You Should Know About Choosing A Mouthwash
Maybe you have been told you should be using a mouthwash. Or, maybe you feel that it is an important step in maintaining your oral hygiene. Whatever your reason, if you have ever stepped into the mouthwash aisle at your local drugstore recently, you have likely felt overwhelmed with options.
You want a mouthwash that will benefit your oral hygiene, but determining what type of mouthwash works best for you is an entirely different story. Here’s what you should know about choosing a mouthwash.
All Mouthwash is Not Created Equal
There are so many mouthwashes that will make a list of claims that you should be wary of until further inspection. For instance, there are whitening mouthwashes, plaque-removing mouthwashes, and more. Glancing at the package will help you determine what it wants you to know. Rather than just reading these words, look for the ADA (American Dental Association’s) Seal of Acceptance. As an independent organization, this seal will give you comfort in knowing that it has been tested and proven to be true.

Then, look for one that is designed for either your oral health or what you are trying to achieve.
Choosing the Right One for You
There are different mouthwashes made for different things. Choose one that best fits your oral health goals.
Gingivitis and Gum Disease. If you are currently dealing with gingivitis or gum disease or have been treated for periodontal disease, then a mouthwash designed for this may be a great option. Even those at risk should consider this mouthwash.

Sensitive teeth and gums. Tooth sensitivity is quite common. And, there are mouthwashes out there that can help lower the severity of your tooth sensitivity. Many times it will state on the bottle when it will benefit sensitivity. If not, go ahead and look for one that has calcium phosphate, sodium fluoride, and stannous fluoride in it as they are all strengtheners that will help offer your teeth some protection.
Dry Mouth. There are a few different types of mouthwash that are designed to help reduce dry mouth. And what you will notice is that they won’t contain alcohol. Why? Because alcohol will dry your mouth out more. So, look for a mouthwash that is alcohol-free or that states it is made for those with dry mouth. Keep in mind that there are prescription options available if the over-the-counter ones do not.
Protection and Prevention of Dental Issues. If your teeth are in relatively good shape and you don’t have any oral health concerns, a general mouthwash will work just fine. These usually contain fluoride and will help make your teeth stronger. Thanks to additions like antibacterial, antimicrobial, anti-plaque, and more, serious dental concerns can be addressed before they become too big of an issue - just by regularly using mouthwash.
Mouthwash is Mouthwash
It is important that you use mouthwash as mouthwash - and not as a replacement for brushing or flossing. Your oral hygiene routine needs to contain all three things. You should be brushing, flossing, and rinsing with mouthwash twice a day, at least.
(03/13/2024)by Emerson Dental
More Information: N
Views: 311
Five Dental Fads You Should Brush Off
Dental hacks – from charcoal toothpaste to coconut oil canker sore treatments – are all the rage right now, but these fads may actually not be a reason to smile after all.
In fact, many are ineffective, and some can be even detrimental – and dangerous – to your oral health.
So how can these latest trends affect your teeth? Before you try out that new viral trend on social media, Matthew Messina, DDS, director of the Ohio State Wexner Medical Center Dental Clinic at Outpatient Care Upper Arlington, has some advice for you to chew on.
1. Oil pulling

Oil pulling involves swishing a tablespoon of coconut oil or sesame oil around the mouth for up to 20 minutes in an effort to improve bad breath and yellow teeth. Although oil pulling is an ancient practice dating back more than 3,000 years, Dr. Messina says it is currently the most common dental fad he sees.
“Three thousand years ago, people didn't have fluoride toothpaste off the shelf, so they used what they had,” he says. “The ancient Romans used a paste of ground up eggshells and honey. Ancient Greeks tried rinsing with urine to whiten teeth.”
Despite its popularity, Dr. Messina emphasizes that there is no scientific proof that oil pulling has any beneficial effects on oral health.
“Just because a practice is old, doesn't mean it is effective,” he says.

2. Charcoal toothpaste and other whiteners
Today, Twitter and Facebook are littered with somewhat frightening videos of people lathering on chunky black toothpaste in hopes that it will transform their stained teeth into pearly whites. While charcoal toothpaste can initially whiten teeth, Dr. Messina says that over time it can erode your enamel, the outer layer of the tooth that measures slightly more than a millimeter thick.
“If you look at enamel in a high-powered electron microscope, tooth enamel looks like chain-link fencing,” Dr. Messina says. “The enamel crystal is the fence and colored stains become lodged in the spaces in the matrix.”
Traditional tooth whiteners at the dentist are safe and effective because they use a form of peroxide to bubble out the stains and leave the enamel matrix intact. However, home remedies like charcoal toothpaste, or rinses with lemon juice, carbonated soda or vinegar, are highly acidic and abrasive. They can wear down the entire enamel, leading to tooth sensitivity and even more yellowing.
“We lose some stains, but we lose enamel too. There is only a thin layer on the tooth and it doesn't grow back,” Dr. Messina says. “When it’s gone, it’s gone.”
3. Canker sore home remedies
Canker sores are small, shallow ulcers in the mouth that are common in people ages 10 to 20. They can be painful, and they make eating and talking uncomfortable. Many beauty gurus swear by coconut oil to heal canker sores, citing its anti-inflammatory properties, but Dr. Messina is skeptical about this practice.
“Coconut oil, in and of itself, does nothing to heal mouth sores,” he says. “It can coat them to reduce sensitivity to a degree, but that really isn't healing.”
If you have a sore in your mouth that has been there longer than two weeks, Dr. Messina urges you to see a dentist to have it evaluated, as it could be a sign of oral cancer. It's uncommon, but early detection leads to early cure.
4. Fluoride-free toothpaste
In the early 1900s, dentists discovered that fluoride, in regulated amounts, could help prevent tooth decay. Now, the mineral is regularly added to community water, toothpaste and mouthwash to make teeth stronger and more resistant to cavity-forming acids.
Fluoride toothpaste is much better at preventing cavities and tooth decay than a fluoride-free one.
“Look for a toothpaste with an American Dental Association – ADA – seal on it. You can be confident that a product with an ADA seal says what it does and does what it says. You have our word on it,” Dr. Messina says. “Fluoride is nature's cavity fighter, and in toothpaste, it does an excellent job of reducing decay.”
5. Grills
The trend of wearing teeth jewelry and grills seems to be waning, but Dr. Messina still warns people against the practice. Poorly fitting jewelry on your teeth can attract food debris and bacteria, which can stick in hidden and sometimes unreachable places, making bacteria very difficult to remove.
“The rate of decay under grills and the development of gum disease around mouth jewelry are very high,” Dr. Messina says.
So before you decide to coat your mouth with crystals or metal jewelry, think again.A nice set of clean, white teeth will look a lot better, anyway.
So if today’s dental fads are ineffective, and even dangerous, how can you achieve sparkling white teeth and fresh breath? Dr. Messina says it is as simple as remembering the “Healthy Four.”
“Brush twice a day – once after breakfast and once before bed with a soft toothbrush and ADA toothpaste – floss once a day, eat a healthy diet and see your dentist on a regular basis,” he says.
(03/12/2024)by Wex Medical Center
More Information: N
Views: 556
What Is Antibiotic Prophylaxis?
If you hear the term antibiotic prophylaxis and think, “it's all greek to me,“ that's because, well... it is. Prophylaxis is Greek for “advance guard,“ and in this case, it refers to using antibiotics to help you prevent infection while undergoing certain dental treatments. If you're wondering if you'll need antibiotic prophylaxis, we'll let you know the specific conditions in which it's recommended so you can go into your appointment confident that you're getting the dental treatment that will make you smile.
An Important Note on Antibiotic Resistance
Antibiotics are considered one of the most important scientific discoveries of the 20th century. Bacterial infections that were once considered serious have become preventable and treatable. However, bacteria are adapting and beginning to build up a resistance to some antibiotics because of how much they’re prescribed, so it’s important they’re only utilized when necessary.
According to the Centers for Disease Control (CDC), antibiotic resistance is one of the biggest health challenges of our time. The CDC says that “appropriate antibiotic prescribing means antibiotics are only prescribed when needed, and when needed, the right antibiotic is selected and prescribed at the right dose and for the right duration.” They cite a study revealing that over 30% of antibiotics prescribed are unnecessary. And specific to dental procedures, an Agency for Healthcare Research and Quality-funded study found that ”about 81 percent antibiotic prescriptions given to patients before a dental procedure to prevent cardiac infections were considered unnecessary by current guidelines.”

Your dental and medical professionals are in the best position to determine if you need antibiotics. If you’re wondering if you need them and why – it’s important for you to ask.
When Are Antibiotics Needed for Prevention?
According to the American Dental Association, there are very few circumstances in which antibiotics should be used for preventive measures before dental procedures.
People with prosthetic joints were once prescribed antibiotics before dental procedures, believed to be at a higher risk of a blood infection affecting their prosthetic. Studies have since shown otherwise, and the ADA now recommends against it.

People with specific heart conditions may be at a higher risk of infective endocarditis (bacteria reaching the heart through the bloodstream) but in fewer cases than previously thought – limited mostly to valvular heart conditions or congenital heart defects.
Commonly Prescribed Antibiotics
Amoxicillin is the most commonly prescribed oral medication for antibiotic prophylaxis. If you're unable to take oral medication, your doctor may prescribe an intramuscular (IM) shot or intravenous (IV) infusion of another antibiotic like ampicillin or cefazolin. If you're allergic to certain antibiotics, your surgeon might give you a dose of clindamycin instead.
Dosing Requirements and Side Effects
If your dental and medical professional determine antibiotic prophylaxis is a necessary preventive measure for you, your dosage will depend on your age, size, and the antibiotic you're prescribed. Typically, oral antibiotics should be taken one hour before your procedure and are best taken with a small amount of food. They can also be taken up to a few hours after the procedure if you forgot to take them before your treatment, but it's best to follow your surgeon's instructions and arrive at your dental appointment fully prepared. Because different antibiotics have different side effects, talk with your dental professional about what you can expect and let them know if you have any questions or concerns.
Very few patients need to take antibiotics before seeing a dentist, so it's unlikely you will have to build taking a pill into your routine on appointment days. If you've recently undergone joint or heart surgery, talk to your dental professional about the need for antibiotic prophylaxis for dental or dental hygiene treatment. They know the specifics of your condition and will best be able to offer advice tailored to your individual needs. At least now, you can have an informed conversation with them without saying, “it's all Greek to me!“ And you can be confident you're getting treatment that will make you smile.
(03/04/2024)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/threats-to-dental-health/what-is-antibiotic-prophylaxis
Views: 464
Chronic Bad Breath? You May Need To Visit The Dentist
Embarrassed by chronic bad breath? Breath fresheners can be an effective short-term fix.
But if bad breath persists despite a regular brushing and flossing regimen, it’s best to see your dentist for an exam.
What Causes Bad Breath?
Bad breath, or halitosis, is an embarrassing problem that could signify a more serious medical issue, especially if you’re already practicing good oral hygiene.

The tongue harbors many bacteria, which are normally kept in check by saliva. However, an excess of bacteria can form plaque on your teeth and gums—producing plaque and volatile sulfur compounds that cause bad breath.
Risk factors for bad breath include:
Smoking or chewing tobacco
Poor oral hygiene
Dry mouth due to medications

Gingivitis or periodontal disease
Medications that interfere with saliva production (antidepressants and antihistamines are common offenders)
High-protein diet
Good Oral Health is Essential for Overall Health
Maintaining good oral health is essential for overall wellness.
Teeth and gums are vulnerable to decay, periodontal (gum) disease, tooth loss, and oral cancers. You can prevent many problems with regular visits to your dentist for exams, cleaning, and x-rays.
The American Dental Association recommends these steps for good oral health:
Brush your teeth twice a day with fluoride toothpaste. Use an ADA-approved soft-bristled brush. Floss once a day unless your dentist tells you otherwise.
If you have gingivitis or periodontal disease, floss at least once a day and brush after meals whenever possible.
Visit your dentist regularly—at least twice a year—for checkups and professional cleanings. You may need professional cleanings more often If you have problems with your gums or periodontal disease.
If you use tobacco products, stop. Smoking increases the risk of developing oral cancer and causes bad breath, stained teeth, and mouth sores.
If you drink alcohol, do so in moderation (no more than one drink per day). Excessive alcohol consumption can damage the tissues of the mouth.
Common Signs of Dental Problems
Many people don't realize that their oral health is an important factor in maintaining overall health. A healthy mouth can help prevent severe conditions such as heart disease, stroke, and cancer—not to mention periodontal disease that can lead to tooth loss.
Some signs of dental problems are obvious, such as bad breath or pain when chewing.
These are common signs of dental problems:
Bleeding gums. Bleeding may be a sign of gum disease caused by plaque. Left untreated, gum disease will worsen and may eventually lead to tooth loss and other problems.
Swollen or discolored gums. If you notice any changes in your gums, see your dentist. Changes in gum tissue may indicate a more serious problem.
Bad breath (halitosis). Bad breath can occur when your teeth decay or become infected. Halitosis can be eliminated with proper treatment for any dental problems.
Tooth pain or sensitivity. See your dentist if you’re experiencing persistent tooth sensitivity or toothaches.
Embarrassed By Bad Breath? Schedule an Appointment Today
Good oral hygiene can help prevent embarrassing bad breath, but you should see your dentist if the problem persists.
A dental cleaning removes plaque and reduces your chances of developing cavities and gum disease that can lead to bad breath. Routine dental exams are the best way to protect your smile.
(03/04/2024)by Dr Todd
More Information: https://www.drtoddsmileon.com/chronic-bad-breath-you-may-need-to-visit-the-dentist/
Views: 366
Hydrated Silica in Toothpaste
If you're on the hunt for a new toothpaste or just feel like you need an added ingredient that will clean your teeth more efficiently, you may come across the term "hydrated silica." While cultures like the ancient Egyptians and Romans used eggs and oyster shells as teeth cleaners, we've luckily come a long way with abrasives for our teeth! Hydrated silica is a much gentler abrasive that, for the most part, is very safe to use on your smile. Let's go over what it is, its benefits, potential drawbacks, and why you should consider adding it to your oral care routine.
What Is Hydrated Silica?
Hydrated silica comes from a hydrated form of silicon. Did you know that silica is a substance that makes up a large part of the Earth's crust? The most common form of silica you may be familiar with is sand! But the hydrated version of silica is a substance used in many everyday items, like a coating to paper and textiles. You're also very likely to find this ingredient in your bathroom's medicine cabinet in some of your everyday products. Hydrated silica is a common ingredient found in many personal care products, including cosmetics and toothpaste. It's an abrasive, an absorbent, and a bulking agent in personal care product formulas and is perfectly safe to use in toothpaste.
Benefits of Hydrated Silica

The primary benefit of hydrated silica in toothpaste is its abrasiveness. Stains often settle on our enamel, the outermost layer of our teeth. Some kinds of toothpaste will whiten teeth with bleaching agents, such as hydrogen peroxide, which changes your enamel color. But whitening toothpaste with abrasive ingredients, such as hydrated silica, scrub the stains from the surface of your teeth.
The other useful quality of hydrated silica's abrasiveness is its cleaning ability. Our mouths are full of bacteria, which, when mixed with the foods and drink we ingest, can lead to dental plaque (biofilm). If you brush your teeth twice daily with a clinically proven toothpaste, you should be able to keep plaque at bay. However, when dental plaque isn't scrubbed away and begins to build up on your teeth, it can become a harder substance, known as tartar. You can't clean away tartar on your own, and because of its porousness, it will become an easy substance for even more plaque to adhere to. Only a dental professional can get rid of your tartar! Plaque and tartar contribute to tooth decay and gum disease, which is why it's vital to stop their buildup as soon as you can. Brush twice a day and clean between your teeth once a day with floss, an interdental brush, or another interdental cleaning device.
If you opt for a toothpaste with hydrated silica or other abrasive ingredients, confirm that the tube has the American Dental Association (ADA) Seal of Acceptance. The ADA only awards toothpaste with this seal if it has a relative dentin abrasivity score of 250 or less. That means that with regular daily use and a proper brushing technique, the toothpaste won't cause any wear on your teeth. By finding this seal on your preferred toothpaste, you're confirming it's both effective and safe!
The Drawback of Hydrated Silica

One drawback of abrasives in toothpaste is that they can lead to tooth sensitivity, especially if you brush very hard and do not brush with a soft-bristled toothbrush. The dentin and the pulp that lie beneath your tooth's enamel are sensitive. If your enamel becomes worn down, you could feel discomfort when brushing with a toothpaste that contains abrasives. It's just another reason to keep your mouth healthy and your enamel strong.
If you experience sensitivity, consult your dental professional. They can recommend which toothpaste and toothbrushes you should consider. They will also examine your mouth to root out the cause of your sensitivity. But hydrated silica toothpaste is, in almost all cases, a very safe and efficient toothpaste to use. Who doesn't love the feeling of smooth teeth in a white smile? If you don't experience any sensitivity, this toothpaste type can be your smile's best friend!
(02/16/2024)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/threats-to-dental-health/hydrated-silica-in-toothpaste
Views: 694
Warning Signs From Your Tongue You Shouldn't Ignore
If you have a bleeding mouth sore or pain that lingers for more than a couple of weeks, don’t igore it.
“We see patients all the time who had an irritation around their tooth that ends up being squamous cell cancer, which may have been bothering them for up to a year,” says ear, nose and throat specialist Brian Burkey, MD, MEd.
Some oral cancers are not obvious to us as we look in a mirror and can even be hiding behind the teeth or under the tongue.
“The good news is that when picked up early, these cancers are highly, highly curable,” says Dr. Burkey. “Early detection is key.”

Seven symptoms to look out for
It’s important not to ignore these symptoms, which could signal medical problems or, in limited cases, oral cancer:
Nagging mouth pain.
Bleeding sore in the mouth that won’t heal and lasts for more than two weeks.

Swelling in the neck that lasts for more than two weeks.
An area in your mouth that becomes discolored and stays that way.
A lump or thickening in your cheek that doesn’t go away.
Numbness in your tongue or another part of your mouth.
Constant feeling of something caught in your throat or a change in your voice that lasts longer than two weeks.
While not an exhaustive list, these are symptoms that can slip under the radars of our busy lives.
“That’s why it’s important to notice when they don’t resolve,” says Dr. Burkey. “If symptoms last for more than two weeks, get them checked out by a doctor or dentist.”
Regular oral cancer screenings are crucial
Besides watching for any symptoms, it’s important to get regular oral cancer screenings to catch problems at their earliest stages. Here, Dr. Burkey explains what you need to know — and what to expect:
Who does the screenings? Your dentist is often your first line of defense when screening for oral cancer, but oral surgeons and ear, nose and throat specialists can also perform screenings.
How often do I need a screening? While there are no official recommendations for screenings, it’s important to get screenings during your usual dental checkups, twice a year.
Do I need to request a screening from my dentist or are they routine? Screenings are generally part of your normal dental exam, but ask your dentist to do one if they haven’t.
How long to screenings take? Oral cancer screenings take less than 10 minutes. Your doctor or dentist will perform a visual screening and feel the tongue looking for abnormal color and firm lesions. You also fill out an information form so that the doctor or dentist can pay close attention to any specific areas of concern.
Do the screenings hurt? No, they are generally painless.
How to reduce your risk
Here are ways to lower your risk of getting oral and head and neck cancers:
Quit tobacco. About 90% of people with oral cancer use tobacco (smoking or chewing), and their risk increases with the amount and length of time they use. Tobacco is most closely associated with ‘oral cavity’ cancer specifically, which affects the mouth, including lips, teeth and gums.
Take precautions against HPV. There is a dramatic rise in oropharyngeal cancer, or cancer in the tonsil and base of tongue associated with the human papilloma virus (HPV). You can’t see this area yourself, so finding it requires an exam from an ear, nose and throat physician. HPV is a sexually transmitted disease and is preventable with a vaccine and/or appropriate safe sex precautions, depending on one’s age.
Drink alcohol in moderation. Though less a risk factor than those above, alcohol use can also increase your risk of oral cancers.
Limit time in the sun. You want to protect your face to combat skin cancer, but in particular, don’t forget to protect your lips with sunscreen. They are often forgotten but they need protection too. If you work outside, try to avoid being in the midday sun. You should also wear a hat that shades your face whenever possible.
Good oral hygiene. Alongside getting your dental checkups twice a year, continue good oral hygiene at home by brushing twice a day and flossing once a day. Talk to your dentist about which mouth rinse they recommend, especially if you have mouth sores.
Incorporate a healthy diet. Keeping your teeth health go beyond just brushing. The American Dental Association recommends having a diet filled with plenty of water, vegetables, whole grains, fruits and lean protein. Make sure to avoid sugary treats and snacks to help keep harmful bacteria away.
(02/07/2024)by Health Digest
More Information: N
Views: 435
The Role of a Dentist in Treating Sleep Apnea
The Role of a Dentist in Treating Sleep Apnea
Today, nearly 25 million adults in the country are affected by sleep apnea, according to the American Academy of Sleep Medicine. The statistics are staggering, and the health risks are dangerous. Doctors and healthcare professionals have noticed this growing problem. Now, they are collaborating to develop effective treatment solutions and combat it.
People diagnosed with sleep apnea now have more treatment options than ever and are able to successfully overcome the problem. With effective treatment, the health risks associated with OSA can be alleviated.
As obstructive sleep apnea continues to present an increasing threat to the health of Americans, the medical community is working together to find treatment solutions. Learn about how dentists are working with physicians and sleep clinicians to treat the symptoms of sleep apnea.

What is Dental Sleep Medicine?
An area of specialization for dentists focuses on treating loud snoring and sleep apnea. This field is known as dental sleep medicine. Dentists trained in this field collaborate with doctors and clinicians to find the best treatment plan to address a patient’s sleep disorder. Their role is often to help manage a patient’s snoring and OSA symptoms through oral appliance therapy.
There are two dental appliances which may be recommended, together with CPAP therapy, to treat sleep apnea: mandibular advancement devices (MADs) and tongue-retaining mouthpieces.
Mandibular Advancement Devices

MADs look like athletic mouth guards which fit over the upper and lower sets of teeth. A hinge connects the two trays in the center. This device holds the lower jaw and tongue in a slightly forward position at night. It helps keep the soft tissues in the back of the mouth and throat from blocking the airway when they relax during sleep. Specially trained dentists can adjust the position and fit of MADs to increase comfort and effectiveness.
Tongue-Retaining Mouthpieces
For sleep apnea sufferers with minimal jaw flexibility, tongue-retaining mouthpieces may be helpful. These oral devices keep the tongue from falling back into the airway while sleeping. It fits around the tongue and holds it in place using a light suction force.
Dental Device Integration with Sleep Apnea Treatment
The first step for successful treatment of obstructive sleep apnea is to talk with your doctor about the symptoms you are experiencing. Then, a sleep study should be performed to confirm the diagnosis. This can be done either at a certified clinic or at home with the guidance of a clinician.
For most people with sleep apnea, CPAP therapy is recommended as the first treatment measure. Delivering a continuous stream of pressurized air throughout the night, CPAP therapy is the best way to support someone with moderate to severe OSA. Oral devices, including the MAD and tongue-retaining mouthpiece, can help those with mild sleep apnea. Successful treatment may also include using both an oral device and a CPAP machine.
Getting Oral Devices to Treat Sleep Apnea
Oral devices should only be used when recommended by your physician who is overseeing the treatment plan for OSA. These devices are provided by dentists specialized in sleep medicine who then follow up with their patient and help adjust the treatment plan as needed.
Over-the-counter devices for sleep apnea treatment are never recommended. Though these products are cheaper and readily available, they often only alleviate symptoms, such as snoring. Over-the-counter oral devices often do not prevent the dangerous apneas that occur while you are asleep.
What is the Role of Dentists in Treating Sleep Apnea?
Because sleep apnea is a growing threat for Americans and presents such dangerous health risks, doctors and dentists must work together to address the problem. According to the American Dental Association (ADA), dentists play a key role in diagnosing patients who are suffering from sleep-related breathing disorders.
By getting a patient’s full medical history, a dentist can identify symptoms and refer them to the appropriate doctor. Then, following a physical evaluation, diagnosis and sleep test, the dentist can help determine if an oral device could be an effective treatment solution. Only those trained in dental sleep medicine can provide the appropriate oral device and optimize the fit for the patient. As the patient continues sleep apnea treatment, the dentist will communicate with the physician to track progress and ensure the best treatment.
Find the Best Treatment Options for Sleep Apnea
The journey toward successful management of obstructive sleep apnea and its symptoms should start today. Discuss your concerns with your primary physician and request an overnight sleep evaluation. The trained specialists at Sleep Health Solutions will work with your healthcare providers to effectively diagnose and treat any sleep disorder.
(02/01/2024)by Sleep Health SolutionsViews: 259
Cavity Prevention is Easier Than You Think
Did you know that tooth decay—or cavities—is the most “prevalent, chronic disease” according to the National Institutes of Health? The amount of children and adults alike that get tooth decay outweighs all the other types of disease and chronic conditions a person can develop. The crazy part is, most people don’t even realize that their cavities are actually considered to be a “disease”, nor do many people realize they even have cavities. Tooth decay is a 100% preventable condition with the right oral health habits. Cavity prevention involves some simple steps that make a not-so-simple difference in the health of your teeth and mouth.
Brush Your Teeth
When you eat, sugars in your food combine with bacteria in the mouth to form plaque. Your mouth makes this sticky, acidic substance every single time you eat. That means, the more sugar you eat, the more plaque you make. Plaque sits on your teeth because it’s so sticky and erodes your tooth enamel. If it sits there long enough, you will get cracks and open areas of your teeth, where plaque then gets inside your tooth and decays it. That decay is known as “cavities”, and cavities can lead to tooth loss.
Your gums also become irritated by acidic plaque, and will start to pull away from the teeth, leading to mushy, red and bleeding gums as well as tooth loss. The biggest way to prevent both of these issues is to brush your teeth! The American Dental Association recommends brushing your teeth at least twice a day, for two minutes at a time to keep your teeth healthy. Brush after every meal for even better cavity prevention, and especially brush your teeth before bedtime, so that cavities can’t form overnight.

Use Fluoride Products
Fluoride is a naturally-occurring mineral in the earth’s crust. In dental trials, it was found to act as a barrier between the teeth and acidic/sugary foods and drinks. Fluoride coats the teeth, helps them to remineralize, and diminishes damage caused by foods and drinks.
The American Dental Hygienists’ Association reports that fluoride was responsible for reducing tooth decay by 50-60% since World War II. This is because it was added to the public water supply to strengthen the teeth. If you want your teeth to be more resistant to the acid found in plaque, as well as erosion, use dental products with fluoride in them, or get a prescribed fluoride treatment from your dentist.
Don’t Forget to Floss

Did you know that flossing is integral to cavity prevention? So many people don’t floss, or don’t floss enough. However, studies show that about 40% of your tooth surfaces can’t be reached by simply brushing your teeth. That’s why you want to floss 1-2 times a day or after every meal to clean those areas of the mouth. Use new floss every time and floss all the way up in your gum line, making sure to gently scrape the teeth as you go.
Avoid Frequent Snacking
We mentioned brushing your teeth after every meal for great cavity prevention. This is what you definitely want to do if you are a frequent snacker. Snacking all day will continually expose your teeth to decay-causing plaque and acids. However, when you eat your 3-4 meals a day instead, you only have those times when sugars are hitting your teeth. For better cavity prevention, stick to set meals instead of all-day snacking.
Avoid Sugary Sweets and Drinks
Sugar is the main cause of cavities! Follow these tips for cavity prevention:
Limit your sugar consumption each day. Men should have no more than 9 teaspoons (36 grams) of sugar a day. Women should have no more than 6 teaspoons (25 grams), children should stop at 6 grams and infants should have none.
Avoid acidic drinks like juices and sodas. Sodas contain carbonic acid, which is an acid that erodes tooth enamel. It’s also full of sugar. Citrus drinks and juices contain citric acid as a preservative, which has the same effect. Sparkling water also contains carbonic acid.
Avoid hard candies, chewy candies, suckers, taffys and other types of candies that stay on the teeth for long periods of time. These decay the teeth easier.
If you drink carbonated, acidic, or sugary drinks, make sure you sip through a straw. This limits the drink’s contact with your teeth.
Eat Tooth-Healthy Foods
Some foods are great for the teeth, and those are ones that have minerals such as calcium and phosphate. Look for dairy foods such as milk, yogurt, cheese and eggs to help with cavity prevention. These foods will remineralize the teeth when you eat them, building them up stronger.
Visit the Dentist Regularly
What is the best way to prevent tooth decay from happening? Good oral hygiene! In fact, if you practice good oral hygiene, then you can potentially avoid tooth decay for your entire life. You can also avoid problems such as gum disease, which affects more than 64 million American adults.
We can detect the presence of tooth decay, gum disease, and other oral health problems if you’re visiting the dentist regularly. The ADA and other experts recommend visiting the dentist at least twice a year for comprehensive exams and dental cleanings. So many individuals fear the dentist because of the thought of shots and drills. Only 65% of people are visiting the dentist each year, and only once instead of twice. Exams and dental cleanings are non-invasive, don’t hurt and are the easiest dental services you can get. They are key in preventing tooth decay and gum health issues that would actually make you need dental work.
(01/31/2024)by Dr Ania
More Information: https://drania.com/cavity-prevention-is-easier-than-you-think/
Views: 297
Six Ways to Care for Swollen, Bleeding Gums
Gums are an integral and often overlooked part of the mouth.
Gums are the part of the oral anatomy that serve to contain and protect the teeth and bone, they can demonstrate some of the earliest signs of poor oral health.
While healthy gums are pink and resilient, gums that are swollen, sore, or bloody may be a sign of gum, or periodontal, disease.
According to the Center for Disease Control and Prevention (CDC) 47.2% of people over the age of 30 have some form of periodontal disease.

What causes gum swelling?
Gum swelling is caused by the buildup of plaque and subsequent bacteria.
The colonization of the bacteria causes inflammation and other adverse conditions. This is gingivitis, an early stage of periodontal disease.
Gingivitis, when ignored, can lead to even worse ailments. Cavities, abscesses, and tooth loss are unfortunate symptoms of advanced gum disease.

Receding gums provide the perfect environment for bacteria colonies to grow and flourish. Without proper hygiene, the bacteria is allowed to thrive and eat away at the surface of the teeth making your teeth sensitive.
Fortunately, this negative progress can be prevented with proactive measures.
The American Dental Association recommends brushing twice each day with fluoridated toothpaste, flossing daily, and visiting a dentist twice annually for cleanings and exams.
Read along for six simple ways you can quickly reduce gum swelling and improve your overall oral health. These steps are straightforward and inexpensive.
6 Ways to Reduce Gum Swelling Quickly
1. Brush Twice Daily
If you are showing early signs of gum disease, it is a good time to start thinking about your brushing routine. It is important to brush twice each day, preferably once in the morning and once in the evening.
However, what is even more important is your brushing technique.
The ADA recommends you use a soft bristle brush and fluorinated toothpaste. At a 45-degree angle to the gums, brush in short wisps, until you’ve brushed the entire surface, front and back, of your teeth.
A dentist or hygienist can help you to establish an efficient routine.
As a reminder, brushes should be thrown out and replaced every three to fours months. Otherwise, once the bristles on your toothbrush begin to warp, it is time for a new one.
2. Flossing
Flossing helps to remove stubborn plaque in the hard-to-reach breaks between teeth. It is important to floss once a day. Your flossing technique is crucial.
Food particles and small debris left to fester between teeth and gums quickly turn to plaque and, eventually, tartar.
While many people, especially those with dental work and braces, experience frustration and, sometimes, apprehension, when it comes to flossing, there are special techniques and products that can make this task easier.
Flossing picks with soft bristles help for people to reach around oral hardware or floss without putting stress on a weakened gum.
Such products can sometimes be easier to manipulate for a number of reasons. However, typical nylon floss is a great tool in combatting oral bacteria.
3. Eat Well
Plaque and tartar come as a result of lingering food particles.
While proper dental hygiene can help to remove these bits, eating less sugar and more foods that are rich in calcium and vitamin C can help strengthen your teeth and better their environment.
Snacks, such as sugar-free yogurt, nuts, and leafy greens, can provide essential bone and teeth building vitamins and minerals.
4. Drink Water
We all know that water is essential to life; moreover, it can improve your oral health too. Drinking water helps your body to flush harmful bacteria out of the mouth.
It is also beneficial to switch from sugary fruit juices and sodas to water.
No matter what motivates you to increase your daily H2O intake, your gums will likely see a quick improvement.
5. Mouthwash
Mouthwash is an effective product in the war against oral bacteria. However, many over the counter rinses contain irritating fillers, such as dyes, harsh chemicals and alcohol, which can give you a lingering bad breath.
There are many all-natural antiseptics that can help rid your mouth of harmful bacteria without stimulating your already sore gums.
Many mouthwash products can help to quickly strengthen your gums by hindering the continued growth of oral bacteria.
6. Mindful Choices
If it is your goal is to quickly reduce gum swelling, you’ll want to take into account how your daily food and substance intake are going to impact your mouth.
Hard, chewy foods should be avoided, as they put surplus pressure on an already weakened system. Moreover, sharp food particles can lead to gum abrasions that can become painful abscesses.
Additionally, foods that are too hot, cold, or acidic may only worsen your discomfort. Therefore, it may be best to abstain from such foods until your gums are strong enough.
It is also important to visit a dentist frequently. Dentists can help to identify, track, and repair your teeth. A hygienist can also provide a deeper cleaning than you can at home.
(01/07/2024)by Oxyfresh
More Information: https://oxyfresh.com/blogs/dental-health/6-ways-to-care-for-swollen-bleeding-gums
Views: 487
In Your 40s? Here Are Four Things You Need to Know About Your Oral Health
As you age, especially after you turn 40, there can be so much more to worry about than you think. What if you had the ability to absolutely perfect your smile? What if you could change everything that years of living in lockdown have done to your oral health? Join your Woodlands dentist as we break it all down for you, so it’s easy to understand.
Top Tips for Healthy Teeth
1) Water, Water Everywhere
Some articles and research suggest that drinking enough water every day is one of the most beneficial ways to keep your smile in good shape. It’s important to remember that no matter how easy it may be to reach for a fizzy drink or some sweet tea instead, it’s better to drink water whenever you can, especially if your body is dehydrated. When you consciously make an effort to drink more water after you eat meals or a snack, this helps to wash away leftover debris in your mouth and keep your teeth clean in between brushing.

2) Clean Everywhere in Your Mouth
You might think because you brush your teeth every day that you’re in the clear as far as deterioration or decay is concerned. However, there could be more to your at-home oral health care routine that you’re missing out on. Your dentist in The Woodlands can tell you that so many common oral diseases actually start between your teeth, where a brush can‘t always reach. The American Dental Association says that traditional brushing alone only cleans about 60 percent of your smile — what about the areas left behind?
3) Decrease Your Coffee and Alcohol Intake
Because life has been rough on us all over the past few years, it’s easy to turn to things like coffee and alcohol for some relief. However, these beloved beverages could be causing some issues for your oral health. Coffee is highly acidic, leading to a breakdown in your tooth enamel over time, with decay creeping in right behind. Alcohol is no different. It contains a lot of sugar which can worsen tooth decay or gum disease over time.

4) Eat Your Fruit and Veggies
While it’s certainly OK to indulge in some of the fine foods The Woodlands offers, it’s also important to remember to eat healthy too — especially crisp fruit and vegetables. Why? Because they can actually help clean your teeth rather than create a place where decay and cavities can cause trouble for your oral health. Also, the antioxidant vitamins that fruit and veggies contain will help to protect your gums from disease or infection.
In addition to all of these things, it’s important to see your Woodlands dentist regularly for checkups and cleanings, too, especially when you’re in your 40s. Let us help you schedule a hassle-free consultation or cleaning and keep your smile healthy and happy.
(01/05/2024)by The Woodlands Dental Group
More Information: https://www.thewoodlandsdentalgroup.com/in-your-40s-here-are-four-things-you-need-to-know-about-your-oral-health/
Views: 473
The Six List: At-Home Dental Trends To Avoid
"The 6 list" is a feature exploring various topics on oral health, curated for both patients and dental professionals to share with their patients. "6 at-home dental trends to avoid" was medically reviewed by David R. Rice, DDS, chief editor of DentistryIQ.
Social media has given rise untold trends over the years, both good and bad. Among the decidedly questionable is the uptick in DIY dentistry, particularly since the start of the COVID-19 pandemic.
Here are six home dental practices that range from probably not effective to downright dangerous.
1. Using DIY dentures

A quick Google search on DIY dentures will pull up websites touting assemble-at-home dentures as affordable alternatives to the real deal. But this is one case where you get what you pay for: the cheap materials used in homemade dentures make them an esthetic mishap; worse, they can impede chewing and cause pain in the mouth and jaw.
2. Straightening your teeth
Rubber bands, dental floss, fishing line, paper clips—they all have their purpose, but that purpose isn't straightening your teeth. Why not? Because dentists use a very precise amount of force, in very precise locations to move your teeth through your bone. Trying to achieve this yourself can result in teeth breaking, gum damage, and even tooth loss.
3. Using charcoal as a whitener

A charcoal and baking soda combination has gained popularity as an effective at-home whitener, but dentists don’t understand why: there is no evidence that shows charcoal is effective, let alone safe for the teeth.
4. Filing teeth to reshape them
Early on in the pandemic, filing teeth was among the dental trends popular on TikTok, with one poster saying “A lot of people started cutting their own hair, I became my own dentist” about the practice. Teeth-filing is dangerous in ways those thinking of doing it might not realize: grinding down the enamel and alters tooth structure, making it easier for cavities and nerve damage to develop.
5. Whitening with Magic Eraser
Briefly rubbing a sponge over the teeth to whiten them sounds harmless enough, right? Wrong—Magic Eraser-type sponges are made from Melamine foam, which contains chemicals that become abrasive when wet. If you have any remaining doubts about the practice, just read a Magic Eraser box. The health and safety warning reads, “Do not use on skin or other parts of the body”—including the teeth.
6. “Oil pulling” for oral health
The practice of oil pulling—swishing oil in the mouth to remove bacteria or whiten teeth—is no social media trend; it’s been around since ancient times. And unlike some of the more recent trends, there’s little actual danger to the practice. But there may also be little point: According to the American Dental Association (ADA), currently there are no reliable scientific studies to show that oil pulling reduces cavities, whitens teeth, or improves oral health and well-being.
(01/04/2024)by Dentistry IQ
More Information: https://www.dentistryiq.com/personal-wellness/article/14286506/the-6-list-at-home-dental-trends-to-avoid
Views: 349
Chronic Bad Breath? You May Need to Visit the Dentist
Embarrassed by chronic bad breath? Breath fresheners can be an effective short-term fix.
But if bad breath persists despite a regular brushing and flossing regimen, it’s best to see your dentist for an exam.
What Causes Bad Breath?
Bad breath, or halitosis, is an embarrassing problem that could signify a more serious medical issue, especially if you’re already practicing good oral hygiene.

The tongue harbors many bacteria, which are normally kept in check by saliva. However, an excess of bacteria can form plaque on your teeth and gums—producing plaque and volatile sulfur compounds that cause bad breath.
Risk factors for bad breath include:
Smoking or chewing tobacco
Poor oral hygiene

Dry mouth due to medications
Gingivitis or periodontal disease
Medications that interfere with saliva production (antidepressants and antihistamines are common offenders)
High-protein diet
Good Oral Health is Essential for Overall Health
Maintaining good oral health is essential for overall wellness.
Teeth and gums are vulnerable to decay, periodontal (gum) disease, tooth loss, and oral cancers. You can prevent many problems with regular visits to your dentist for exams, cleaning, and x-rays.
The American Dental Association recommends these steps for good oral health:
Brush your teeth twice a day with fluoride toothpaste. Use an ADA-approved soft-bristled brush. Floss once a day unless your dentist tells you otherwise.
If you have gingivitis or periodontal disease, floss at least once a day and brush after meals whenever possible.
Visit your dentist regularly—at least twice a year—for checkups and professional cleanings. You may need professional cleanings more often If you have problems with your gums or periodontal disease.
If you use tobacco products, stop. Smoking increases the risk of developing oral cancer and causes bad breath, stained teeth, and mouth sores.
If you drink alcohol, do so in moderation (no more than one drink per day). Excessive alcohol consumption can damage the tissues of the mouth.
Common Signs of Dental Problems
Many people don't realize that their oral health is an important factor in maintaining overall health. A healthy mouth can help prevent severe conditions such as heart disease, stroke, and cancer—not to mention periodontal disease that can lead to tooth loss.
Some signs of dental problems are obvious, such as bad breath or pain when chewing.
These are common signs of dental problems:
Bleeding gums. Bleeding may be a sign of gum disease caused by plaque. Left untreated, gum disease will worsen and may eventually lead to tooth loss and other problems.
Swollen or discolored gums. If you notice any changes in your gums, see your dentist. Changes in gum tissue may indicate a more serious problem.
Bad breath (halitosis). Bad breath can occur when your teeth decay or become infected. Halitosis can be eliminated with proper treatment for any dental problems.
Tooth pain or sensitivity. See your dentist if you’re experiencing persistent tooth sensitivity or toothaches.
Embarrassed By Bad Breath? Schedule an Appointment Today
Good oral hygiene can help prevent embarrassing bad breath, but you should see your dentist if the problem persists.
A dental cleaning removes plaque and reduces your chances of developing cavities and gum disease that can lead to bad breath. Routine dental exams are the best way to protect your smile, so schedule an appointment today!
(01/02/2024)by Dr. Todd Paczewski
More Information: https://www.drtoddsmileon.com/chronic-bad-breath-you-may-need-to-visit-the-dentist/
Views: 376
Your Tongue Is Probably Filthy, Here’s How to Clean It
I’d like to think I’m pretty on top of my oral hygiene. I brush my teeth twice a day every day. I also try to stick to experts’ recommendation that I brush for a full two minutes every time.
But until recently, even I, Two-Minute Tooth Brushing Girl, was missing a crucial component from my oral hygiene routine: I wasn’t cleaning my tongue. As it turns out, brushing or scraping your tongue may help you get rid of grody bacteria that can cause bad breath.
Though the American Dental Association says brushing your tongue isn’t a necessary step for good oral health in the same way brushing your teeth and flossing are, some evidence shows it can help tame breath that reeks. At the very least, it might make your mouth feel really clean. Here’s why cleaning your tongue can be a good idea, plus the right way to do it, if you’re so inclined.
Your mouth is full of bacteria, but that’s not automatically a problem. In fact, it’s a good thing for your oral hygiene.

Though tons of bacteria are hanging out in your mouth at any given moment, most of them aren’t harmful, Lisa Simon, D.M.D., an oral health and medicine integration fellow at the Harvard School of Dental Medicine, tells SELF. It seems completely counterintuitive, but many bacteria in your mouth protect you by keeping out foreign organisms, like disease-causing pathogens, Philip Tierno, Ph.D., director of clinical microbiology and diagnostic immunology at New York University Medical Center, tells SELF.
The problem is that even though most of the bacteria in your mouth is doing you a solid, sometimes it doesn’t smell great.
A lot of the bacteria living in your mouth are anaerobic, meaning they don’t need oxygen to survive, Dr. Tierno says. These anaerobic bacteria—including the ones on your tongue—can produce various byproducts, including sulfur compounds, which can smell like straight-up trash.

How bad the sulfur smells will vary, Sally Cram, D.D.S., a periodontist based in Washington, D.C., tells SELF. For example, if you’ve eaten recently, bad breath can get way more pronounced because anaerobic bacteria can feed on food debris, break it down, and release those smelly sulfur compounds.
Having a dry mouth can also make the smell more severe, Dr. Cram says. This can happen if you’re dehydrated or if you have the aptly named condition dry mouth. Saliva neutralizes bacterial acids and limits bacterial growth, according to the Mayo Clinic, so when your spit is running low, bacteria may be able to cause more of a smell.
The bacteria that causes bad breath is usually non-pathogenic, meaning it’s not harmful or disease-causing, Dr. Tierno says. But sometimes, bad breath could mean you have an infection, like gum disease, aka periodontitis. If your bad breath is accompanied by symptoms like swollen gums, bleeding gums, loose teeth, or painful chewing, you should talk to your dentist.
Now, how do you actually clean your tongue? Grab a tongue scraper or toothbrush and get to work.
Cleaning your tongue is pretty easy, Vera Tang, D.D.S., a New York-based dentist, tells SELF. You can either use a tongue scraper or toothbrush once or twice a day after brushing your teeth.
If you have a strong gag reflex, Dr. Tang recommends you use a tongue scraper, because it’s flatter and may feel less intrusive than a toothbrush. But if you’d rather not spring for a tongue scraper, you can use the same toothbrush you use on your teeth every day. Since your tongue and teeth touch all the time and share a ton of bacteria, you don’t need a separate toothbrush to clean them, Dr. Simon says.
Once you have your tool of choice, you’ll want to stick your tongue out as far as you can, Dr. Tang says. Then reach to the back of it and scrape outward to the tip. Be careful not to press too hard—you don’t want to cut your skin. Just apply gentle pressure, rinsing the scraper or toothbrush off after each pass to avoid re-depositing all that crud back on your tongue.
If your gag reflex is giving you trouble, you can try humming to distract yourself while you do this, Dr. Tang says. You can also try not extending your tongue as much.
If you’d rather not come face-to-face with all the stuff hanging out on your tongue, you can just use mouthwash instead. You can opt for a cosmetic mouthwash, which can basically mask bad breath, or you can go for a therapeutic one that’s actually meant to control bacteria that can cause bad breath, tooth decay, and other oral hygiene issues. Therapeutic mouthwash is available by prescription and over the counter. Here’s more information on figuring out which kind of mouthwash makes sense for you.
Whether you use a toothbrush or tongue scraper to clean your tongue, make sure you can’t see any matter on it when you’re done.
All you have to do is rinse it off the same way you’d rinse off a toothbrush, Dr. Cram says. If you want to go the extra mile, you can dip it in some mouthwash, as well.
You should be replacing your toothbrush every three or four months, so if you’re using a designated tongue scraper, you can grab a new one that often, too. The only exception is if you’re sick, whether with a cold or some other kind of infection. You’ll want to get a new toothbrush and tongue scraper to start from a clean slate, Dr. Simon says.
If you’re wondering whether you’ve cleaned your tongue well enough, its color might be a clue.
Remember, clean doesn’t mean 100 percent bacteria-free. “Most people’s tongues and mouths are dirty, but that’s a totally normal thing for your mouth to be,” Dr. Simon says. Still, if you want to know whether or not your tongue-cleaning efforts have been successful, check out your tongue in the mirror. It should be a fleshy pink color, Dr. Cram says.
If it looks black and hairy, white, or any other color besides pink, that probably just means there’s a buildup of debris on your tongue that you can clean off using the above method. See a dentist if the fuzziness or abnormal color persists despite regular cleaning.
Once you’ve stuck out your tongue, given it a once-over, and signed off on its fleshy, pink appearance, you’re good to go. Feel free to repeat the process daily, or just whenever your tongue takes on a weird color, or your mouth feels a little dirtier than usual. Your tongue (and the people you talk to) will thank you.
(01/01/2024)by Lindsey Lanquist
More Information: https://www.yahoo.com/lifestyle/tongue-probably-filthy-clean-120000507.html
Views: 351
Does flossing make teeth thinner?
Flossing is known as a safe and effective oral cleaning method, but it is not commonly used in Vietnam. Therefore, issues related to flossing such as "does flossing make teeth thin" or "when to floss"... are all very new. This article will answer the above questions in detail for readers.
1. Flossing and recommendations from a dentist
Food plaque on teeth when persisted for a long time can lead to periodontal disease and the serious consequence of this problem is tooth loss, if left untreated. Therefore, it is extremely necessary for everyone to protect and clean their teeth from the residence of these plaques.The American Dental Association has long stated that flossing is essential to taking care of your teeth and gums. Dentists also believe that repelling the growth of bacteria and plaque through brushing and flossing will ensure your teeth are always clean, thereby minimizing the risk of gingivitis - something conditions that can lead to periodontal disease.
2. Why use dental floss instead of toothpicks?

Vietnamese people are often more familiar with toothpicks than floss when they want to remove food stuck in between their teeth. However, the use of toothpicks, in the opinion of dental experts, is a bad habit for oral health. Toothpicks have the potential to cause damage to teeth and soft tissues. Moreover, the use of toothpicks also causes the interdental spaces to become thinner, which looks unsightly.At this point, flossing is the most optimal solution. This dental hygienist is recommended by every dentist every day. Because of its soft, thin and chewy structure, floss easily penetrates into many nooks and crannies of the teeth, even the narrowest of teeth, helping to thoroughly clean daily plaque and food debris.
3. Does flossing make teeth thinner?
A lot of people, for cosmetic reasons, question whether flossing will make teeth thinner. The answer from dental professionals is no, if you use dental floss correctly. This is also an outstanding advantage that makes dentists recommend using dental floss instead of daily toothpicks.However, in some cases, if you do not choose the right type of quality dental floss with a large size, the use of these floss will cause teeth to become sparse after a while. So, if flossing properly; Choosing quality silk thread with thin, soft, smooth but high durability will not thin teeth but still achieve absolute cleaning effect.
4. How often should you floss?

In order to determine if flossing can make teeth thinner, the factor of frequency of flossing is also taken into account. Flossing too much can also cause tooth decay because you're constantly flossing between your teeth. So how often is it reasonable to use dental floss?So far, there is no exact conclusion about the number of times to use dental floss per day. However, the formation of plaque in the mouth takes place continuously. Along with that, bacteria will take about 4-12 hours to grow on plaque. So flossing more than once per day won't be as beneficial. As recommended, this will cause serious damage to gum tissue if you floss the wrong way, exposing the roots more. Not only that, this also creates an opening for bacteria to enter and cause tooth decay.In short, you can floss once a day and up to 3 times a day if you feel food stuck between your teeth after eating.
(12/30/2023)
by Vinmec International Hospital
More Information: https://www.vinmec.com/en/news/health-news/general-health-check/does-flossing-make-teeth-thinner/
Views: 390
Four Dental Hygiene Mistakes That Can Harm Your Oral Health
Home dental hygiene serves as your first line of defense against common dental and oral diseases. Between those important professional dental.
exams and cleanings, your home care practices can minimize plaque accumulation and help maintain strong tooth enamel.
However, even the most careful and concerned individuals can do more harm than good if they pursue their dental hygiene regimen incorrectly. If you want to get the most out of your everyday oral wellness efforts, eliminate these four dental hygiene mistakes from your routine and replace them with healthier alternatives.
1. Tooth Brushing Technicalities

Many people think of tooth brushing as a mundane activity that doesn't merit any special thought, brushing their teeth in whatever manner they learned in childhood or using whatever technique seems to remove food particles. Unfortunately, incorrect tooth brushing can make you more vulnerable to dental problems.
Aggressive brushing can harm your mouth in multiple ways, especially if you compound this error by using a firm-bristled toothbrush instead of a gentler soft-bristled model. The excessive force can contribute to enamel loss, making your teeth hypersensitive, while also causing your gums to recede and expose the tooth roots.
If you scrub your teeth with a simple back-and-forth motion, you may clean the tooth surfaces without also removing plaque from the gum line. This error allows bacteria to trigger inflammation and periodontal disease. Placing the toothbrush at an angle and gently sweeping vertically, away from the gum line, yields better results.
2. Flossing Errors

Flossing complements brushing in your dental hygiene regimen by removing debris between teeth and near the gum line that a toothbrush can't easily reach. However, this practice can be ineffective or even destructive if the wrong technique or product fails to remove food particles and/or irritates your gums.
Start by making sure that your choice of dental floss suits you. For example, if you have unusually tight spaces between your teeth, you may miss certain spots, which then develop tooth decay or gum disease. Ask your dentist whether you should purchase a particular type of extra-thin floss.
Don't make the mistake of scrubbing your teeth with the floss or jamming the floss down into your gums. A rough flossing technique can cause gum irritation and bleeding without providing any special benefits. Always floss gently and carefully, moving the plaque away from the gum line and out of the teeth without pressing on the gums.
3. Mouth Rinsing Problems
You'll find a wide range of mouthwashes available to help you rinse out your mouth and freshen your breath. Some mouthwashes boast ingredients known to kill oral bacteria, giving you additional protection against gum disease and tooth decay. Even so, you should choose your products carefully and use them wisely.
Some mouthwashes include alcohol as their antibacterial ingredient. Although the American Dental Association has deemed alcohol-based mouthwashes safe and effective, alcohol can also raise your risk for oral cancer. Consider alternating an alcohol-based mouthwash with non-alcoholic alternatives to minimize this risk.
Even water can rinse out your mouth to a useful degree by helping to dislodge or dissolve bits of food debris. If you have just brushed your teeth, however, you may want to wait a few minutes before rinsing with water. If you rinse immediately after brushing, you'll remove beneficial traces of fluoride from the toothpaste prematurely.
4. Insufficient Fluoride
Speaking of fluoride, your choice of toothpaste, oral rinse, and even everyday water can either help or hurt your dental hygiene. Cities typically add fluoride to tap water due to its ability to help support strong bones and teeth. However, not every toothpaste or other oral care product includes this vital ingredient.
Always read the label to make sure you buy a toothpaste that includes sodium fluoride as its active ingredient. If you prefer a toothpaste that doesn't contain fluoride, accompany it with an oral rinse that does. When you rinse your mouth with water, use tap water instead of bottled water.
(12/20/2023)by Carlino And Paton, DDS
More Information: N
Views: 405
What Is The Difference Between Stomatology and Oral Medicine?
You're a devoted dental patient who attends all your regularly scheduled checkups, commits to a vigorous oral care routine, and replaces your toothbrush when it begins to fray. Still, you may not be aware of how much your oral health relates to your overall health and how the understanding of this connection has developed. While we believe that taking care of your mouth is essential for the upkeep of your teeth, gums, and gorgeous smile, it's also related to your physical wellbeing.
In some countries, the original term for this field, "stomatology," is used instead of oral medicine. But it's not a term you're likely to see on your dental professional's office door in the United States. Stomatology has evolved into oral medicine as a recognized dental specialty in the United States. Its specialists fill an essential role in training dentists and treating various health problems that affect the mouth and teeth. Let's go over the details of oral medicine, its evolution from stomatology, and the specific diseases this field diagnoses and treats.
Regulating Dentistry
We consider the American Dental Association (ADA) the premier governing body of dentistry in the United States. The ADA determines what fields of dentistry should be specialties. There are currently twelve specialties, ranging from dental public health to pediatric and surgical disciplines.

In September 2020, oral medicine was added as one of these specialties. Its representing organization in the United States is the American Academy of Oral Medicine (AAOM), founded in the 1940s out of an understanding that there should be an integrated approach to studying medicine and dentistry. This made the study of the relationship between oral health and other ailments of the body, also known as oral-systemic health, official!
What is Oral Medicine?
As noted by the ADA, oral medicine is "the specialty of dentistry responsible for the oral health care of medically complex patients and the diagnosis and management of medically-related diseases, disorders, and conditions affecting the oral and maxillofacial region." Oral medicine training in dental school focuses on few key areas:
The management of dental patients who present with complex medical conditions

Nonsurgical management of oral manifestations of systemic diseases (examples include HIV/AIDS, lupus, and diabetes)
Diagnosis and management of acute and chronic oral mucosal lesions and disorders (examples include candidiasis and leukoplakia)
Other oral conditions not associated with the teeth
Oral medicine specialists play an essential role in the field of dentistry. They examine patients and determine both the diagnosis and course of treatment. They also perform biopsies and consult with many other medical and dental specialists, depending on the patient's health issue and treatment needs.
Diseases That Affect the Mouth
Some systemic diseases such as diabetes, HIV/AIDS, and lupus may have oral manifestations. When these diseases result in dental issues, their diagnosis and management would be an oral medicine professional's responsibility. While not related to the oral cavity in nature, some conditions or treatments need monitoring from an oral care perspective. For example, if you undergo cancer treatment, you'll need special oral care because some cancer treatments can result in oral mucosal lesions and pain.
Did you know that oral medicine also covers oral cavity ailments that aren't yet completely understood? A burning tongue, sores, ulcers, sensory disorders, taste disorders, movement disorders, and chronic pain are just some of the areas that can be part of the oral medicine discipline. There's ongoing research on these ailments to understand their interconnectedness with the rest of the body and potential causes.
The Future of Oral Medicine
Because healthcare providers see the benefits of working from a more comprehensive care perspective, the future of oral medicine looks bright. Eventually, the practice of oral medicine will expand on a global level as specific populations age. Their chronic health issues will need a multi-disciplinary care approach. Physicians, dental professionals, and other healthcare providers will work in an interdisciplinary manner to improve their patients' quality of life.
We may come to learn that many health issues don't work in a vacuum. The connection between oral and systemic health is becoming better understood in no small part because of the field of oral medicine, known for years as stomatology. This oral-systemic link is what makes oral medicine essential to both the dental and medical fields of study in the United States. So when you partake in your rigorous oral care routine and attend your scheduled professional dental appointments, you're not only taking care of your dental health but your overall wellbeing too!
(12/19/2023)by Colgate
More Information: https://www.colgate.com/en-us/oral-health/adult-oral-care/what-is-stomatology#
Views: 425My BEST Dentists Journal Headlines

