Dentists Journal
Top Ten Stories of the Week
11/30/2024
All Dentists Journal · Previous Week · This Week · All Time List · Headlines

What Is A Gumline Cavity?
If you’ve recently joined the cavity club or are worried you may be a future member, know that you’re not alone. Tooth decay is so common that the Centers for Disease Control (CDC) report that it affects nine out of ten people over the age of 20. While receiving a cavity diagnosis is never the ideal experience, it’s important to learn about the common causes, treatments and prevention tactics that can help stop it from worsening or lessen the risk of future cavities.
Causes of Gumline Cavities
A dental cavity forms when plaque, a sticky bacterial film that builds up inside the mouth, solidifies and creates an area of decay. This bacteria combines with sugar to produce acids that dissolve the tooth's enamel, the hard surface that works as a protective layer against tooth decay. And when this protective layer begins to wear, different types of cavities have the potential to form.
Have you ever wondered what areas of the mouth are most prone to tooth decay? Well, not all teeth are created equal. Plaque tends to accumulate more easily in certain areas. For example, the back teeth' pits and fissures (molars) are a hot spot for plaque and the spaces in between the teeth. Plaque also builds up easily along the gumline, and when this plaque isn't removed, a gumline cavity can form.

Gumline cavities can also be associated with exposed tooth roots. Gum tissue usually protects the roots, but the roots will be vulnerable if the gum tissue recedes. That's because roots are covered in a material called cementum, which is much weaker than tooth enamel.
Treatment of Gumline Cavities
As outlined by Mayo Clinic, there are several standard treatments for cavities, the most common, a filling. To create a filling, a dental professional numbs the surrounding area of the problematic tooth, drills, or lasers to remove the decayed material, and then fills in the hole with a protective material like composite resin or dental amalgam.
Tooth decay at gumline treatment is similar to other cavity treatments, but with some small differences. If the cavity extends beneath the gumline, it can be challenging for the dental professional to access it with their drill or laser. In these situations, your dentist may perform minor gum surgery to access the cavity.

How to Prevent Gumline Cavities
Toothbrushing
While there's no such thing as guaranteed gumline cavity prevention, you can take daily, consistent steps to fight them. The best way to prevent cavities is to brush your teeth at least twice a day. Remember to brush along your gumline with a proper brushing technique that involves placing your toothbrush at a 45-degree angle to your gumline and using a back-and-forth motion to brush along each tooth. Once the gumline area is clean, move on to the rest of the tooth surfaces for complete cleaning.
Interdental Cleaning
For the hard-to-reach plaque around your teeth and gumline, a daily routine of flossing will also help to prevent cavities. To floss beneath your gumline, curve the floss around each of your teeth' base and make sure to be gentle to avoid cutting or bruising the gum tissue. Water flossing is an excellent alternative to flossing, while mouthwash should also be added to your daily oral health routine to rinse out bacteria.
Professional Teeth Cleanings
And like all preventative health measures, a regular dental checkup is paramount to your overall oral health. A dental professional can thoroughly clean your teeth and remove plaque and tartar from along the gumline that you could not remove with your at-home measures. They can then thoroughly examine your mouth and look for conditions like gum recession that could put you at risk of gumline cavities.
No one enjoys receiving the news of a cavity at the gumline diagnosis. Still, the more you know about this specific type of tooth decay - its causes, prevention, and treatment - the more confident you'll feel with whatever next steps your dental professional recommends. With an excellent oral hygiene routine and help from a dental professional, you can reduce the chances of a gumline cavity or proactively treat it if recently diagnosed.
(11/22/2024)by Colgate
More Information: N
Views: 416

Can an Electric Flosser Make Flossing Easier?
“Do you floss regularly?” That is a question everyone has heard, and it usually takes place while you’re sitting in the dental chair. Head tilted back. Mouth wide open.
Flossing (also referred to as interdental cleaning) is an absolute must for the wellbeing of your overall oral health. It’s also something people tend to forget or just don’t want to do. Here, we’ll tell you about the electric flosser and how it may just be a flossing game changer for you.
Types of Electric Flossers
Water flossers and air flossers are two types of electric flossers available. Both clean between the teeth and around the gumline. This is what makes them different:

Water flosser produces a stream of water
Air flosser uses jets of air containing tiny water droplets
How Do Electric Flossers Work?
Both flossers operate with a motor or pump that pushes water into a reservoir. From there, the water goes through the flosser tip. Flossers work by sending steady pulses in between the spaces of your teeth. The pressure of the stream loosens and rinses away food particles, debris, and plaque from in between your teeth.

There are battery-operated flossers that you plug in to charge. The other flossers need to be plugged in while using.
Are Electric Flossers As Effective as Traditional Floss?
If you struggle with or don’t like traditional flossing by hand, electric flossing is the way to go. According to the ADA, flossers are considered an excellent way to clean between your teeth. They even list ones that have their seal of acceptance. This means the ADA found them to be safe and effective in removing plaque and fighting gingivitis.
Who Benefits From Electric Flossers?
String floss can be tricky, especially if you have braces, dental bridges, or arthritis. According to the ADA, electric flossers are a good option for people with dental work or difficulty flossing by hand.
Flossing is an essential part of your oral care routine. Cleaning between teeth after each meal is instrumental in removing plaque and keeping gingivitis and periodontal disease under control. If you are happy flossing by hand, that’s great. Keep it up! However, if you’re someone who isn’t flossing because you find it difficult or you don’t enjoy it, consider using an electric flosser. Talk it over with your dental professional. They will help you find what’s best for you and your oral health.
(11/22/2024)by Colgate
More Information: N
Views: 334

What causes receding gums?
Gum recession, also known as gingival recession, occurs when the margin of the gum tissue surrounding the teeth wears away, exposing more of the tooth surface. This can happen for a number of reasons:
Gingivitis and periodontal disease
The most common cause of gum recession is due to gingivitis, an early stage of periodontal (gum) disease. When plaque (a sticky film of bacteria) builds up along and under the gumline, it can cause inflammation and irritation, making the gums swollen, reddish in color, and prone to bleeding easily when brushing or flossing.
Over time, this chronic inflammation damages the gum tissue and causes it to slowly detach from the tooth. This creates spaces known as periodontal pockets, where more bacteria can accumulate. As the disease advances, the pockets deepen and more gum tissue is destroyed, leading to loosening of the gums and eventual exposure of the tooth roots.
Aggressive brushing
Brushing too vigorously or with improper technique can eventually cause the gums to recede. Scrubbing back and forth vigorously or brushing horizontally with pressure can wear down the gum tissue. Ideally, brushing should be done at a 45-degree angle towards the gums, using gentle circular motions. Harder bristled toothbrushes may also irritate and traumatize the gums over time, causing sensitivity and recession.

Smoking and tobacco use
Smoking and chewing tobacco have been strongly linked with higher rates of gum disease and accelerated gum recession. The multitude of toxins and chemicals in tobacco products can irritate and inflame the gum tissue. They also suppress the immune system, restrict blood flow, and slow down the healing response.
Additionally, the nicotine causes gum tissues to become more permeable and prone to bacterial invasion. Smokers tend to have much more tartar and plaque buildup as well, which exacerbates irritation of the gums. The stains can also make gum issues harder to recognize visually.
Clenching and grinding teeth
People who have a habit of forcefully clenching, grinding, or chomping their teeth are at higher risk for increased gum recession. The excessive forces exerted during these behaviors can cause teeth to move and shift out of alignment, often putting more pressure on the gum tissue surrounding the teeth. Over time, this can definitely cause the gums to recede.

Periodontal surgery
Certain surgical procedures to treat advanced gum disease can cause recession as well. For example, gingivectomy is performed to excise excessive diseased gum tissue in order to reduce deepened periodontal pockets. This can sometimes leave areas of root exposure once healing is complete.
Orthodontic treatment
The movement and adjustment of teeth during orthodontic treatment can in some cases contribute to gum recession. Certain types of aggressive tooth alignment and prolonged pressure can create tension on the gum tissue. This is especially true if proper oral hygiene is not maintained during treatment. Inadequate bone support around the teeth can also predispose gums to recession.
Thin gingival tissue
Some people simply have thinner gum tissue genetically that is more vulnerable to recession even without inflammatory disease. Thin gingiva offers less protection for the deeper structures of the periodontium. There is a reduced barrier against the accumulation of bacteria and easier penetration of bacterial toxins.
Genetics
Research suggests that genetics play a definite role in gum recession as well. Some people may be predisposed to thinner tissue, insufficient keratinized gingiva, or gum anatomy that is more susceptible to recession. Other genetic traits related to connective tissue disorders, anti-inflammatory response, and wound healing may also influence risk.
Orthodontic tooth extraction
Extracting teeth for orthodontic purposes can potentially lead to gum recession as well. This is especially true of premolar extractions, where gums and bone may thin over time near the extraction sites. Proper treatment planning is important to avoid this consequence.
Overly aggressive gum surgery
In rare cases, gum surgery to treat periodontal disease may be too aggressively performed, removing more tissue than necessary. This can result in receding gums due to insufficient gingiva remaining to provide adequate coverage.
Why does gum recession matter?
Receding gums are a concern because they can expose the tooth roots and lead to further problems:
Tooth decay – Without the protective covering of gum tissue, exposed tooth roots become much more vulnerable to invasion by decay-causing oral bacteria. Plaque and tartar can readily adhere in these areas, leading to cavities.
Tooth sensitivity – Once the cementum layer of the root surface is exposed due to receded gums, the openings to underlying dentinal tubules become exposed as well. This allows hot, cold, or acidic foods to stimulate the nerves and fluid within the tubules, causing sharp pains and sensitivity.
Destruction of bone – The fibers of the periodontal ligament that attach the teeth to the surrounding jawbone can also become exposed and irritated. This bony attachment is damaged, leading to inflammation and gradual loss of the alveolar bone around the tooth.
Tooth loosening or loss – As bone recedes away from the root surface due to infection and inflammation, teeth can become loose and even fall out in severe cases of gum disease. Mobile teeth make chewing difficult and undermine dental function.
Poor aesthetics – Increased tooth length and dark triangular spaces between teeth due to gum recession can give your smile an unappealing “toothy” or uneven look. Receding gums accentuate the aging process.
Root cavities – Once gum recession occurs, cavities at the gumline and beneath the gums can form. These subsurface lesions are more difficult to detect, treat, and restore.
Keeping gum recession under control is extremely important to minimize the risk of these undesirable consequences. Mild cases can often be treated and stabilized to prevent any further progression of the recession. More advanced recession may require complex grafting procedures to cover substantial areas of exposed root surfaces in an effort to regrow some of the lost gum tissue for both functional and aesthetic reasons.
Why does gum recede between teeth specifically?
Gum recession can occur anywhere around the teeth where gingival tissues have broken down, but it is most prevalent in the areas between the teeth (interproximal areas). There are several reasons this occurs frequently in these locations:
Difficult to access for cleaning
The tight embrasures and small spaces between teeth provide ideal areas for plaque to accumulate and thrive. Food debris and bacteria can readily get trapped in these interdental spaces, which are harder to access and keep clean compared to broader facial and lingual tooth surfaces. Lack of adequate cleaning in these areas allows plaque to proliferate.
Inflammation and tissue destruction
The anaerobic bacteria in plaque produce toxins that break down gum tissue fibers and cause inflammation. recurring episodes of inflammation due to poor cleaning within the gingival crevice can lead to irreversible destruction. The cellular attachment of gum to tooth is lost, resulting in recession.
Food packing
Bits of food readily get packed into the tight spots between teeth during eating and chewing. They then become impacted and are difficult to dislodge completely. This constant source of irritation inflames the localized area and promotes sustained bacterial colonization in that vulnerable site.
Weak gingival embrasures
Some individuals are prone to having weaker, thinner gum tissue between their teeth based on certain anatomical factors. The size, shape, and position of the interdental bone and contacts predispose the gum to easier breakdown and recession even with diligent oral hygiene.
High muscle attachment
A stronger, more forceful muscle attachment near the crestal bone places increased stress on the gingival margin. The pull of muscle forces during chewing can contribute to more rapid localized tissue breakdown in those high stress areas. This is often seen between back molars.
Orthodontic factors
Teeth that are crowded, crooked, or overlapped can create areas where cleaning and maintenance of gums is impaired. Physical impediments make hygiene access difficult. Orthodontic treatment to straighten and align teeth also puts tension on gum and bone tissues in between teeth.
Periodontal disease progression
As gingivitis and periodontitis progress, collagen fibers that attach the gums to the tooth surface are steadily destroyed by proteolytic enzymes from bacteria. The initial gingival inflammation increasingly destroys the gingival margin until the gum detaches from the tooth. The interdental papilla is often the first affected area.
With meticulous oral hygiene and professional care, gum recession between teeth can often be minimized or avoided altogether. But in moderate to severe cases, surgical procedures like gum grafting are usually needed to try to cover exposed roots and regrow healthy gingival tissues between teeth. The adjacent teeth provide scaffolding for the graft to adapt and heal optimally.
What are the treatment options for receding gums between teeth?
Here are some of the key treatment approaches available when gums are receding between teeth:
Improved oral hygiene
Practicing thorough daily oral hygiene is crucial both for treating and preventing receding gums between teeth. Effective hygiene to control plaque is the starting point in managing gum recession. This includes brushing properly twice per day with a soft or extra soft bristled brush. Flossing once daily with light force is critical to dislodge plaque between teeth. Using antiseptic mouthwash can reduce bacteria as well.
Professional cleanings
Getting teeth professionally cleaned and scaled by a dental hygienist every 6 months is key to controlling subgingival plaque. More frequent cleanings may be prescribed if gum disease is present. Regular cleanings allow areas like interdental spaces to be cleaned beyond what patients can do at home.
Gum tissue grafting
Grafting gingival tissue can help cover exposed tooth roots and fill in the receded areas between teeth. Tissue is commonly harvested from the palate and surgically adapted into place around the recession defects. Over several months, blood supply re-establishes in the grafted donor tissue. Proper healing provides maintained gum coverage.
Guided tissue regeneration
Using specialized barrier membranes or tissue-stimulating proteins can be combined with grafting procedures. This encourages selective regeneration of bone and gingival attachment fibers along the root surface, helping rebuild lost support around the recession.
Pinhole surgical technique
This is a minimally invasive approach where small “pinholes” are made in the gums. Special tools are used to gently loosen gum tissue and slide it down over exposed roots without grafts or sutures. Less discomfort but results can be variable.
Bone grafting
Bone grafts or tissue-derived growth factors can be placed under the gumline when significant bone loss is present near the recession. This supports regrowth of natural tissue and stabilizes improved gum coverage.
Crown lengthening
When gums have receded substantially, crown lengthening surgery reshapes gum and bone tissue to expose more natural tooth structure. This provides a better foundation for restorative work.
Laser therapy
Lasers have been utilized to remove diseased gum tissue while also promoting healing. Their value for stimulating regrowth is being researched.
Medications
Locally applied or systemic drugs that aim to reduce bacteria and inflammation may be helpful. Locally delivered antimicrobials can suppress plaque in difficult to clean recession areas.
The prognosis for stabilizing or improving gum recession between teeth depends on multiple factors: proper home care, degree of recession, health conditions, and choice of treatment. Mild cases may respond to conservative options, while advanced recession may require a combination of regenerative procedures to optimize outcomes.
(11/23/2024)by CDHP Dental Health Project
More Information: N
Views: 407

Signs Of A Cavity In Between Teeth
You know the importance of brushing your teeth and having good oral hygiene to avoid cavities. But did you know that cavities aren't just in your teeth?
Yes, even when you take care of your enamel, you can still end up with a cavity between your teeth. This has a technical term called an interproximal cavity. It forms like other cavities: when the enamel is worn away and bacteria are able to get into the tooth.
When this happens with your permanent teeth, it can cause tooth pain that you don't want to have to deal with, as well as other problems when the cavity penetrates into the bloodstream.
The Goal is to Keep Your Healthy Teeth Free From Decay

Preventive dentistry is the best way to make sure you don't end up with interproximal cavities and tooth decay. These tips will teach you how to recognize if you have the signs of a cavity in your teeth and how to prevent cavities in general.
Keep in mind that if you're concerned that you may have a cavity, you should contact your dentist early. The sooner the problem is taken care of, the less likely you'll need more serious fixes like a dental crown or root canal treatment.
Understand What a Cavity Is
You've been taught to brush your teeth since childhood to avoid cavities. But what exactly is this dental concern, anyway? And do you really need to floss?

A cavity is an easily preventable dental condition in which the hard surface of your teeth (the enamel) ends up with a tiny hole in it. This permanent damage is caused when the bacteria stick to the tooth.
Cavities Can Be Avoided With Regular Care
As you engage in frequent snacking, eat sugary foods or drink sugary drinks, and don't effectively clean right after, the food particles form dental plaque.
As plaque, bacteria sticks to the enamel and decays the tooth. If you don't remove decay fast, it turns into a hole that requires a large filling to fix it. However, if it's caught early, the enamel could be recalcified with fluoride gel.
Preventing a Cavity
The best way to prevent interproximal cavities and other cavity types, according to the American Dental Association, is to brush at least twice a day.
Use toothpaste with fluoride to get rid of the bacteria, and follow with flossing and a mouth rinse. Fluoride is a commonly added ingredient to most over-the-counter tooth products.
Tooth Sensitivity? Stop What You're Doing and Check Your Technique
If you notice tooth sensitivity, you could be using the wrong brush. Always use a soft-bristled toothbrush unless your dentist recommends otherwise. Brush your teeth in a circular pattern, and include your gums to prevent gum disease.
Habits Are Important, Too
Flossing is important since interproximal cavities form between the teeth, and the floss and mouthwash get up in those hard-to-reach places.
Avoid sugary snacks and drinks, quit habits like using tobacco, and head to your dentist during office hours for preventative cleanings. If you need professional help quitting bad habits, your primary doctor can provide medical advice.
Recognize the Symptoms of Interproximal Cavities
If you're concerned that something isn't quite right, but you're not sure what's going on with your teeth, look for these symptoms to guide you:
Sensitivity to heat or cold- This is usually one of the first side effects you'll notice as the cavity erodes your enamel and gets into the second layer of tissue, the dentin. Once temperatures reach this layer, discomfort is the natural side effect.
Pain in the teeth - Sensitivity is annoying but it goes away. Pain, on the other hand, is different. It's constant, mild to moderate, and often throbbing. It can be hard to narrow down where the pain is coming from because it feels like it's in your other teeth, too. The dentist can take x rays to figure out where the interproximal cavity is.
Bad breath - Officially called halitosis, bad breath is a warning that there's tooth decay going on somewhere. Halitosis is harder to diagnose yourself, but if you know you have it, you want it gone quickly.
Browning or yellowing teeth - When you see dark spots on your teeth, it's not normal. This is a sign that a hole is beginning to form inside the tooth. It can be recalcified with fluoride gel if you catch it before tooth decay becomes a hole. At that point, the dentist can use tooth colored filling material to cover the hole, but it can't be reversed.
Abscesses or pus forming - If you have a weird spot on your gums that is beginning to show pus, it's a sign your cavities have progressed. This means you have to schedule an ASAP visit with your dentist before your interproximal cavity requires a root canal, bridge or dental implant.
Chips - Sometimes, a chip or broken tooth occurs without us realizing it. If you ate something hard or sticky, it could have cracked the top layer. To prevent cavities from destroying the tooth, the dentist can place a natural looking cover over the tooth or add a filling treatment. This keeps plaque from getting into the dentin and causing discomfort. But a chip or crack that isn't treated becomes a serious dental issue, often requiring a root canal to correct.
Head to the Dentist Before You Think You Have a Cavity
So how can you avoid interproximal cavities between two teeth or cavities in general? The best thing to do is to seek out preventative care at least every six months, according to the American Dental Association.
Professional cleanings and dental exams help catch problems early, before cavities can form. And if you do need a filling, the dentist can use a variety of metal alloys to solve minor issues.
Prevention or Early Care, Either Way is a Good Reason to Visit the Dentist
Interproximal cavities form when bacteria is ignored and allowed to run rampant. Head to your dentist for routine visits, and call for an urgent appointment if you think you may have an interproximal cavity or any other dental issues.
(11/23/2024)by Charlotte Emergency Dental
More Information: https://www.charlotteemergencydental.com/blog/signs-of-a-cavity-in-between-teeth/
Views: 358

Why Does the Roof of My Mouth Hurt When I Eat?
There are some common sources to explain why the roof of the mouth hurts and causes you discomfort while you eat. It can have many possible causes, so one should not instantaneously assume the worst-case scenario. Some of the more common issues are discussed below.
Burns & Bumps
Any hot drink or extremely spicy foods can result in burns and bumps forming on the roof of your mouth. The skin on the roof of your mouth or the palate is more sensitive in comparison to that on your tongue. Hence a sore palate is more susceptible to a sore tongue.
A minor burn due to an extremely hot drink or spicy food can damage your soft palate and cause bumps, blisters, or swelling. If such is the case, then it may take about a week for the bumps to settle down. In the meantime, you can choose to eat soft and light foods and drink cool or chilled drinks so that your palate can heal without any further damage.

Canker Sores
Canker sores tend to form on the inside of the cheek and are round and very sensitive, at times though they may also end up forming on the roof of your mouth. They can be caused due to several issues related to the immune system. They may start to develop due to stress, hormonal imbalances, or consuming certain types of foods.
They usually tend to be sore for about a week and go away within two weeks. In the meantime, while they heal, you can consume bland foods to avoid irritating the canker sores. If they extend two weeks, you should pay a visit to the doctor, and your dentist could prescribe a pain-relieving gel to be applied to your sores.
Bump on Roof of Mouth Sinus Infection

Bacterial infections such as common cold, tonsillitis, streptococcal sore throat, sinusitis, and other types of such infections can result in the palate to be sore. The pain may be due to bacteria growth irritating your palate or the sinus pressure pushing on the palate of your mouth. Some fungal infections can also cause pain and redness of the palate.
Causes of Roof of Mouth Bump
The bump on the roof of the mouth can be caused due to multiple varying reasons. Some of the causes are:
Injury
Burns
Hyperdontia
Oral Cancer
Torus Platinus
Cold Sores
Cold sores generally tend to form on the lips but can also find its way to the roof of your mouth. When they form on the roof of your mouth, they can be extremely painful as fluid-filled blisters may also develop. They can be caused due to a virus knows as ‘herpes simplex virus.’
The fluid-filled blisters start to become crusty within four days and start to heal after 8-10 days. You should avoid touching them no matter how sore they become, as that increases the time of the healing process. Cold sores do have the chance of coming back again, so a visit to the doctor may be required to get a long-term medication to get rid of them completely
Variety of Other Symptoms of Pain in Roof Of Mouth
When you are facing pain in roof of the mouth ,you may experience following symptoms:
Itching
Fever
Blistering
Cough
Sore Throat
Runny Nose
Dental Issues
In some cases, when you have recently gotten done with dental treatment, the after effects may include pain around the treated area along with an infection. The infection can then reach the soft tissues on your palate, especially if the treated area includes the top teeth.
In such a case, visiting a doctor is the best option to get rid of the infection and get the proper medication to get rid of the pain.
Oral/Mouth Cancer
Generally, having a mouth sore is harmless and tends to heal on its own. Whereas, in some cases having the constant roof of mouth sores can be a symptom of oral/mouth cancer. It can be treated if found at an early stage. You should visit your dentist if your mouth sore does not heal by itself within two weeks. If your dentist suspects that the mouth sore might be cancerous, you will be sent to an oral surgeon to get an oral evaluation and perform a biopsy of the tissue.
Mouth Cancer can be developed on any part the mouth including:
Gums
Tongue
Roof of Mouth
Floor of Mouth
Lips
If cancer is found, the treatment can start instantly. The treatment may require surgically removing the cancerous sore and after that, getting chemotherapy or radiation to be making sure that other cells are not affected.
Have Some Questions About Roof Of Mouth Sore? Here Is Everything You Need To Know
Why the roof of mouth hurts when I eat after not eating for a while?
Sometimes this feeling is common and if your mouth aches for a couple of seconds or a few more maybe it’s just the salivary gland trying to produce more saliva all of a sudden. Since you haven’t eaten in a long time, your mouth reacts to the surge.
However, if the pain becomes frequent, you need to get it checked immediately as it can be due to buns, acute or chronic infections, dental issues, cold sores, or canker sores. It may also be due to mouth cancers. And in any such case, it is better to get inspected before your condition worsens.
What is incisive papilla and how to get it removed?
It is the projection of the mucous tissue that appears between the upper teeth, two of them. A swollen papilla hurts a lot and is caused due to many factors. Oral hygiene has, however, nothing to do with it. It mostly occurs due to human impact, including consuming food that is sharp or biting the papilla.
Food that is hot or too spicy can also result in the incisive papilla. It can be treated quickly by thorough cleaning of the mouth or utilization of floss in the spaces. Brushing twice in a day and good oral hygiene helps it heal faster.
How to check if I have bumps on the roof of the mouth?
Checking for bumps on the roof of the mouth is an easy task. Most of the time, your mouth lets you know that it’s in trouble. You start to feel something extra in your mouth as your palate has become swollen. It gets hard to eat and drink the stuff without the pain and soon it starts irritating you. Or , you may experience erythema and spots in the mouth.
What is a hard bump on the roof of the mouth?
Bumps can be caused due to problems like canker sores; colored sores that appear on the roof of your mouth. Cold sores, infections, etc. however, torus palatinus is the most common cause and the hard palate is affected in this case. If your bump has not healed after two weeks, you need to see a doctor.
Home remedy to cure lump on the roof of the mouth
Lumps or bumps on the palate are not troublesome in the early days and can be treated at home. Several home remedies to get rid of such problems are:
Drinking as much cold water as you can; it helps get rid of mouth burns. You can also retain the cold water in your mouth for 5-10 minutes sequentially.
Another good option is to consume yogurt or milk (not hot), its proteins help as a barrier and coats your skin.
Utilization of aloe Vera gel is also practiced around the world as it is considered as a natural healing aid.
How to Cure if the Roof of my Mouth Hurts when I Eat Bread?
Eating bread or any other soft item may hurt if your mouth is going through an oral or dental problem including burns, bumps, sores, and infections. If it’s not serious you can cure the pain at home by using honey, milk, or keeping yourself hydrated. It checks your electrolyte imbalance and helps in quick healing. However, if the imbalance is severe, you need to see a doctor.
If your bumps or infections are caused due to trauma cold water can help, but painful blisters demand medical help. You may be advised to use medicated mouthwashes, soft toothbrushes, or other pastes.
Why does the Roof of Mouth Hurt when Swallowing?
Mouth roof, also known as palate may hurt or get sore when you try to swallow things if it’s injured. Damage can be of many forms. For instance, you may have developed a bump or burn due to hot or spicy food. As the palate, soft or hard, is much more sensitive than the tongue, a small burn can lead to a severe bump and become troublesome.
Apart from that, immune deficiencies may lead to the formation of canker sores right inside your cheek area and when it travels to the mouth, you feel pain when swallowing stuff. Dental problems can also lead to sore mouths.
How to Get Rid of Blisters on the Roof of the Mouth Due to Eating?
Mouth sores are irritating and really painful. They are caused by many related and unrelated mouth problems. Whatsoever, once a blister is formed inside your mouth or on the lips, it becomes really difficult to eat or drink something. But with patience and care, it can be treated. If you are unaware of the reason you should try avoiding hot, salty, crispy, and vitamin C food.
Also, items with high sugar content, tobacco, or alcohol should not be consumed. These foods can be acidic and are bad for your oral health. Along with precautionary treatments, you need to apply mouth ointment, gargle with salty water, and should not touch the blisters.
What is the Difference in Lump and Roof of Mouth Sore?
Lumps or mucous cysts occur on the lips or inside the mouth. It occurs when your salivary glands have excessive mucous. The problem is not so painful and is relatively harmless if treated early as compared to mouth sores. The latter results from canker sores, bumps, infections, or other reasons and mainly affect the palate area. Lumps, however, can occur everywhere.
Also, lumps formed on the roof of the mouth may lead to the roof becoming sore. Both can be managed if caught early and can be quite painful if the situations worsen or prolongs. Cysts can become permanent and cancerous if are not handled with care.
Is Blister and Roof of Mouth Burn the Same?
Essentially, they are not the same however are caused due to similar reasons. Mouth burns are usually internal and affect the palates. On the contrary, blisters mostly affect the area inside of the lips but can appear on the outside. As discussed, the set of causes is almost the same for both problems, and, hence, the treatments also converge.
You may avoid eating salty, hot, or edgy food. Also, stay away from food that is rich in vitamin C, sugar, etc. Ointments and mouth gels can help you get rid of both the problems but blisters are more damaging and irritating than the burns. The burned roof of the mouth can be healed fast by different cures.
What Causes Swelling in the Roof of the Mouth?
The swollen palate may result from one of the stated reasons. Cold sores or canker that appear on the gums, lips, and other areas may lead to blistering and swelling of the palate. Many people suffer this fate after eating pointy food that may hurt the soft palate, hot or spicy food resulting in a burn, or through a hard item.
Another common reason is dehydration that leads to electrolyte imbalance in the mouth. It leads to swelling and is usually one of the first indications of dehydration. Lumps, viral infections, or cysts are some of the extreme underlying problems. In any of these cases, you must receive proper medical care.
How do you stop the roof of your mouth from hurting?
Pain in the roof of the mouth can be unbearable and everyone wants some kind of immediate relief from that pain. If you are at home and you face such issue then the best thing you can do for an instance is that you can suck something cold or you can use warm water and rinse. This would make a lot of difference.
Why does the roof of mouth feels bruised?
You may feel that there is a bruise on the roof of your mouth after drinking something very hot or extreme cold. It may also happen due to inflammation or infections.
Why is the roof of my mouth red and hurts?
This is mostly searched by the people who face roof of mouth sore and red. They see some sort of small red spots on the roof of their mouth. The cause of such spots may vary. It might be because of the dentures or some infection and it also might be caused due to irritation from food.
(11/25/2024)by Cards Dental
More Information: https://cardsdental.com/why-does-the-roof-of-my-mouth-hurt-when-i-eat/
Views: 429

Understanding Lip Discoloration: Causes and Treatment
Have you ever noticed that your lips are changing color? This may be due to hyperpigmentation or skin discoloration, which can result from a variety of factors.
Our lips are covered with thinner skin, which makes them more susceptible to the effects of pollution, sun, and aging. They’re also more likely to get darker spots, discoloration, and lesions.
These spots look quite unattractive and can be a cause of embarrassment for you. So how do you bring back your natural lip color? Luckily, there are several treatments available for this problem. Ahead, learn about the sources of lip discoloration and how to treat and prevent it.
What is Lip Discoloration?

Lip discoloration is a condition in which the tips of the lips get tanned or become discolored. This occurs because the skin on our lips is so much thinner that the barrier is not as effective in retaining the moisture needed for healthy-looking and pigmented lips. Certain external factors also contribute to lip hyperpigmentation.
Lip Discoloration Causes
A person can experience lip discoloration due to numerous causes. It can be a result of sun damage, nutritional deficiencies, or an underlying medical condition. Apart from that, various other factors may also become a reason for discolored lips:
Hormonal Changes: Lip discoloration due to hormonal shifts are more likely to impact women with relatively darker skin tones.

Smoking: If you are a chain smoker, then you’re definitely at higher risk of lip hyperpigmentation.
Chemotherapy Treatment: Some sort of chemotherapy treatments can harm the tissues in our lips and may result in lip discoloration. In addition to that, issues like the insufficient amount of hemoglobin and excessive sweating might also lead to darkened lips.
Medical Conditions: Certain diseases, such as dermatitis or jaundice, can leave you with purple or extremely tanned lips.
Excessive Use of Substandard Lipsticks: Daily usage of such products may also contribute to darkened or discolored lips.
Lip Discoloration Treatment
Numerous medical treatments are available for discolored lips that you can opt for depending on the extent of your discoloration, budget, and personal preferences.
These treatment options may also address the underlying condition that causes lip discoloration. However, if your lips are getting darker because of the use of certain medications, speak to your dental professional about going for alternative drugs.
Medical treatments for some skin discoloration usually include:
Laser therapy.
Intense pulse light therapy.
Cryotherapy.
Photodynamic therapy.
Surgery.
Chemical peels.
Topical medicated ointments.
Preventing Lip Discoloration
Depending on the cause, lip discoloration can be prevented through various approaches:
Quit smoking, and if it is difficult, speak with a doctor to get a smoking cessation plan.
Eat a balanced diet.
Limit sun exposure and apply a lip balm having sunscreen in it.
Protect your face and lips from sun exposure as much as you can.
Exfoliate regularly.
Know when to see a professional.
Be gentle with your skin.
When to See a Doctor
Sometimes, severe lip discoloration or pain can be indicative of a serious underlying condition. Therefore, it’s best to seek medical attention if you experience irregularly shaped skin lesions, contusions that do not heal, difficulty breathing, or chest pain.
Key Takeaway
The lips are one of the most noticeable features of our face, so it’s no surprise that we all want them to look the best they can. But due to certain environmental factors and medical conditions, they get discolored and look aesthetically unpleasing.
However, there’s no need to worry. There are various tricks and cosmetic procedures available that can polish the texture and color of your lips.
You can also use topical creams to fade the discoloration of your lips. But nothing can work unless you also apply sunblock on your lips religiously. Remember, taking care of your lips is important for your overall health and hygiene.
If discolored or hyperpigmented lips are due to an underlying medical condition, then it can be a cause of concern. In such cases, consult your healthcare professional. So he can evaluate the actual cause and provide appropriate treatment.
FAQs:
How Can I Fix My Discolored Lips Naturally?
There are several home remedies that you can opt for to restore your hyperpigmented lips. Turmeric, coconut oil, cucumber juice, aloe vera, lemon, honey, and pomegranate powder are some of the most preferred and widespread ingredients that can naturally nourish and beautify your lips.
How Do You Treat Discolored Lips?
After determining the actual cause of discolored lips, doctors can prescribe the most suitable treatment options. If certain medications are darkening your lips, you need to talk to your doctor to be switched to another medicine.
There’s also a wide range of over-the-counter creams and gels available that you can pick to lighten the dark skin around your lips. If none of this works, then you should consider going for medical treatments, such as cryotherapy, light therapy, or surgery.
Is Lemon Good For Lip Discoloration?
Lemon is a natural bleaching agent popular for its incredible skin-lightening properties. Therefore, it can be extremely beneficial in fixing darkened or discolored lips. You can apply lemon and sugar scrub daily on your lips to acquire the maximum results.
With consistent use, it will heal the uppermost layer of your lips and clear away pigmentation, resulting in visibly lighter, soft, and supple lips.
(11/25/2024)by Why Health Line
More Information: N
Views: 480

Lost Gum From Between Teeth
Have you lost gum from between your teeth? If you look at any magazine photo or advertisement you will see cosmetically beautiful smiles with uniform, straight teeth. The smiles you see in these magazines do not have gaps or spaces. If you have tiny triangles between two or more of your teeth, you may feel self conscious about their appearance.
Unfortunately, lost gum between teeth can indicate that the tissue is not as healthy and strong as it should be. Often, gum treatment is needed before cosmetic alterations can be made to fill these spaces. Good oral hygiene is important for your teeth and gums and patients are encouraged to improve how they brush and floss. Once your gums have been treated and are healthy, treatment for the dark spaces can be done. You can say goodbye to these black spaces in your smile through one of three treatment options.
What causes lost gum from between teeth?
In simple terms, space opens between teeth is caused by trauma, receding gums, and gum disease. From a distance, those spaces look like there is food is caught between your teeth. Upon professional inspection, those black spots can indicate a bigger dental problem. You may wish to fill spaces between the teeth for a more uniform appearance.

Gum disease has two distinct stages: gingivitis and periodontitis. The beginning stage of gum problems is gingivitis. Gingivitis is an infectious inflammation of the gums that many people experience at one point or another. It can usually be treated with diligent brushing, antiseptic mouthwash, and thorough flossing at home. Left untreated, gingivitis can progress to periodontitis, a more serious infection can occur. Full blown gum disease will destroy the supporting bone between tooth roots. It can eventually lead to tooth loss.
To get rid of this deeper infection, your dentist will do a deep cleaning called scaling and root planing. During this procedure, they remove plaque and tartar buildup around the roots.
Gum disease causes gum and bone loss
Gum infections will cause loss of the triangular papillae from between teeth. This disease is serious and has also been linked to more than just your oral health. In fact, the bacteria present in this disease can flow into your bloodstream. This is thought to increase the likelihood of developing heart disease, heart failure, dementia, and diabetes. Unfortunately, the damage that gum disease can cause to your body doesn’t end with better brushing habits. After all, periodontal disease isn’t just a lack of oral hygiene. Many pregnant women experience gestational gum problems due to the increased changes in hormones.

Certain medications can also lower your immune system, making your body even more susceptible to illnesses like gingivitis and gum disease. Dental treatments can resolve the disease, yet repairing the lingering damage presents a different matter altogether.
In addition, mild gum recession can be caused by aggressive brushing techniques. Dentists recommend that your regularly brush your teeth with a less abusive soft bristled brush. Use the proper brushing technique to protect your gum tissues and prevent further recession.
Options for replacing the lost gum from between teeth
Your gums need specialized care before the dentist can start fixing the dark spaces. Once any present disease and infection has been cleared, then one of the following procedures may be recommended:
Dental bonding:
Also referred to as composite bonding, dental bonding repairs the structure and appearance of teeth. This technique uses the same resin like composite material that is often used to fill cavities. This commonly performed procedure offers cosmetic solutions that can last anywhere from five to 10 years with proper care and maintenance. Dr. Fondriest will perform a shade analysis to perfectly match the dental bonding to your natural tooth color, for a seamless appearance.
Using bonding instead of veneers to replace a gum papillae is quite difficult. When comparing bonding vs. veneers, replacing the lost gum from between teeth is easier with veneers.
Veneers:
Crafted from very thin pieces of ceramic, veneers act as a type of cover for your front teeth. They can camouflage a host of cosmetic issues in an otherwise healthy, functional dentition. Often old composite veneers are replaced with porcelain. Dental veneers are one of the best ways to improve the cosmetic appearance of teeth in a relatively short amount of time. It often takes just a couple of appointments to receive the veneers to camouflage the host of esthetic issues, including spaces between your teeth. However, due to their custom fabrication and design, ceramic veneers are pricier than other cosmetic treatments. Dental veneers last on average 15 to 20 years before needing replacement. Most clients who choose them feel that veneers are worth it.
Dental crowns can be used to fill space from lost gum from between teeth
Dental crowns are restorations used to protect a weakened or injured tooth. They also are used to correct serious esthetic flaws, when fillings or dental bonding will not suffice. The dental crown is usually made of porcelain, and covers the entire visible area of a tooth. This porcelain “cap” acts as a cover over the vulnerable or unaesthetic natural tooth.
It’s important to note that for each open space, two teeth will need cosmetic treatment. Essentially the root contours are reshaped to close the visible gaps.
An aspect of better quality dentistry is achieving a goal with the least amount of drilling. Crowns and veneers are the two main cosmetic dental options for transforming your smile.
Orthodontic treatment can close space from lost gum from between teeth
Gum disease will often cause recession of tissue from around and between your teeth. The gum between your teeth is called the interdental papillae. Losing the papillae produces the dark space. The black spaces will be more pronounced when your teeth shapes are triangular/trapezoidal in shape. Simply sanding the contact points of crowns to a more square shape will broaden the contact point between the crowns. As the teeth move closer, these spaces close down by pinching the gum papillae.
(11/24/2024)by Dr. James Fondriest, DDS
More Information: https://lakeforestdentalarts.com/lost-gum-from-between-teeth/
Views: 325

What To Do If It’s Been a While Since Your Last Dentist Appointment
It’s no secret that going to the dentist, especially if it’s been a while since your last appointment, can be intimidating. Whether it’s due to a fear of the unknown or financial concerns, people often put off their dental appointments until more serious concerns arise. No matter the reason, Smile Designers hopes you will schedule your next appointment with our family dentistry in Longmont, CO! Here are a few of our tips to make your first dentist appointment in a while a bit easier. Contact us today to schedule an appointment.
Schedule an Appointment As Soon As Possible
If you feel it’s been too long since your last dentist appointment, schedule an appointment with our family dentistry in Longmont as soon as possible. It’s important to prioritize your dental health, regardless of how long it’s been since you last visited the dentist.
Communicate With Your Dentist

Communication is key when it comes to receiving the dental care you need. It’s important to remember that you aren’t alone in putting off your biannual dentist appointments. In fact, according to Delta Dental Institute, 42% of Americans reported that they don’t see a dentist as often as they should. Let your dental care team know when your last visit was and be honest about any concerns you have.
Make a List of Any Questions or Concerns
Before you go to your next dentist appointment, make a list of any concerns or questions you may have. This can help you remember everything you want to discuss with your dentists and ensures you are getting the most out of your dental care.
Know What To Expect

Knowing what to expect can make your dentist appointment less daunting. During your appointment, your dentists will examine your teeth, gums, and mouth to check for any issues. They may also take X-rays, provide a thorough teeth cleaning, and perform any restorative dental treatment needed. Your dentist is there to help you and wants to ensure you’re comfortable, so don’t hesitate to ask questions or voice any concerns!
Don’t hesitate to ask questions or voice any concerns!
If it’s been a while since your last dentist appointment, don’t delay any longer. By taking action now, you’re setting yourself up for a healthier future. At Smile Designers, we’re happy to welcome you back or help you establish a new dental care routine, no matter how long it’s been.
(11/27/2024)by Smile Designers PC
More Information: N
Views: 376

Tooth Pain After a Filling: Is It Normal?
It is relatively common for you to have some pain or sensitivity in the treated tooth after a filling. After all, a dentist was just poking around and drilling in the tooth. Usually, any discomfort should fade after a day or two. Why do some people experience tooth pain for longer than the normal period after a filling? There are many reasons you might feel a bit of pain or sensitivity after a dentist fills your tooth, beyond the normal discomfort.
Malocclusion
One common reason for pain in a tooth after you get a filling is that the filling isn't positioned quite right, and it's interfering with your bite. A filling that is too high can cause malocclusion, which prevents the teeth from fitting together correctly when you bite down. Your dentist can adjust the height of your filling so that you can bite down with comfort and ease.
Type of Filling

The type of filling your dentist used can also cause sensitivity or discomfort in the tooth. For example, sensitivity is fairly common when a composite resin material is used in the filling and may result from the filling shrinking slightly and creating a gap beneath it. There are many ways to cope with or eliminate sensitivity due to a composite filling, from using a different material or changing the method used to place the filling.
Galvanic Shock
Galvanic shock occurs when adjacent fillings composed of different metals (one of gold and the other made of amalgam) touch and produce an electric current; however, this situation is rare.
Exposed Pulp

If an inflamed nerve or an exposed pulp is behind your discomfort, your options might be to have a root canal or for the dentist to remove the damaged tooth and replace it with an implant or bridge.
Keep in mind that your new filling may also be aggravated by hot, cold or sweet food and beverages, as well as air and pressure from chewing. These sensitivities should subside in a week or two. If they don't, schedule a return visit to your dentist. They may refer you to a dental specialist known as an endodontist, a dental professional who specialises in identifying tooth pain, performing root canals, and most importantly, saving teeth. The endodontist may determine that your cavity was deeper than suspected and that the decay had gone into your tooth pulp. In that case, they will most likely perform a root canal. In South Africa, many general dentists can perform root canal procedures themselves, so referral to an endodontist may not be required.
What to Do About the Pain
The goal of getting a filling is to correct tooth cavities and ease any discomfort. But if it's been a week since your filling and you're still feeling pain when you bite down, eat, or even just open your mouth, you should schedule an appointment with your dentist as soon as possible. He or she will be able to pinpoint and correct the issue.
If you want to avoid cavities in the first place, be sure to follow a great oral care routine at home.
Brushing twice a day will strengthen your enamel and help prevent cavities.
Flossing daily will also help you prevent cavities and will keep your gums healthy.
Regular dental visits are important for spotting any problems before they need major treatments.
Preventive care is always best, but once you need a filing, seek your dentist's help to plan your next steps.
(11/26/2024)by Colgate
More Information: https://www.colgate.com/en-za/oral-health/fillings/tooth-pain-after-a-filling-is-it-normal
Views: 326
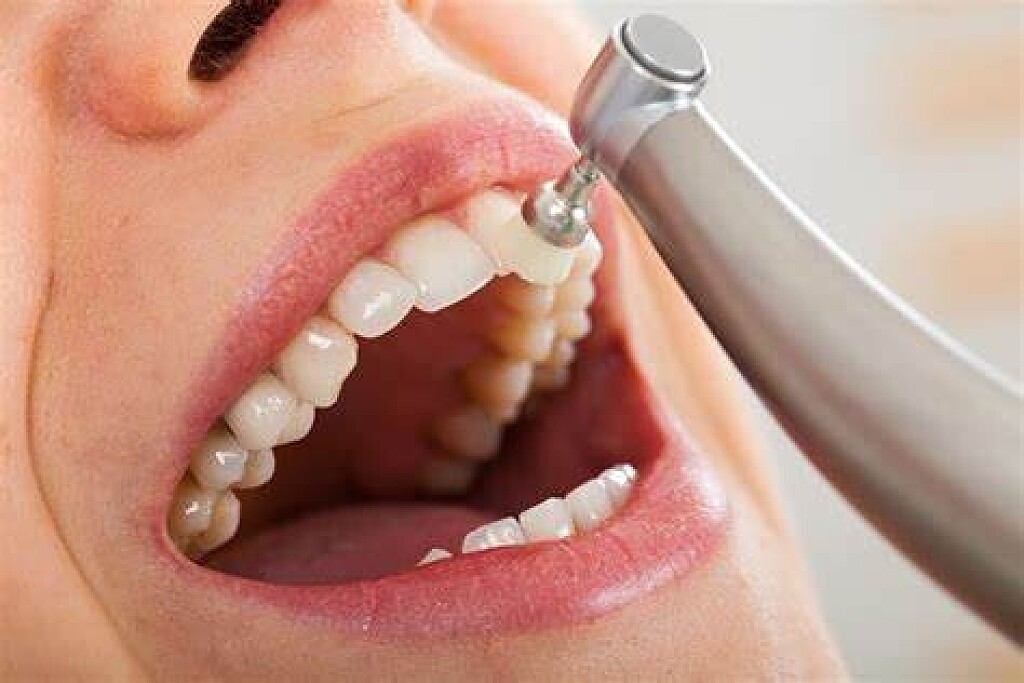
How Does A Tooth Polishing Procedure Work?
Smooth, shiny, stain-free teeth are a real confidence booster. One way to achieve a bright, attractive smile is through tooth polishing. Many dental practices offer polishing after a dental treatment or as the final stage of a routine dental visit. Dental hygienists generally perform this service in busy practices, but dentists may perform the polishing themselves in some practices.
Cleaning and Polishing Teeth
When layers of plaque build up on the teeth, they harden and form a tough mineral substance called tartar. Germs can live beneath tartar and cause dental problems. To help prevent this, dental hygienists remove tartar in a procedure called scaling. After scraping off the hard tartar with special instruments, the hygienist polishes the teeth. Dental polishing removes surface stains on the teeth and leaves them shiny and smooth, putting the finishing touches on a protective dental treatment.
Tooth Polishing Procedures

Tooth polishing is a painless dental procedure, and some patients enjoy it. The dental hygienist uses a small, soft rubber cup and polishing paste. If a patient has severe stains, an air polishing system may be used - this involves a jet of pressurised air and water mixed with an abrasive agent to polish the teeth. An article in the Journal of Indian Society of Periodontology (JISP) reports that some dental hygienists provide selective polishing, which means they only polish teeth that remain stained after scaling. Another option is therapeutic polishing, which helps remove germs from tooth roots that are exposed during dental surgery.
Tooth Polishing Pastes
Tooth polishing pastes are called prophy pastes, an abbreviation of prophylaxis that refers to the protective effects of tooth cleaning and polishing. Dental hygienists choose between fine, medium and coarse pastes to fill the rubber cup that delivers the paste to the tooth surface. Coarse and medium pastes are most effective at removing stains quickly, according to the American Academy for Oral Systemic Health, but they can also scratch and roughen the tooth enamel, thus making it more likely to develop stains at a later stage. Fine pastes are less damaging and create a more highly polished finish, but can be less effective at removing stains. The JISP states that the abrasive agents most often used in prophy are calcium carbonate and pumice flour.
Air Polishing for Teeth

Published by the Journal of Dental Hygiene, a review of several studies shows that polishing with a jet of air, water and an abrasive agent removes stains more effectively and quickly than polishing with a rubber cup and prophy. In addition, air polishing is generally less harsh on tooth enamel. Sodium bicarbonate is often used as the abrasive agent in air polishing, but glycine (a naturally occurring amino acid) is less abrasive and just as effective.
Tooth Polishing Precautions
If there is gum recession and the cementum is exposed, the use of a mild polishing paste may be recommended to ensure there is no sensitivity to the tooth surface. If patients have problems like teeth sensitivity, untreated cavities, exposed dentin or roots, and problematic or receding gums, these oral issues should be treated before the teeth are scaled and polished. Lastly, according to the Journal of Dental Hygiene, patients who should not have their teeth polished include the following: people suffering from respiratory problems, hypertension, conditions that weaken tooth enamel, or allergies to the abrasive agents.
Although tooth polishing is not an essential dental treatment, it can help patients feel confident about the look of their teeth and encourage good oral care habits. If your teeth have surface stains, ask your dentist whether polishing would help improve their appearance.
(11/26/2024)by Colgate
More Information: https://www.colgate.com/en-za/oral-health/dental-visits/how-does-a-tooth-polishing-procedure-work
Views: 440

